-
PDF
- Split View
-
Views
-
Cite
Cite
Phuc H Le, Tien N Tran, Nguyen Phung, Nhan N T Le, Surgical management of bilateral axillary severe hidradenitis suppurativa with thoracodorsal artery perforator V-Y advancement flaps: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf061, https://doi.org/10.1093/jscr/rjaf061
Close - Share Icon Share
Abstract
Hidradenitis suppurativa (HS) is a chronic inflammatory disorder caused by follicular occlusion and rupture, leading to recurrent abscesses and dermal destruction. Severe cases, classified as Hurley Stage III, often require surgical intervention. This report presents a 27-year-old male with bilateral axillary Stage III HS persisting for 2 years. Despite a 10-week Adalimumab regimen, recurrent lesions necessitated surgical excision with bilateral thoracodorsal artery perforator (TDAP) V-Y advancement flaps. The patient exhibited successful wound healing and cicatrization and preserved functionality postoperatively. TDAP flaps present several advantages over skin grafts, including reliable vascularity, minimal donor site morbidity, and improved aesthetic results. This case demonstrates the effectiveness of TDAP V-Y advancement flaps in reconstructing axillary defects, significantly reducing the risk of recurrence. The patient’s positive recovery and absence of procedure-related complications show that TDAP V-Y advancement flaps offer a superior, functional, and aesthetically pleasing option for managing severe HS.
Introduction
Hidradenitis suppurativa (HS) is a chronic, inflammatory hair follicle disorder characterized by painful, recurrent abscesses, sinus tract formation, and scarring, primarily in intertriginous areas. Its pathogenesis involves follicular occlusion and rupture, leading to an exaggerated immune response [1]. HS significantly impairs quality of life due to pain, malodor, and drainage, especially in severe stages (Hurley stage III), where diffuse involvement with multiple interconnected tracts dominates. Wide surgical excision and reconstructive techniques are pivotal for refractory cases, ensuring durable outcomes and functional restoration [2].
Case report
A 27-year-old male presented with a 2-year history of recurrent, painful axillary swellings, progressively worsening despite prior treatment. Clinical examination revealed discharging sinuses, hypertrophic scars, and erythematous nodules bilaterally, severely impairing his quality of life, as evidenced by a Dermatology Life Quality Index (DLQI) score of 22. His body mass index (BMI) was 28 (height: 170 cm, weight: 80 kg), a recognized risk factor for HS. Cultures of purulent discharge were sterile, consistent with the sterile nature of sinus tract contents in HS. The patient was diagnosed with Hurley stage III HS based on clinical findings.
Initial medical management included a 10-week course of clindamycin and adalimumab, which failed to achieve symptom resolution. Given the persistence of symptoms, surgical intervention was deemed necessary. The procedure involved bilateral wide excision of affected tissue with immediate defect reconstruction using thoracodorsal artery perforator (TDAP) flaps in a single operation.
Under general anesthesia, the patient was placed supine with bilateral arm abduction at 100°. On each side, two to three perforators along the anterior border of the latissimus dorsi were located with a handheld Doppler device. The vascular territory targeted for the flap design extended from the third rib superiorly to the seventh rib inferiorly, with the lateral scapular border posteriorly and the mid-axillary line anteriorly. Based on the perforators of the thoracodorsal vessels, a V-Y advancement flap was planned.
All hair-bearing skin within the axillary region was excised to the axillary vessels, completely removing diseased tissue. The flap dissection commenced with a subfascial approach along the anterior margin, followed by careful superior and posterior border elevation. Once the flap was islanded, it was advanced subcutaneously using a V-Y translation technique without the need for further isolation of the perforators, as the flap’s inherent mobility was sufficient to close the primary defect effectively (Fig. 1). Secondary defects were closed first, followed by inset of the flap using absorbable subcutaneous and subcuticular sutures. A single drain was placed posteriorly on each side. The TDAP flaps provided robust coverage while preserving axillary contour and full range of motion, with minimal donor site morbidity. The patient had an uneventful postoperative recovery and achieved complete resolution of symptoms with no recurrence over a 3-year follow-up period. Postoperative photographs demonstrated excellent aesthetic and functional outcomes, maintaining the axillary contour and flexibility required for optimal arm movement (Fig. 2).
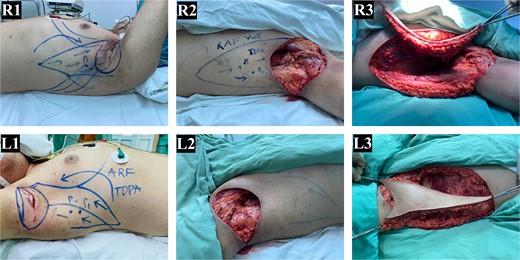
Bilateral stage III axillary HS and TDAP flap reconstruction. (R1-L1) preoperative image showing bilateral axillary HS and the freestyle V-Y advancement flap design based on the musculocutaneous perforators of the thoracodorsal artery. (R2-L2) post-excision of all hair-bearing axillary skin, revealing the axillary defect. (R3-L3) intraoperative movement of the TDAP flaps for defect closure (R: Right, L: Left).

TDAP flap closure and postoperative outcomes. (R1-L1) intraoperative closure of the axillary defect with TDAP flaps. (R2-L2) healed flap wound with a fully functional range of motion of the shoulder, observed at 2 weeks postoperatively. (R3-L3) follow-up at 3 years demonstrating successful healing and sustained functional outcomes (R: Right, L: Left).
Discussion and review of the literature
Pathophysiology and diagnosis
HS results from complex genetic, environmental, and immunologic factors interplay. Affected individuals often have a family history (33%–40%), and mutations in the gamma-secretase/Notch signaling pathway are implicated in some familial cases [3]. Obesity and smoking exacerbate the condition by increasing skin friction, sweat retention, and inflammatory responses. HS predominantly affects women, with peak onset between puberty and menopause, and fluctuates with hormonal cycles. Diagnosis is clinical, often using the Hurley classification system to stratify disease severity and guide [2, 4].
Surgical indications and options
Surgery is indicated for Hurley stage III HS or resistant stage II cases unresponsive to medical therapy. Surgical options vary, from local procedures like deroofing and laser therapy to extensive wide excisions [5, 6]. While deroofing offers temporary relief, it is unsuitable for diffuse disease. Wide excision, involving resection of affected tissue with safe margins, is the gold standard for severe HS. Reconstruction of the resultant defect is critical to ensure functional and aesthetic outcomes [7]. TDAP flaps have emerged as an effective reconstructive option for axillary HS, offering advantages such as robust vascular supply, minimal donor site morbidity, and adaptability for large defects [8]. Studies report high patient satisfaction and reduced recurrence rates with TDAP flaps compared to skin grafts or local flaps [9, 10].
Surgical technique and outcomes of TDAP flap
Preoperative planning involves perforator mapping using Doppler ultrasound. The flap axis is centered over the posterior axillary line, and incisions parallel the lateral thoracic fascia. After meticulous dissection and flap elevation, the defect is closed in layers over drains to prevent fluid accumulation. Proper flap positioning ensures complete coverage and preserves axillary mobility [10–12].
TDAP flaps offer significant advantages in reconstructing severe axillary HS defects, combining functional restoration, aesthetic results, durability, and minimal donor site morbidity. Their flexibility prevents contractures, ensuring a full range of motion, while the thin, hairless flap closely mimics axillary skin. The robust vascular supply reduces necrosis and recurrence risk, with donor site complications limited to scarring. Van Rappard et al. reported 89% patient willingness to recommend excision techniques, with 63% achieving recurrence-free outcomes. The TDAP flap is reliable for both acute and delayed reconstructions, solidifying its role as a preferred option in severe cases [13].
Comparison with other techniques
Alternative reconstructive techniques include local fasciocutaneous flaps, skin grafts, and musculocutaneous flaps. While these methods are more straightforward, they often lack the durability and functional outcomes TDAP flaps offer. Although skin grafts are easy to harvest, they may result in poor contouring and increased contractures. Local flaps carry the risk of recurrence if excision margins are inadequate. Musculocutaneous flaps, such as the gracilis flap, are suitable for complex perineal or buttock defects but may cause donor site morbidity [14, 15].
In conclusion, wide excision followed by TDAP V-Y advancement flap reconstruction offers an optimal balance of functional and aesthetic outcomes for severe axillary HS. Integrating preoperative imaging modalities, such as computed tomography angiography, may refine flap planning and enhance results as surgical techniques advance. Additionally, multidisciplinary approaches combining medical therapy with surgery could improve long-term outcomes, minimizing disease recurrence and optimizing patient satisfaction.
Author contributions
Conceptualization: HPL, NTT, and NTNL. Performed the operation: HPL and NTT. Project administration: NTT and NTNL. Writing—original draft: HPL, NP and NTT. Writing—review & editing: HPL and NTT. All authors read and approved the final paper.
Conflict of interest statement
The authors declare they have no relevant financial or non-financial interests to report.
Funding
This work was supported by Hue University under ID No. DHH2024–04-217. The authors also acknowledge partial support from Hue University’s Core Research Program, Grant No. NCM.DHH.2022.03.
Ethical approval
The authors’ institution waived ethical approval.
Informed consent
Written informed consent was obtained from the patient for anonymized information and accompanying images to be published in this article.



