-
PDF
- Split View
-
Views
-
Cite
Cite
Youness Slimi, Mohammed Frikal, Mohammed Mahmoudi, Karim Haddar, Houssam Boukabous, Abdelali Guellil, Rachid Jabi, Imane Skiker, Mohammed Bouziane, Small bowel obstruction unmasking an internal hernia through a broad ligament defect: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf074, https://doi.org/10.1093/jscr/rjaf074
Close - Share Icon Share
Abstract
Internal hernias are rare occurrences in which abdominal organs protrude through a mesenteric defect. Among these, herniation through the broad ligament is an especially uncommon type, comprising only 4% of all internal hernias. This condition can present with a wide spectrum of symptoms, ranging from abdominal pain to acute small bowel obstruction. Diagnosis is often difficult due to nonspecific clinical and radiological signs, making the condition a challenge to detect preoperatively. We present the case of a 30-year-old woman who developed an acute small bowel obstruction, identified through a CT scan. Surgical exploration revealed an incarcerated internal hernia passing through a defect in the broad ligament. After releasing the incarcerated bowel and closing the hernial orifice, the patient made a full recovery. This case provides additional insight into broad ligament hernias and the surgical approach to this rare condition.
Introduction
Hernias involving the broad ligament, a peritoneal structure that supports the female pelvic organs, are extremely rare [1]. These hernias typically occur when a defect in the broad ligament allows abdominal contents, most commonly small bowel, to protrude through. They were first identified in autopsy cases in the 19th century [2]. Though rare, they should be considered in the differential diagnoses when a patient presents with symptoms of bowel obstruction or unexplained pelvic pain. Broad ligament hernias can be congenital or acquired and are often diagnosed during surgical intervention. Due to the lack of specific clinical signs, the preoperative diagnosis of broad ligament hernias remains challenging [3].
This article discusses a rare case of a broad ligament hernia diagnosed in a 30-year-old woman, with a focus on its clinical presentation, diagnostic difficulties, and surgical management.
Case presentation
A 30-year-old woman, with a history of previous open appendectomy (via McBurney’s incision) and drainage of a presumed appendiceal abscess presented to the emergency department with severe hypogastric abdominal pain. Her past gynecological history was unremarkable. On examination, the patient appeared stable with mild tenderness in the hypogastric and periumbilical regions. There were no abnormalities noted on rectal examination.
Initial laboratory results showed a white blood cell count: 12580/μl (indicating mild leukocytosis) and normal hemoglobin: 12.1 g/dl and C-reactive protein: 2 mg/L.
A CT abdomen was conducted due to suspicion of a mechanical small bowel obstruction. The scan revealed a closed-loop dilation of the ileum in the pelvis, near the uterus, caused by an internal hernia through the right broad ligament (Fig. 1). In light of the clinical presentation suggesting small bowel obstruction, an exploratory laparotomy was carried out to evaluate and address the underlying cause.
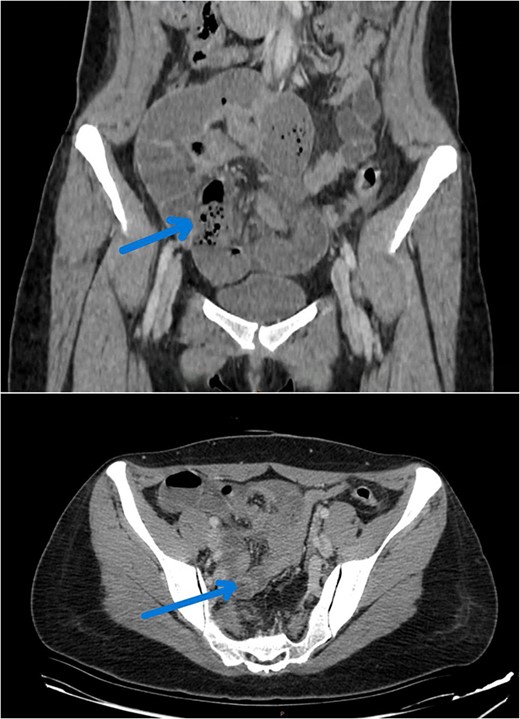
CT image reveals a closed dialed loop localized to the right of the uterus (arrow).
The laparotomy revealed an incarcerated segment of ileum passing through a defect in the right broad ligament; the diagnosis was made intraoperatively based on visual examination of the samll bowel and surrounding structures. The defect in the broad ligament was identified as part of a broader assessment of the bowel’s condition. No signs of bowel ischemia were noted despite the bowel’s incarceration (Fig. 2). After the herniated segment of ileum was reduced, the broad ligament defect was identified and repaired using continuous sutures to prevent recurrence. Additionally, a necrotic portion of the right fallopian tube was found and removed via a retrograde salpingectomy (Fig. 3).
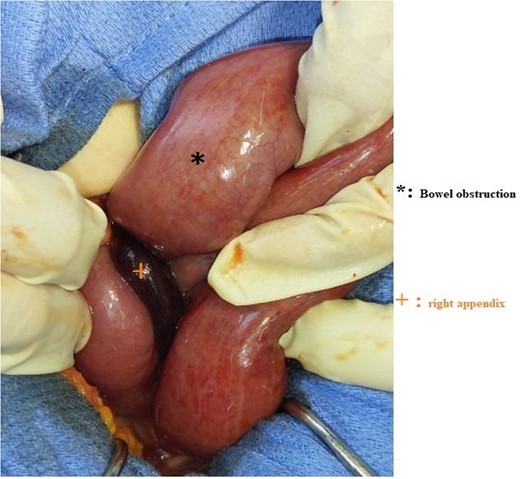
Intraoperative image showing a bowel obstruction with herniation of the right broad ligament.

Shows the specimen removed during the salpingectomy procedure, with a portion of the necrotic fallopian tube excised.
The postoperative course was uneventful, and the patient was discharged on the third postoperative day in a stable condition.
Discussion
Background and epidemiology
Internal hernias are rare, accounting for only 0.6% to 6% of all abdominal hernias. Of these, broad ligament hernias make up a very small percentage, with estimates ranging from 0.5% to 4% of all internal hernias [4, 5]. Internal hernias typically occur when abdominal organs protrude through a congenital or acquired defect in the mesentery, peritoneum, or other abdominal structures. Broad ligament hernias are particularly rare, and the condition is often difficult to diagnose due to the nonspecific nature of symptoms and the rarity of the hernia itself [6]. It is important to note that these hernias may remain asymptomatic for years or present with vague abdominal complaints, often being detected incidentally during surgical procedures for other conditions [7].
Broad ligament hernias may occur as a result of congenital peritoneal defects, though many cases are associated with acquired conditions such as pelvic inflammatory disease, endometriosis, or previous pelvic surgery, which can cause peritoneal adhesions [8]. These hernias can also result from anatomic variations in the broad ligament, such as incomplete fusion of the peritoneal layers [9].
Pathophysiology and classification
The broad ligament is a peritoneal fold that stabilizes the uterus, fallopian tubes, and ovaries. A hernia can occur when a defect or breach in the ligament allows abdominal contents, typically the small intestine, to protrude into the pelvic cavity. Broad ligament hernias are classified according to the location and extent of the defect in the ligament.
Three primary types of broad ligament hernias are described:
1. Type I: Defects located caudal to the round ligament of the uterus.
2. Type II: Defects above the round ligament, often involving the mesosalpinx.
3. Type III: Defects within the layers of the round ligament and mesometrium, typically more complex and prone to complications [10].
Clinical presentation
Symptoms of broad ligament hernias are highly variable and can include abdominal pain, nausea, vomiting, and signs of small bowel obstruction, such as distension and constipation [11]. These hernias may present with acute or chronic symptoms. In our case, the patient presented with acute hypogastric pain and signs of bowel obstruction, which led to the diagnosis during the emergency laparotomy. It is not uncommon for broad ligament hernias to remain undiagnosed for years and only become evident when complications such as bowel incarceration or strangulation occur [12].
Diagnosis
Preoperative diagnosis of broad ligament hernias is challenging due to the rarity of the condition and the nonspecific symptoms. Imaging modalities, such as CT scans and ultrasounds, can show signs of bowel obstruction or may suggest the presence of a transition point, but these findings alone are insufficient for a definitive diagnosis [13]. In some cases, CT imaging may reveal a hernia, but this is not always reliable, and a laparotomy or laparoscopy may be required for definitive diagnosis [14].
In the present case, the CT scan suggested a transition point indicative of bowel obstruction, which prompted surgical intervention. Intraoperative findings confirmed the broad ligament hernia, emphasizing the importance of direct visualization during surgery for accurate diagnosis.
Management and treatment
Management of broad ligament hernias usually involves surgical intervention. Historically, laparotomy was considered the gold standard for treatment as it allows direct visualization of the hernial defect and any associated complications. However, with the advancement of laparoscopic techniques, some cases are now treated minimally invasively, which can offer benefits such as reduced recovery time and fewer complications [15, 16].
In our case, a successful laparotomy was performed to reduce the incarcerated bowel and repair the broad ligament defect. The presence of a necrotic fallopian tube necessitated a retrograde salpingectomy. Laparotomy remains the preferred method in cases where complications such as bowel strangulation or necrosis are present, as was the case in this patient. Laparoscopic repair may be an option for uncomplicated cases [17].
Conclusion
Broad ligament hernias are rare but should be considered in the differential diagnosis of abdominal pain and bowel obstruction, especially in female patients. They remain challenging to diagnose preoperatively, but surgical exploration remains the most reliable method for diagnosis and treatment. Laparotomy continues to be the preferred approach for these cases, though laparoscopy is gaining popularity due to its benefits in terms of reduced recovery time and lower complication rates [18, 19].
A high index of suspicion should be maintained for internal hernias, particularly in patients with unexplained abdominal symptoms. Early diagnosis and surgical intervention are critical to prevent complications and recurrence.
Author contributions
S.Y. wrote the article, have consulted the patient, and prepared the patient for surgery and participated in the surgery. F.M. have helped collecting data. M.M. have helped writing the article, data collection. H.K. have helped collecting data. H.B. have helped collecting data. G.A. supervised the writing of manuscript. J.R. supervised the writing of manuscript. S.I. have posed the radiological diagnosis. B.M. have supervised the writing of the paper, and has been the leader surgeon of the case.
Conflict of interest statement
None declared.
Funding
None declared.



