-
PDF
- Split View
-
Views
-
Cite
Cite
Alwaleed Al-Dairy, Ahmad Al-Bitar, Surgical management of recurrent subaortic stenosis: a case report of the modified Konno operation, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf100, https://doi.org/10.1093/jscr/rjaf100
Close - Share Icon Share
Abstract
Subaortic stenosis (SAS) is a rare congenital heart defect (CHD), accounting for 1%–2% of all CHD and the second most common type of left ventricular outflow tract (LVOT) obstruction. SAS ranges from localized obstructive membranes to complex tunnel narrowing and often coexists with other CHD like ventricular septal defect, interrupted aortic arch, and aortic coarctation. Despite generally successful surgeries, SAS recurs in 5%–30% of patients, necessitating reoperation. Recurrence factors include younger age at initial surgery, higher preoperative LVOT gradients, and complex anatomical presentations. This report discusses an 11-year-old girl with recurrent SAS who underwent a modified Konno operation. It emphasizes the need for meticulous surgical technique and vigilant postoperative follow-up to manage SAS and reduce recurrence risk effectively. The case highlights the challenges of this CHD and underscores the importance of personalized, comprehensive care strategies.
Introduction
Subaortic stenosis (SAS) is a rare congenital heart defect (CHD), accounting for 1%–2% of all CHDs, and represents the second most common type of left ventricular outflow tract (LVOT) obstruction [1–4]. SAS is considered a spectrum lesion, ranging from a localized obstructive membrane (in up to 70% of cases) to complex tunnel narrowing of the LVOT [4, 5]. In 50%–60% of cases, SAS is associated with other CHDs such as ventricular septal defect, interrupted aortic arch, and coarctation of the aorta [5–7]. Despite satisfactory surgical outcomes for SAS repair, recurrence is common, with 5%–30% of patients requiring reoperation. Although many factors have been reported to be associated with a higher recurrence rate—such as younger age at initial surgical intervention, higher preoperative peak LVOT gradient, and tunnel-type stenosis—the insufficient relief of the obstruction at the initial operation may be considered the most important factor. Herein, we report a case of an 11-year-old patient with recurrent subaortic stenosis who underwent the modified Konno operation (MKO).
Case presentation
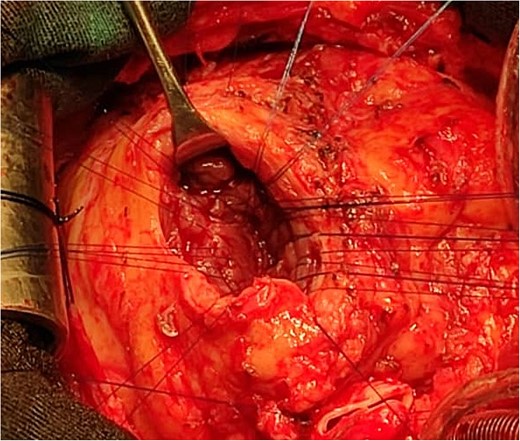
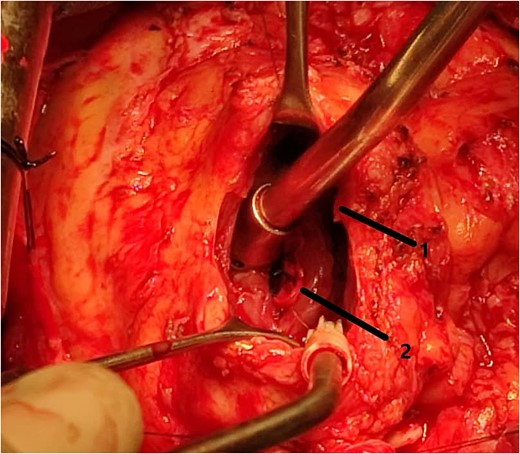
An 11-year-old girl was referred to our hospital with a main complaint of progressive exertional dyspnea. She had undergone surgical repair of SAS 6 years ago. Transthoracic echocardiogram (TTE) revealed the following findings: severe left ventricular hypertrophy, tunnel-like fibromembranous subaortic stenosis with a length of 10 mm, a peak gradient (PG) across the LVOT of 170 mmHg, and mild aortic regurgitation. Based on these findings, the patient was scheduled for elective surgical repair with a possible indication for MKO. The operation was performed via median sternotomy with great caution to avoid inadvertent rupture of any cardiac cavity due to heavy adhesions from the previous operation. The aorta was cannulated just below the takeoff of the innominate artery. Bicaval cannulation was performed to provide a bloodless field. Aortic cross-clamping was applied, and antegrade cold blood cardioplegic solution was administered via a catheter placed in the ascending aorta. The ascending aorta was opened transversely 1 cm above the sinotubular junction (Fig. 1). The aortic valve leaflets were examined carefully to confirm that the aortic valve could be preserved. LVOT was examined thoroughly, and it was clear that the stenosis in the subaortic area was so complex that simple resection through the aortic valve orifice would not be sufficient. The right ventricular outflow tract was opened transversely below the pulmonary valve. The conal papillary muscle was identified (Fig. 2). A right-angle instrument was introduced through the aortic orifice into the interventricular septum, and the tip of the instrument was used to perforate the conal septum to the left of the conal papillary muscle to prevent damage to the conduction system; the septal incision was completed with great caution to avoid damage to the aortic cusps and to extend the incision downward as necessary to completely relieve the stenotic subaortic area (Fig. 3). Interrupted 5/0 Prolene sutures were placed circumferentially around the septal incision to close the interventricular septal defect using a bovine pericardial patch to provide adequate widening of LVOT (Fig. 4). The right ventriculotomy was closed with a second bovine pericardial patch to avoid any possible obstruction of the right ventricular outflow tract (Fig. 5). The remainder of the operation was completed uneventfully. After 6 hours of mechanical ventilation, the patient was extubated, and she convalesced well postoperatively. TTE showed excellent results of the operation with PG across LVOT of 20 mmHg. On 1 year follow-up, the patient was asymptomatic and in very good general condition, and TTE findings confirmed the excellent result.
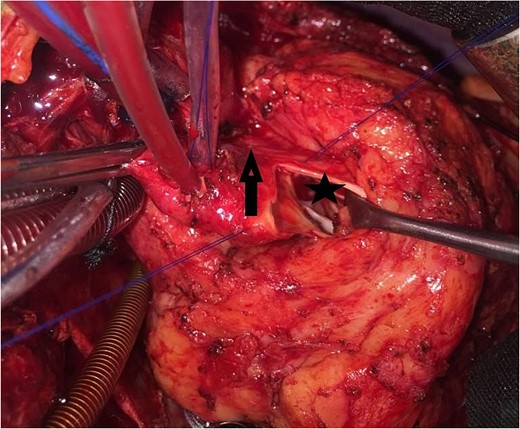
Intraoperative image showing the opened aorta. The arrow points to the aortotomy, and the star points to the stenotic left ventricular outflow tract through the aortic orifice.
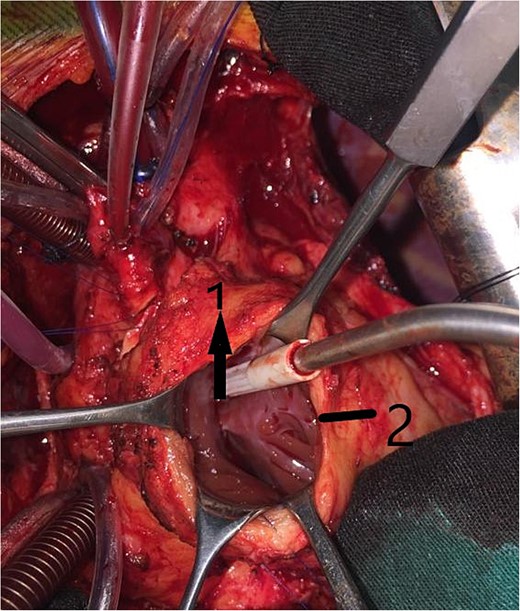
Intraoperative image showing the right ventriculotomy (2) and the conal papillary muscle (1).
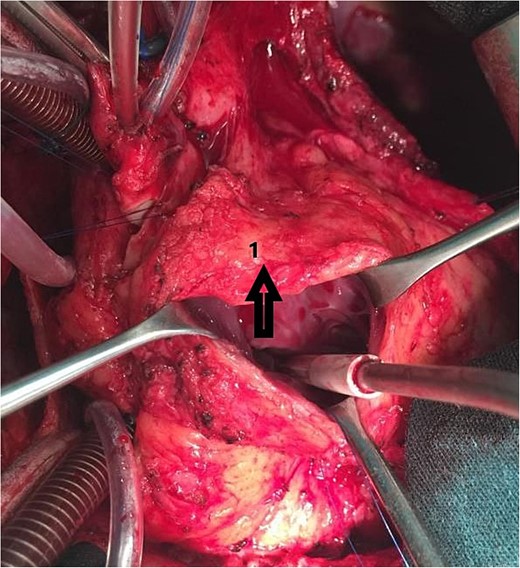
Intraoperative image showing the interrupted sutures placed around the septal incision.
Intraoperative image showing the bovine pericardial patch used to close the septal incision. (1) Right ventriculotomy and (2) bovine pericardial patch.
Discussion
SAS is the second most common type of congenital LVOT obstruction. It has a progressive nature, and its rate of progression is unpredictable in children [1, 7, 8]. Recently, it has been reported that SAS may be considered an acquired lesion, as its development may be attributed to hemodynamic abnormalities caused by abnormal left ventricular geometry [5–8]. Most patients are asymptomatic and are usually revealed by auscultation of a systolic ejection murmur. When symptoms are present, they include exertional dyspnea (the most common symptom in 40% of cases), chest pain, syncope, and rarely heart failure [1, 5]. Recurrence is common after surgical repair of SAS, and the most important factors that increase the rate of recurrence include: younger age at diagnosis and initial surgical intervention, higher preoperative peak LVOT gradient before surgery, smaller aortic annulus, tunnel-like type, as well as surgical technique and insufficient relief of the obstruction [8]. The reintervention rate doubles with every 10 mm Hg increase in preoperative PK; on the other hand, it decreases by 14% for every additional 6 months of age [7]. In our patient, we attribute the recurrence to tunnel-type stenosis and insufficient excision during the initial surgery. Herein, we emphasize the importance of adequate surgical repair of SAS at the first operation. Regarding MKO, it is of great importance to perform the septal incision quite to the left of the conal papillary muscle to avoid possible injury to the conduction system.
Conclusion
In conclusion, SAS presents as a rare but significant CHD that commonly recurs after initial surgical repair, necessitating careful long-term management. Our case highlights the complexity and challenges associated with SAS, particularly in tunnel-type stenosis and in situations where initial surgical relief is insufficient. This case underscores the importance of comprehensive surgical approaches and vigilant postoperative monitoring to optimize outcomes for patients with SAS.
Conflict of interest statement
The authors have no conflict of interest. None of the authors listed in the manuscript are employed by a government agency that has a primary function other than research and/or education. Moreover, none of the authors are submitting this manuscript as an official representative or on behalf of the government.
Funding
There are no funding resources for writing this manuscript.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
- aortic coarctation
- left ventricular outflow obstruction
- interrupted aortic arch
- subaortic stenosis
- congenital heart defects
- ventricular septal defect
- follow-up
- tissue membrane
- preoperative care
- repeat surgery
- surgical procedures, operative
- wakefulness
- left ventricular outflow tract gradient
- recurrence risk
- left ventricular outflow tract



