-
PDF
- Split View
-
Views
-
Cite
Cite
Domagoj Eljuga, Rhea Marie Muzar, Josip Jaman, Ksenija Eljuga, Goranka Rafaj, Zlatko Vlajcic, TDAP flap in reconstruction of a severe postburn contracture of the axillary region—a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf080, https://doi.org/10.1093/jscr/rjaf080
Close - Share Icon Share
Abstract
Herein we report a case of a male patient who was burned with hot oil and as a consequence developed a severe axillary contracture with limited abduction and elevation of his left arm. Due to the restriction in the range of movements, our patient reported limitations in everyday activities with decreased quality of life. For this patient we proposed a reconstructive plan that required a combination of multiple techniques of scar release and reconstruction of the defect with thoracodorsal artery perforator (TDAP)-based flap. One year postoperatively, we achieved a significant improvement in range of motion. We showed that TDAP flap provides a thin and pliable tissue coverage with a safe vascular supply. Furthermore, we eliminated the need for prolonged splinting which enabled early postoperative rehabilitation. To conclude, TDAP flap proved to be an ideal flap for this scenario and when used in combination with other techniques, optimal end result can be achieved.
Introduction
Postburn contractures in the axillar region can lead to a significant limitation in range of motion of the upper limb and thereby pose a huge burden in quality of life. The aim of surgical treatment is to restore the function of the shoulder with minimal or no local anatomic distortion and to improve, if possible, esthetic outcomes.
Case report
A 38-year-old male patient was admitted to Department of Plastic and Reconstructive surgery in a hospital for surgical treatment of a motion limiting postburn contracture in the axillar region. The initial injury caused by hot oil was managed a year prior to this procedure when split-thickness skin grafting was used. He presented to us with a severe shoulder contracture due to scar tissue over the entire right shoulder and scapular region (Fig. 1). Abduction and elevation were limited to a maximum of 70°; according to Kurtzman and Stern, the axillary contracture of our patient was classified as type Ib [1]. The patient was otherwise healthy non-smoker, working as a professional truck driver. Due to the functional restriction of his injury, he could not return to his work environment.

Our proposed reconstructive plan incorporated usage of a thoracodorsal artery perforator (TDAP)-based flap, performance of a Z-plasty as well as coverage of the donor site defect using split thickness skin grafts. Preoperatively marking of the perforator vessel was made by Doppler ultrasound.
Operative technique
Intraoperative position of the patient was on his left side with abducted shoulder.
First step consisted of an excision of the contracting scar tissue and additional release using a multiple Z-plasty. The remaining defect to be reconstructed with the fasciocutaneous flap reached from the posterior axillary line to the lateral margin of the scapula. Therefore, we continued with an incision at the anterior border of the latissimus dorsi muscle; after detection of the dominant septocutaneous branch of the thoracodorsal artery, the perforator vessel was dissected for ~10 cm in length, the cutaneous and intramuscular branches in its course were ligated. Care was taken to preserve the accompanying neurovascular bundles. Flap elevation was performed from ventral to dorsal. Its transposition was made by rotation of ~90° with minimal tension on the pedicle. The flap was than fitted in the defect area and fixated. At the end of procedure, the flap was vital and there were no signs of venous congestion.
Donor site defect was partially covered with a split-thickness skin graft taken from the femoral region.
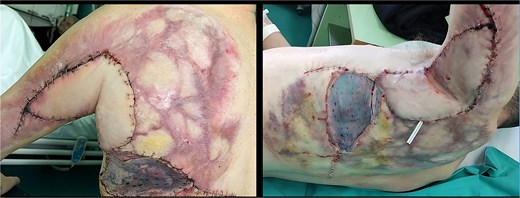
The early postoperative period was uneventful (Fig. 2). Three days postoperatively physical therapy was initiated; the patient was discharged 10 days after surgery. One month postoperatively a significant improvement in range of motion, with full abduction range and elevation up to 120° was accomplished (Fig. 3). In 1-year follow-up period, our patient presented to us with range of movement of 170° elevation, without any pain and fully functioning in work and social life (Fig. 4).


Discussion
Burn injuries can cause restrictions in range of movement especially if neck, wrist, or shoulder area is affected. It has been documented that this group of patients experience reduced quality of life, particularly 1 year after burn injury when most of the contractures will be permanent [2]. In extensive axillary contractures, often a combination of multiple techniques of release is required concerning the pattern of the scar and the condition of the surrounding tissue. With perforator flaps, there are numerous possibilities in flap design which provide improved function and appearance of the recipient site, thereby causing minimal damage of the donor site [3, 4].
The TDAP-based flap is a fasciocutaneous flap which represents a good option for severe axillary contractures where surrounding skin is not available for any local flaps or the use of local flaps would result in incomplete contracture release.
The TDAP was firstly introduced in 1995 by Angrigiani as a fasciocutaneous flap based on a perforating cutaneous branch of the thoracodorsal artery which by itself is a terminal branch of the subscapular artery. Important advantage of the TDAP is that muscle strength of the latissimus dorsi muscle is not affected as the flap does not integrate muscle tissue [5].
The flap can be planned either as a free flap or a pedicled one. Longitudinal axis can be designed in all directions thereby offering a broad range of movement based on the defect and desired final scar location. Dimensions up to 15 × 25 cm have been documented with pedicle length up to 20 cm [5, 6]. The cutaneous perforators are mostly found on the lateral border of the latissimus dorsi muscle. It is recommended to detect them preoperatively using color Doppler ultrasound [7]. Indication for the TDAP flap is very versatile and has been used as a free flap for various reconstructive needs throughout the body. When used as pedicled flap, it is very suitable for partial breast reconstructions. In axillary region, when surgical treatment is indicated for cases of hidradenitis suppurativa, it proved to be a reliable flap [4, 8]. For postburn contractures in axillary region, Jiang et al. showed good results in their series of patients for unilateral and bilateral cases of postburn contractures. They also showed a possibility of thining the flap if indicated [9].
With this case report, we showed satisfactory results in reconstruction of the axillary region using the TDAP flap which offers a non-bulky coverage in soft tissue repairs with minimal donor site morbidity and hidden scars—overall leading to a satisfactory functional and esthetic results for the patient.
Conflict of interest statement
None declared.
Funding
None declared.



