-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel Medina, Veronica A Angos, Juan C Sinchi, Gabriel A Molina, Diana E Parrales, Mauricio R Heredia, Miguel J Ochoa-Andrade, Intraluminal migration of a gossypiboma, a rare complication of a problem we should never have to face, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf142, https://doi.org/10.1093/jscr/rjaf142
Close - Share Icon Share
Abstract
After surgery, forgetting instruments, gauze, surgical pads, cotton, or other surgical materials is a serious but avoidable complication. Symptoms are broad and will depend on the location of the gossypiboma and the body's reaction against it. Most will manifest either as an exudative inflammatory or fibrotic reaction. Intraluminal migration is relatively rare and, in most cases, will mimic symptoms of abdominal obstruction. We present the case of a healthy 25-year-old male. After an emergency surgery, a whole surgical pad was left inside his abdomen, which eroded its bowel wall and migrated into the lumen. After a thorough evaluation, surgery was decided, and the foreign body was extracted. On follow-up, the patient is doing well.
Introduction
Post-operative complications are bound to happen in any surgery, and although many will continue to happen, one should be completely avoidable [1]. One of these complications that appears due to a human error and which is frequently underreported is the retained foreign body, or gossypiboma [1, 2].
We present a case of a 25-year-old male. After an appendectomy, a surgical pad was forgotten in his abdomen. The surgical pad eroded the bowel wall and was found within its lumen.
Case report
The patient is an otherwise healthy 25-year-old male. He underwent emergency surgery due to acute appendicitis 5 months prior to his admission. He was told that due to the severity of his disease, the surgical team had to convert the approach from a laparoscopic to a conventional-open approach. Afterward, he recovered completely; nonetheless, two months after surgery, he started to experience abdominal pain in his lower left abdomen. At first, the pain was mild and was accompanied by nausea; nonetheless, as time passed, the pain became intolerable and was followed by severe episodes of vomiting and abdominal distension. Therefore, he was brought immediately by his family to the emergency room.
On examination, a tachycardic, febrile, and septic patient was encountered. He was not hypotensive; however, he was extremely dehydrated. His abdomen was distended with tenderness, but no masses were detected on clinical examination. Intravenous fluids were initiated, and complementary exams were requested.
Leucocytosis, with neutrophilia, along with an elevated C-reactive protein, was noticed, and due to his clinical findings, an acute abdomen due to adhesions was suspected. Therefore, an abdominal computed tomography (CT) was requested to have a surgical plan. To the surprise of the medical team, the CT unveiled severe dilation of loops of the small bowel and an intraluminal foreign body with tiny air bubbles containing a metallic marker suggestive of an intraluminal gossypiboma (Fig. 1A–C).
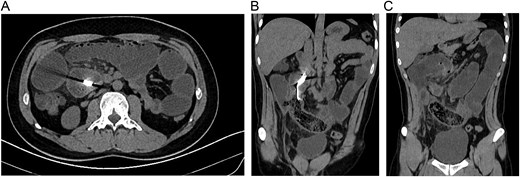
(A) CT, dilation of small bowel loops is seen with obstruction and a hyperdense image in the bowel. (B) CT, reveals a spongiform pattern of mixed mass with gas bubbles inside the intestine. (C) CT, reveals a spongiform pattern with dilated bowel.
Due to this, surgery was decided after obtaining consent.
At laparotomy, multiple adhesions were discovered between the loops of the small bowel, which were dissected with blunt dissection. After exposure, 50 cm away from the ileocecal valve, a 45 cm segment of the ileum was extremely dilated and congestive in its mesentery. Within the bowel, a foreign body was detected within its lumen. With these findings, a resection of the compromised bowel was decided, and a side-to-side anastomosis was completed with a mechanical stapler (Fig. 2A and B).
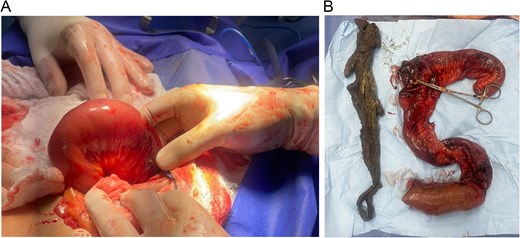
(A) Laparotomy, compromised bowel wall with the foreign body inside its lumen. (B) A whole surgical pad is found within the bowel.
A whole surgical pad was found within the lumen of the small bowel, completely obstructing the intestine. Abdominal obstruction due to intraluminal migration of a surgical pad was the final diagnosis.
His postoperative course was uneventful; he completely recovered after the surgery, but we were told that his legal team was contacting his previous surgeon due to our findings.
Discussion
Gossypiboma is derived from the Latin term `gossipium', which means cotton and the Kiswahili term `boma', which means concealment [1]. Gossypiboma occurs when a surgical material (sponges, towels, instruments, rubber tubes, etc.) is left inside a patient inadvertently after a surgical procedure; this is an extremely rare and regretful situation one would think should never happen; regretfully, it appears in one per 100–3000 to 5500–10 000 surgeries [1, 2]. This high variability is due to its medico-legal implications and fear of retaliation against the medical team; therefore, it is frequently underreported [1, 3].
Since it was first described by Wilson et al. in 1884, this retained surgical foreign body is an avoidable medical error [1, 2]. Nonetheless, it appears more often if there is an unplanned change in the operation, a high body mass index, or surgery is an emergency [2, 4]. The abdomen (56%) is the most affected location, followed by the thorax (11%) and pelvis (8%), yet any place could be affected, including the extremities or even the brain [3, 4]. In our case, the patient had emergency surgery and also a change in their original plan, which might have led to the gossypiboma.
Gossypiboma can appear in multiple clinical presentations, and symptoms will depend on the foreign body's location and the body's reactions against it [1, 5]. The most common is the transudative one, which occurs when there is a high antigenicity response that results in severe inflammation, adhesion formation, and abscess [5, 6]. Gossypiboma can also generate granuloma-like reactions that lead to adhesions and calcifications [7, 8]. Due to this, clinical presentation is highly variable, and patients may be asymptomatic for days or years [1, 7].
In other rare occasions, the foreign body will erode into the bowel wall and enter its lumen; afterward, the intestinal loop will close after the foreign body's migration [6, 7]. Peristaltic activity in the bowel will push the foreign body through the intestine until it reaches the ileum, which usually results in obstruction [6–8]. This complication can take weeks or years to occur, and on even rarer occasions, the foreign body can be expelled through the rectum [8]. Other complications include obstruction, peritonitis, adhesion, fistulas, and abscesses [1, 6]. As it happened in our patient.
Diagnosing gossypiboma is problematic because it is rare, and most are usually not suspected [2, 5]. Imaging is critical for diagnosis; X-rays can be helpful, but CT is the most effective approach to confirm the diagnosis and evaluate multiple difficulties [5]. The only treatment for gossypiboma is surgery through any approach with complete removal of the foreign body [1, 4]. However, it carries a high risk of reoperation, readmission, prolonged hospital stay, sepsis, and death [2, 6]. This is without mentioning the medico-legal implications that gossypiboma carries [1, 2, 5].
The surgical team must remain vigilant during every surgery, and a thorough count of all surgical materials at the end of every procedure is essential. Clear communication and prevention are the only ways to prevent this severe and avoidable complication.
Conclusion
The surgical team's performance and attention to the patient will define the patient's prognosis. We must remember that the patient trusts us, and we must always be alert to count all the surgical materials to avoid forgetting anything inside them.
Conflict of interest statement
None declared.
Funding
None declared.



