-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroki Nakahara, Shunsuke Doi, Satoshi Yasuda, Minako Nagai, Kota Nakamura, Yasuko Matsuo, Taichi Terai, Yuichiro Kohara, Takeshi Sakata, Masayuki Sho, Small bowel perforation caused by a fish bone in a patient with vascular Ehlers-Danlos syndrome: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf098, https://doi.org/10.1093/jscr/rjaf098
Close - Share Icon Share
Abstract
Management of gastrointestinal perforation in patients with vascular Ehlers-Danlos syndrome (vEDS) is clinically challenging. A male in his 40s with vEDS presented with right lower abdominal pain. Computed tomography revealed a foreign body in the ileum with bowel perforation. A detailed inquiry revealed that he had consumed codfish six days prior. Based on these findings, he was diagnosed with a small bowel perforation caused by a fish bone. Emergency laparotomy was performed and intraoperative findings showed a fish bone in the ileum penetrating the mesentery. We resected ~5 cm of the small intestine, including the perforation site. Although the patient experienced postoperative paralytic ileus, he was discharged on postoperative Day 27. Gastrointestinal perforation caused by fish bones in patients with vEDS is extremely rare and requires careful assessment to determine the appropriate treatment. For surgeons, an individualized surgical strategy and optimal perioperative management are important to prevent fatal complications.
Introduction
Ehlers-Danlos syndrome (EDS) is a heterogeneous group of inherited connective tissue disorders and the global prevalence is estimated to range from 1 in 5000 to 1 in 100 000 individuals. [1, 2] Vascular EDS (vEDS), also known as type IV, is particularly rare, accounting for <5% of all EDS cases. It is the most severe subtype due to its strong association with arterial ruptures and spontaneous gastrointestinal perforations, leading a median life expectancy of 48 years [3]. Surgical intervention is indicated for vEDS patients with gastrointestinal perforation; however, postoperative outcomes are poor due to severe complications arising from tissue fragility [4]. Therefore, management of gastrointestinal perforation in patients with vEDS is clinically challenging.
Herein, we present an extremely rare case of small bowel perforation caused by a fish bone in a patient with vEDS.
Case report
A male in his 40s was diagnosed with vEDS 5 years ago and has been followed up at our internal medicine department. His medical history included spontaneous mesenteric artery rupture and sigmoid colon perforation, for which he underwent two laparotomies. He presented to our hospital with a chief complaint of right lower abdominal pain. Physical examination revealed tenderness in the right lower abdomen without signs of peritoneal irritation. Laboratory tests showed slightly elevated inflammatory markers as follows: white blood cell count: 8000/μl, C-reactive protein: 6.51 mg/dl. Contrast-enhanced computed tomography revealed a foreign body in the ileum with bowel perforation (Fig. 1). Free air was localized in the mesentery and no abscess formation was observed. A detailed inquiry into the onset of abdominal pain revealed that he had consumed codfish 6 days prior. Based on these findings, the patient was diagnosed with a small bowel perforation caused by a fish bone. Although surgery for a patient with vEDS involves the risk of fatal complications, emergency laparotomy was performed due to the potential for injury to other organs or blood vessels and the risk of peritonitis from the migration of the fish bone. Intraoperative findings showed severe adhesions of the small intestine and a sharp 4 cm foreign body (fish bone) located 15 cm proximal to the terminal ileum penetrating the mesentery through the ileal wall (Fig. 2). We removed the foreign body and confirmed that it is a fish bone (Fig. 3). We resected ~5 cm of the small intestine, including the perforation site, and performed a stapled anastomosis. The patient developed postoperative paralytic ileus, which improved with conservative treatment using a nasogastric tube, and he was discharged on postoperative Day 27.
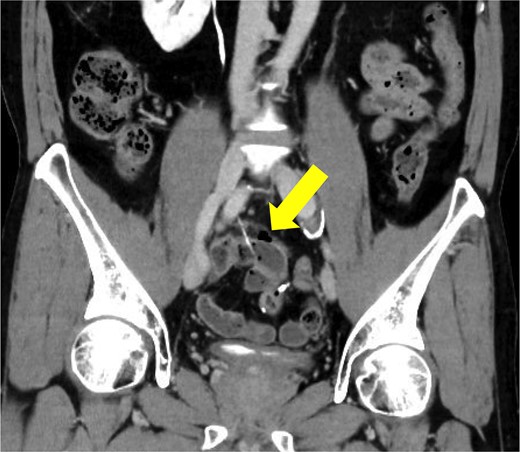
Contrast-enhanced computed tomography before surgery. A sharp foreign body with bowel perforation was identified in the ileum. Free air was localized in the mesentery and no abscess formation was observed.

Intraoperative findings. Severe adhesions of the small intestine were observed and a sharp 4 cm foreign body was located 15 cm proximal to the terminal ileum penetrating the mesentery through the ileal wall (arrow).
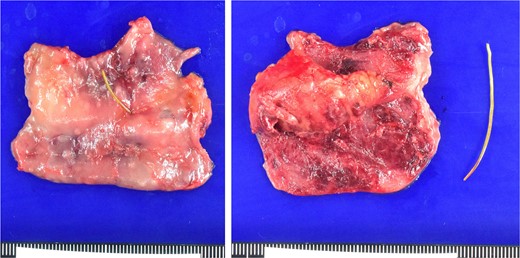
Macroscopical findings. Approximately 5 cm of the small intestine, including the perforation site, was resected. The foreign body was confirmed to be a fish bone.
Discussion
Accidental fish bone ingestion is common, but gastrointestinal perforation from fish bones is rare, with an incidence of < 1% [5]. However, fish bones are the most frequent cause of gastrointestinal perforation from foreign body ingestion [6]. Conservative treatment, including endoscopic removal, bowel rest, and antibiotic therapy can be appropriate for small perforations without evidence of free air, abscess formation, or systemic instability [7, 8]. However, surgical intervention is necessary when free air, signs of peritonitis, or clinical deterioration are present [9]. Therefore, a comprehensive assessment is essential to determine whether conservative treatment or surgical intervention is warranted for gastrointestinal perforation caused by a fish bone. To the best of our knowledge, this is the first reported case of small bowel perforation caused by fish bone in a patient with vEDS. Patients with vEDS are at high risk for fatal postoperative complications due to their tissue fragility and poor wound healing; therefore, more cautious management of gastrointestinal perforation is required.
In this case, the patient had a history of two laparotomies, and small bowel adhesions and angulation may have contributed to the fish bone perforation. Given the high risk of postoperative complications and mortality in patients with vEDS, conservative treatment may be preferable when feasible [10]. Endoscopic removal was considered in this case; however, it was deemed difficult due to the distance from the terminal ileum and the presence of small bowel adhesions. Additionally, patients with vEDS are reported to be at high risk for endoscopy-related perforation, with an incidence rate of ~10% [11]. Therefore, considering the risk of secondary complications from fish bone migration, such as abscess formation, peritonitis, and bleeding, we selected surgical intervention. Previous studies have reported an anastomotic leakage rate of up to 55% after colon perforation in patients with vEDS, supporting the recommendation for stoma creation [12]. However, small bowel perforation in vEDS is rare, and appropriate surgical procedures remain unclear due to a lack of evidence. In this case, since abscess formation around the perforation site, and bowel edema was not observed, we performed bowel anastomosis. As a result, although the patient experienced paralytic ileus, no anastomotic leakage occurred, and he was discharged without any fatal complications. Nevertheless, creating a small intestinal stoma may be necessary in some cases to prevent anastomotic leakage, depending on intraoperative findings. Therefore, an individualized surgical strategy is essential for managing small bowel perforations in patients with vEDS.
To avoid postoperative severe complications and mortality, postoperative management is also crucial. Particularly, patients with vEDS may develop vascular complications postoperatively, necessitating careful attention. Several cases have been reported in which arterial rupture occurred early after surgery for gastrointestinal perforation in patients with vEDS [13, 14]. Although no definitive treatment for vEDS has been established, β-blockers such as celiprolol are recommended to prevent arterial complications [15]. Additionally, strict blood pressure management is crucial, particularly in the postoperative period. In this case, systolic blood pressure was strictly controlled at ~100 mmHg with a combination of celiprolol, a calcium channel blocker, and an angiotensin receptor blocker. Moreover, appropriate analgesics were administered to prevent blood pressure elevation due to wound pain. Consequently, meticulous postoperative blood pressure management successfully prevented vascular complications.
In conclusion, gastrointestinal perforation caused by fish bones in patients with vEDS is extremely rare and requires careful assessment to determine whether conservative treatment or surgical intervention is appropriate. For surgeons, an individualized surgical strategy and optimal perioperative management are important to prevent fatal complications associated with tissue fragility.
Conflict of interest statement
The authors declare no conflicts of interests.
Funding
None declared.



