-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmad Al-Bitar, Mohammed Shwin, Incidental finding of metastatic mesothelioma in an inguinal hernia sac: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf099, https://doi.org/10.1093/jscr/rjaf099
Close - Share Icon Share
Abstract
Inguinal hernias are the most common type of abdominal wall hernias, often requiring surgical intervention. Mesothelioma, a rare cancer associated with the linings of serous cavities, can occasionally be found in hernia sacs. This paper presents the case of a 38-year-old male with an incidental diagnosis of stage 4 pleural mesothelioma discovered during a routine inguinal hernia repair. Despite being asymptomatic, the patient's hernia sac examination revealed mesothelioma, which was confirmed through histopathological analysis and imaging. This rare finding underscores the importance of thorough examination and comprehensive oncological evaluation when unusual findings are encountered during routine surgeries. The case highlights the necessity for awareness and vigilance in similar scenarios to potentially improve patient outcomes.
Introduction
Inguinal hernias, which occur when abdominal contents or preperitoneal fat protrude through the inguinal canal, are the most prevalent type of abdominal wall hernias, comprising 75% of cases [1].
The surgical correction of these hernias is a common elective procedure in surgical practice [2].
While various visceral organs can be found within an inguinal hernia, the intestine and omentum are the most frequently encountered [3].
Throughout a person's lifetime, approximately 7.3% of men will experience an inguinal hernia. These hernias are part of a broader category of defects in the parietal peritoneum that result in protrusions of the abdominal wall skin [4].
Mesothelioma, a rare cancer originating from the linings of serous cavities such as the pleura, peritoneum, and pericardium, can sometimes be associated with hernias [5].
In fact, for various gastrointestinal and gynecologic cancers, the initial symptom or sign may be a newly developed hernia caused by a tumor mass or malignant ascites [6].
Although uncommon, malignant epithelial tumors can be found within surgically removed hernia sacs, occurring in less than 0.5% of cases.
When cancer spreads within the abdominal and pelvic cavity as peritoneal metastases, it follows a specific pattern characteristic of the particular cancer type [6].
This paper presents a case of an asymptomatic male patient who underwent hernia sac repair, during which mesothelioma was incidentally discovered.
Case presentation
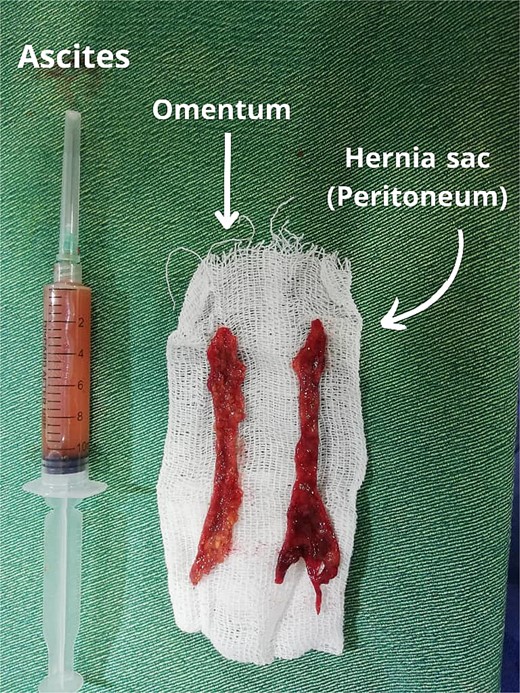
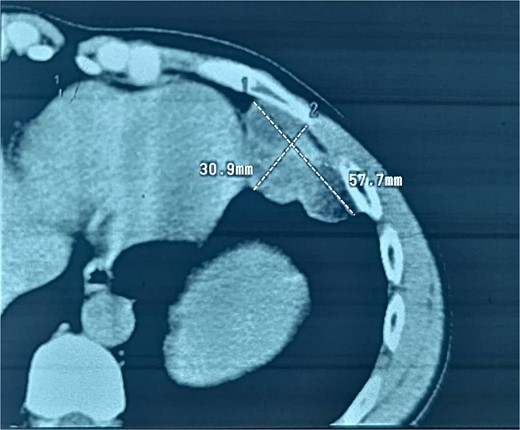
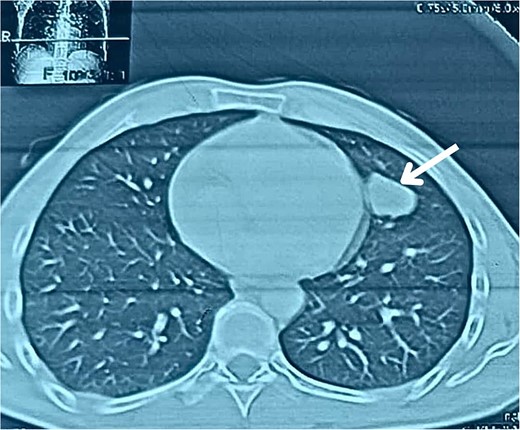
A 38-year-old male educator and part-time farmer with no notable cancer history in his family and a non-smoking background sought medical attention. His medical records included a left inguinal hernia repair two years prior and an ischemic stroke six years ago, for which he was undergoing ongoing treatment with clopidogrel, aspirin, and rosuvastatin. The patient reported swelling in the right inguinal region, without any other symptoms. The patient was prepared for surgery to repair the hernia. Upon opening the hernial sac, a thickened wall was observed. Aspiration was conducted to exclude bladder involvement, yielding cloudy, serous fluid indicative of ascites and omental thickening. Based on these observations, samples from the hernial sac wall (peritoneum), omentum, and ascitic fluid were submitted for histopathological analysis, and the hernia was repaired (Fig. 1). Peritoneal surgical biopsy showed that the peritoneal tissue fragments involved epithelioid cell malignant neoplasms with tubular and papillary formations and stromal infiltration. An IHC study revealed Calretinin and CK5/6 markers (mesothelial cell markers) were diffusely positive in the tumor, leading to a diagnosis of malignant mesothelioma. (Fig. 2 and 3) CEA levels were assessed and found to be within the normal limits. Contrast-enhanced computed tomography (CT) of the chest, abdomen, and pelvis revealed a 58 × 31 mm lobulated mass with multiple septate cavities in the lateral and basal pleura of the left lower lobe (Figs 4–6). The scan also showed thickening of the omentum, mesentery, and peritoneum, consistent with a left pleural mesothelioma with peritoneal and omental metastases. Oncologists diagnosed the patient with stage 4 pleural mesothelioma. The patient was determined to require oncological treatment consisting of eight cycles of cisplatin combined with gemcitabine. Unfortunately, the patient died during the fourth chemotherapy cycle.
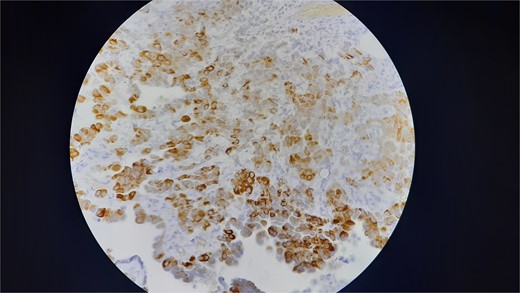
Shows that the neoplastic cells are strongly and diffusely positive for Ck5/6 (membranous and cytoplasmic staining).
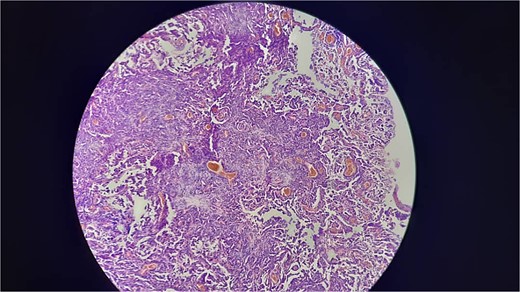
Shows that invasive proliferation of atypical mesothelial cells with large hyperchromatic nuclei with tubulpapillary and solid growth pattern.

Discussion
Malignant mesotheliomas are uncommon neoplasms of the pleura and peritoneum, typically linked to asbestos exposure. These tumors can develop in the mesothelial cell lining, including that of hernias. The outlook is grim, and they may be associated with inguinal or umbilical hernias [7].
The unexpected discovery of a malignant peritoneal mesothelioma (MPM) in an inguinal hernia sac is extremely rare, with the initial case documented in 1976 [8].
The incidental finding of mesothelioma in this patient underscores the need for thorough histopathological examination of hernia sacs, particularly in cases with unusual clinical features or presentations.
Research indicates that 85.5% of malignant mesotheliomas occur in the pleura, 13.2% in the peritoneum, 0.8% in the pericardium, and 0.5% in the testicular tunica vaginalis [9].
Malignant mesotheliomas of the tunica vaginalis are exceptionally uncommon, with a recent study noting only five instances. While asbestos exposure is linked to most peritoneal mesotheliomas, it is not the cause in all cases. Four out of five patients with tunica vaginalis mesotheliomas had a history of asbestos exposure [10].
The identification of mesothelioma in this scenario not only enhances our comprehension of its possible manifestations but also underscores the importance of collaboration between surgeons and pathologists.
Histologically, malignant mesothelioma is categorized into three types: epithelioid, sarcomatoid, and biphasic. For pleural mesothelioma, the frequencies of these types, along with cases of unknown classification, were reported as 53.6%, 23.3%, 18.3%, and 4.8%, respectively [9].
Acherman et al. reported that among 51 cases of malignant peritoneal mesothelioma, primary symptoms included abdominal pain (33%), abdominal pain and distention (10%), abdominal swelling (31%), and new hernias (12%). Of these hernias, five were inguinal and one was umbilical. Although umbilical hernias are infrequent, a newly developed abdominal hernia should be considered a potential primary symptom of malignant peritoneal mesothelioma [11].
In male patients with malignant peritoneal mesothelioma, 17% were diagnosed due to a new inguinal hernia, compared to 5% of female patients [12].
The oncology literature contains several reports of peritoneal metastases becoming symptomatic within hernia sacs [13].
Developing a treatment plan for these patients is challenging due to the scarcity of such cases [14].
Generally, treatment outcomes are poor. Chemotherapy appears to be the only relatively successful treatment, particularly when combined with debulking procedures [15].
Further studies are warranted to explore the pathophysiological link between hernias and the development of mesothelioma, which may provide insights into its etiology and potential preventive measures.
This case contributes to the limited body of literature on the association between mesotheliomas and hernias, suggesting that vigilance in similar scenarios could potentially improve patient outcomes.
Conflict of interest statement
The authors have no conflict of interest.
Funding
None declared.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Author’s declaration
None of the authors listed on the manuscript are employed by a government agency that has a primary function other than research and/or education. Moreover, none of the authors are submitting this manuscript as an official representative or on behalf of the government.
Ethics statement
The manuscript was approved by ethics committee.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient-consent policy.



