-
PDF
- Split View
-
Views
-
Cite
Cite
Tadashi Kamio, Manabu Kamio, Takashi Kamio, A rare case of successful staged surgery for giant coronary artery aneurysm, multiple artery aneurysms, and coronary-to-pulmonary artery fistula, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf154, https://doi.org/10.1093/jscr/rjaf154
Close - Share Icon Share
Abstract
Large coronary artery aneurysms (CAAs) with multiple arterial involvements are rare, and complications like coronary artery fistulae are extremely uncommon. Managing such cases presents a significant challenge. A 75-year-old female presented with a left inguinal mass and palpitations. Computed tomography revealed an abdominal aortic aneurysm and a left common iliac artery aneurysm. Coronary angiography identified a giant CAA and a coronary-to-pulmonary artery fistula. She underwent a two-stage surgical approach: first, an aortobiiliac Y-graft interposition, followed by open-heart surgery for aneurysmectomy and ligation of the pulmonary artery fistula 4 months later. Her postoperative course was uneventful, and she remained well at the 1-year follow-up. This case shows that prioritizing the aneurysm with the highest rupture risk, followed by staged treatment of CAAs, can lead to successful outcomes without major complications.
Introduction
A coronary artery aneurysm (CAA) is defined as a localized dilatation of the coronary artery measuring ≥1.5 times the diameter of the adjacent normal segment or the patient’s largest coronary vessel [1, 2]. The prevalence of CAAs detected by coronary angiography is reported to be 0.3%–5%; however, cases of rare CAAs accompanied by multiple aneurysms or fistulas are scarcely reported [3–5].
Coronary artery fistula aneurysms are thought to result from atherosclerotic changes superimposed on congenital fistulas, but such cases are extremely rare with unclear epidemiological data, and the optimal treatment approach for patients with multiple systemic aneurysms remains uncertain [6]. Primary strategies include stenting, surgical ligation of the aneurysm with distal bypass surgery, or conservative management with anticoagulation therapy [7]. However, due to the rarity of these cases, comprehensive data on perioperative complications and long-term outcomes are lacking.
Case presentation
A 75-year-old female presented to her primary care physician with complaints of a left inguinal mass and palpitations that had persisted for several months. Her medical history included hypertension, dyslipidaemia, and Mycobacterium avium complex pulmonary disease (MAC-PD). Computed tomography (CT) revealed an abdominal aortic aneurysm with a maximal diameter of 42 mm, as well as aneurysms in the right (maximum diameter of 57 mm) and left (maximum diameter of 30 mm) common iliac arteries (Fig. 1). In cases of bilateral common iliac artery aneurysms associated with an abdominal aortic aneurysm, management typically involves aorto-bilateral iliac or femoral artery grafting. Thus, open surgical repair was planned. Prior to repair of the aortic and iliac aneurysms, the patient underwent risk stratification and preoperative cardiac evaluation to minimize perioperative cardiac and pulmonary complications.
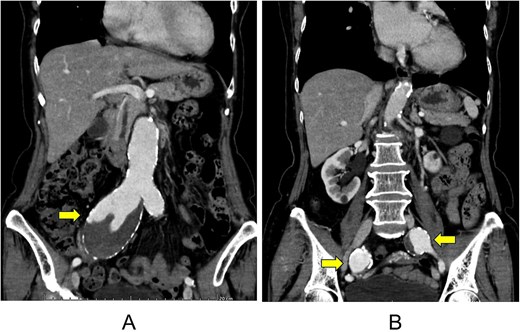
Computed tomography images of an abdominal aortic aneurysm (A) and multiple aneurysms of the right and left common iliac arteries (B).
Coronary angiography revealed a large CAA originating from the left anterior descending artery (LAD) and a vessel suggestive of a fistula from the LAD to the pulmonary artery (Fig. 2). Additional CT coronary angiography was performed to better define the anatomy prior to intervention. The length of the aneurysm was 15 mm, and the maximum diameter was 8.5 mm. Given the rarity of this case, three-dimensional (3D) reconstruction was performed using CT multiplanar reconstruction to assist with surgical planning, followed by the creation of a 3D-printed model of the anatomical structure (Fig. 3).
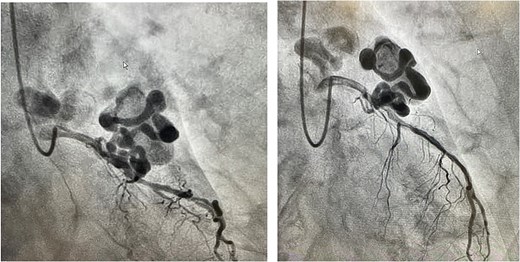
Coronary angiography findings of a large CAA originating from the left anterior descending artery.
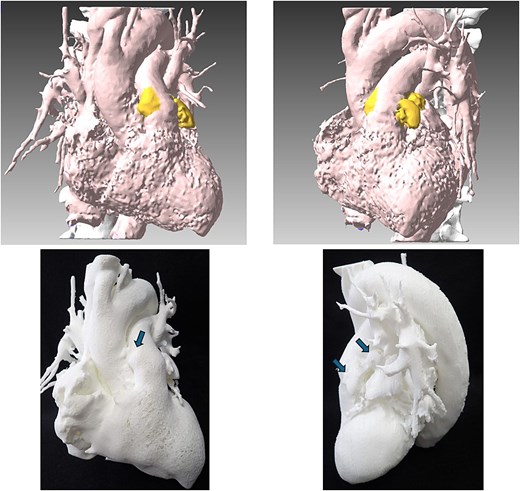
3D reconstructed images of the heart and 3D-printed anatomical structure.
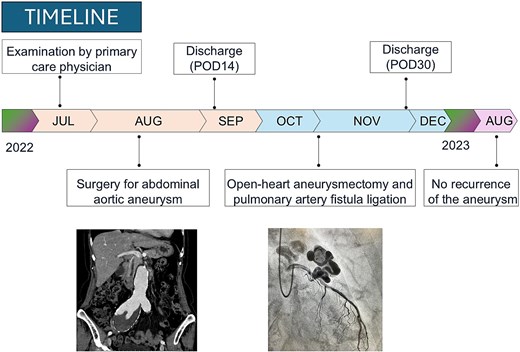
The patient presented at a multidisciplinary conference, where a two-stage surgical approach was recommended. The first stage involved addressing the abdominal aortic and bilateral iliac artery aneurysms, with surgical treatment of the giant CAA planned for a minimum of four months later. The patient provided informed consent and subsequently underwent successful repair with aortoiliac Y-graft interposition, followed by monitoring in the intensive care unit. The patient was discharged on the 14th postoperative day. Four months after discharge, she underwent open-heart aneurysmectomy and pulmonary artery fistula ligation, as her overall condition had improved sufficiently to allow for re-intervention.
Her postoperative recovery was uneventful, and no complications were observed during the 1-year follow-up period. CT performed 1 year post-procedure confirmed an excellent surgical outcome, with no evidence of new aneurysms (Fig. 4).
Discussion
Large CAAs accompanied by multiple arterial aneurysms are exceedingly rare. In the literature, the most common vascular aneurysm associated with CAAs is an abdominal aortic aneurysm, with a reported incidence of 52.6%, which aligns with our case [4]. CAAs have been described in various conditions, including Kawasaki disease, mycosis fungoides, Marfan syndrome, connective tissue diseases, and arteritis. However, atherosclerosis remains the most common cause of isolated CAAs. Giant CAA, defined as those with an internal diameter greater than 8 mm, carry a high risk of morbidity and mortality due to their potential for rupture, thrombosis, and embolization. Early detection and appropriate surgical intervention are crucial to preventing adverse outcomes. In our case, the patient had an aneurysm measuring 8.5 mm, placing her in the high-risk category. Despite the complexity of this case, we successfully performed abdominal graft replacement surgery. This staged approach, prioritizing the repair of the abdominal aortic aneurysm before addressing the CAA, proved to be effective in preventing rupture and improving patient outcomes.
Our patient had not only a large coronary aneurysm and multiple artery aneurysms, but also a coronary-pulmonary artery fistula. Most coronary artery fistulas are discovered incidentally during angiography for coronary vascular disorders, and in our case, it was discovered incidentally during a preoperative investigation [8]. Large coronary aneurysms with fistulas require early surgical resection, because rupture can cause cardiac tamponade or sudden death [9, 10]. According to past reports, coronary artery fistula aneurysms are more commonly observed in elderly individuals in their 70s and in women, with many cases reported in Asians, particularly Japanese [11]. The clinical features of the present case are consistent with these findings. Interestingly, a literature review revealed that there could be a connection between coronary artery fistulas and bronchiectasis, and the likelihood of a co-occurring coronary artery fistula and pulmonary-related disease was reported to be 33% [12, 13]. Considering that the current patient had underlying MAC-PD and CT scans revealed bronchiectasis, it is plausible that MAC-PD may have contributed to coronary artery fistula development.
Conclusion
Large CAAs with multiple arterial aneurysms are rare and challenging, but prioritizing high-risk aneurysms followed by staged CAA treatment can achieve successful outcomes without major complications.
Acknowledgements
I would like to express my deepest gratitude to the cardiac surgeons at Yokosuka Uwamachi Hospital for their exceptional work in successfully performing this remarkable surgery.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
None declared.
Ethical approval
As case report, no ethical approval was required. The patient signed the written informed consent for the publication of this case report study including all the images, available for reviewers. The authors confirm that written consent for the submission and publication of this case report, including images and associated text, was obtained from the patient in line with the CARE guidelines.



