-
PDF
- Split View
-
Views
-
Cite
Cite
Santiago Muñoz-Palomeque, Diego Molina-Mosquera, Felipe Pacheco-Barzallo, Beyond the weight loss: revisiting small bowel obstruction as an underestimated risk of intragastric balloons, Journal of Surgical Case Reports, Volume 2025, Issue 12, December 2025, rjaf998, https://doi.org/10.1093/jscr/rjaf998
Close - Share Icon Share
Abstract
Intragastric balloons (IGB) are a minimally invasive, reversible method for weight reduction in obese patients who fail conservative therapy but do not qualify for bariatric surgery. Despite their safety profile, rare yet severe complications can occur, such as small bowel obstruction (SBO) due to balloon migration. We present a case of a 37-year-old woman who developed SBO one year after gastric balloon placement, following successful weight loss. Imaging revealed a migrated balloon obstructing the jejunum, which required surgical extraction via enterotomy. This report compares our case with previously documented events, highlighting the clinical presentation, diagnostic challenges, and therapeutic decision-making. Although reported rates of obstruction remain below 0.2%, migration may occur months after the expected balloon excretion period. Persistent vigilance is required even long after IGB therapy. A stepwise diagnostic and management algorithm is proposed to guide clinicians facing this rare but potentially life-threatening complication.
Introduction
Obesity remains a major public health issue worldwide. Bariatric surgery is the most effective and durable intervention, but eligibility criteria—body mass index (BMI) ≥40 kg/m2 or ≥ 35 kg/m2 with comorbidities—exclude many patients who fail medical management consisting in lifestyle and pharmacologic interventions. For these individuals, intragastric balloon (IGB) therapy offers a minimally invasive, temporary option to induce weight loss by reducing gastric capacity and delaying gastric emptying [1].
IGBs induce early satiety by mechanically reducing gastric capacity and delaying gastric emptying [1]. Devices such as the Elipse™ swallowable intragastric balloon (EIGB) represents a significant advance, as it is designed for non-endoscopic placement and spontaneous excretion after ~16 weeks. A systematic review of 2013 patients by Vantanasiri et al. [2] found EIGB to be safe and effective, with a small-bowel obstruction (SBO) rate of only 0.13% (n = 3). Similarly, Ienca et al. [3] reported on 1770 consecutive patients and demonstrated an excellent safety profile with 14.2% total body weight loss (TBWL) and only three cases of SBO requiring surgical removal. Alsabah et al. [4] corroborated these findings, noting one SBO among 135 patients.
Nonetheless, rare yet serious adverse events—including migration and intestinal obstruction—continue to challenge the perceived safety of these devices. We describe a case of complete small bowel obstruction due to a migrated gastric balloon one year after placement, emphasizing diagnostic reasoning, surgical management, and lessons learned from literature comparison resumed in a practical guideline.
Case report
A 37-year-old woman with a history of gastric balloon placement one year prior for grade I obesity (initial BMI = 30.5 kg/m2) presented with five days of bilious vomiting and abdominal pain, worsened in the preceding 48 hours, along with inability to pass flatus. Her BMI at presentation was 24.09 kg/m2, consistent with sustained post-balloon weight reduction.
On examination, her abdomen was mildly distended, tender in the right iliac fossa and hypogastrium, with a positive Blumberg sign. Laboratory testing revealed leukocytosis (10 880/mm3) without neutrophilia. Ultrasound findings were unremarkable, but contrast-enhanced computed tomography (CT) demonstrated a foreign body within the jejunum, with proximal small bowel dilatation and a clear transition point—highly suggestive of gastric balloon migration and obstruction (Fig. 1).
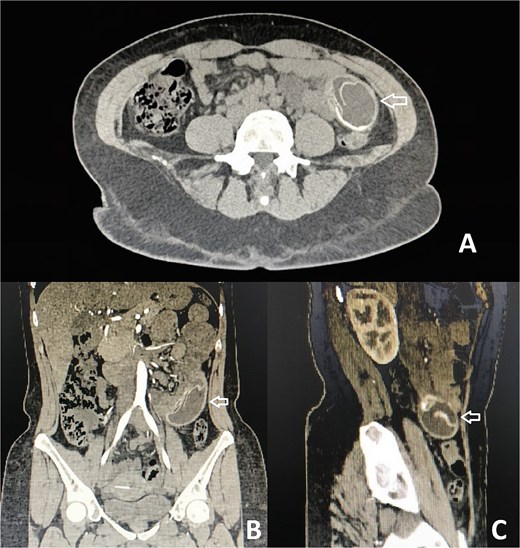
CT with evidence of a foreign body compatible with a migrated gastric balloon (indicated by the arrow). (A) Axial plane. (B) Coronal plane. (C) Sagittal plane.
An exploratory laparotomy confirmed distended stomach and proximal loops, with the balloon impacted ~60 cm distal to the ligament of Treitz, causing complete intraluminal obstruction (Fig. 2A). A transverse enterotomy was performed to extract the foreign body (Fig. 2B and C), followed by primary closure using absorbable polyglycolic suture (Fig. 3). The patient’s postoperative course was uneventful, and she was discharged on the fourth postoperative day.
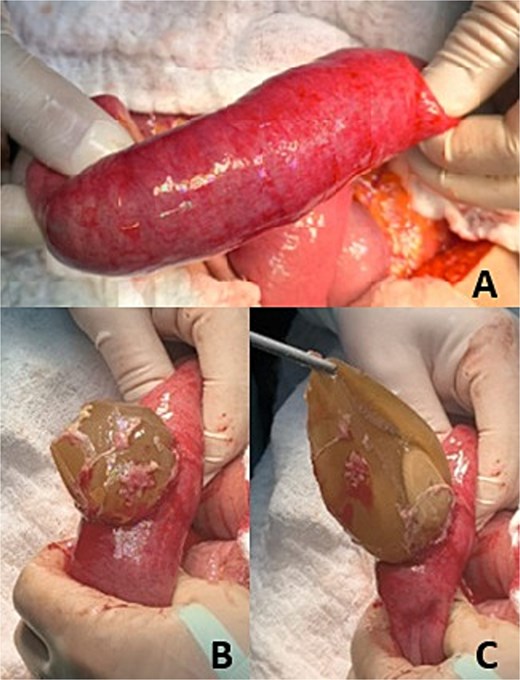
Intestinal obstruction. (A) Identification of the area of intestinal obstruction. (B) Enterectomy. (C) Removal of intraluminal foreign body (migrated gastric balloon).
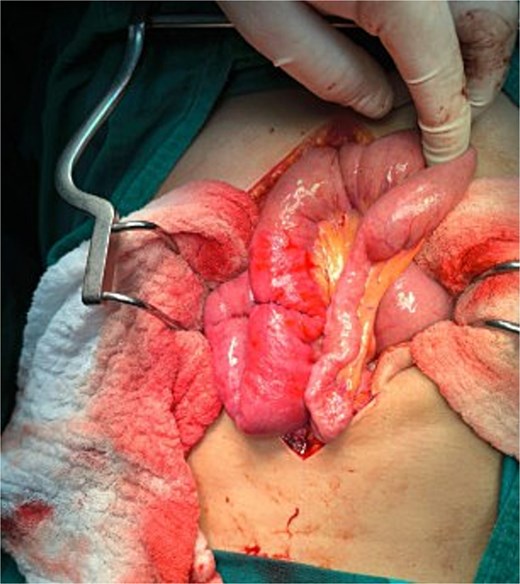
Transverse enterotomy raffia after removal of intraluminal foreign body (migrated gastric balloon).
Discussion
Although most IGB complications are minor (nausea, vomiting, reflux), migration leading to SBO is a rare but serious event. Migration typically follows balloon deflation, permitting passage through the pylorus into the small intestine [1, 5, 6].
Comparative analysis of reported cases (Table 1)
Comparative summary of reported cases of small bowel obstruction secondary to intragastric balloon migration.
| Author/Year . | Age/Sex . | BMI/Obesity Grade . | Time from IGB Insertion to Event . | Clinical Presentation . | Diagnostic Modality . | Location of Balloon . | Management . | Surgical/Endoscopic Approach . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Ntyl et al. [5], 2023 | 17 / F | 48.8 (morbid obesity) | Not specified | Early obstruction symptoms (vomiting, pain) | CT abdomen | Small bowel | Laparoscopic removal | Emergency laparoscopy | Full recovery |
| Bamakhrama et al. [6], 2023 | 33 / F | Not specified | 2 months | Epigastric pain, nausea, vomiting | CT abdomen | Proximal jejunum | Endoscopic retrieval | Endoscopic extraction with surgical backup | Full recovery |
| Di Saverio et al. [9], 2021 | 49 / F | 31.2 (obesity grade I | 9 months | Cramp-like pain, vomiting, no flatus/stools | X-ray + CT (triple contrast) | Distal jejunum | Laparoscopic enterotomy + intracorporeal suture | Laparoscopic surgery | Full recovery |
| Brizuela et al. [7], 2022 | 30 / F | Not specified | 18 months (delayed removal) | Severe abdominal pain, obstruction symptoms | CT abdomen | Not specified | Surgical enterotomy | Laparotomy | Full recovery |
| Moszkowicz & Lefevre [8], 2020 | 49 / M | Not specified | 11 months | Acute bowel obstruction | CT abdomen | Ileum | Enterostomy and suture | Laparotomy | Full recovery |
| Rzepa et al. [10], 2019 | Adult / M | 28 (overweight) | Not specified | Abdominal pain, IGB deflation | CT abdomen | Ileum | Enterotomy | Laparoscopy | Full recovery |
| Handaya et al. [11], 2020 | 46 / F | Not specified | 10 months | Gastric distension, salivation, nausea | CT scan + X-ray | 40 cm before ileocecal junction | Ileotomy | Laparoscopy | Full recovery, Discharged after 5 days |
| Mousavi Naeini & Sheikh [12], 2021 | 25 / M | Not specified | 5 months | Abdominal pain, methylene blue urine | CT + Endoscopy | Not specified | Enterotomy | Surgery | Full recovery |
| Muñoz-Palomeque et al., 2025 (This Case) | 37 / F | 24.09 (post-obesity) | 12 months | Bilious vomiting, abdominal pain, no flatus | CT abdomen | 60 cm distal to Treitz | Enterotomy + transverse closure (Vicryl) | Laparotomy | Uneventful recovery, discharged on day 4 |
| Author/Year . | Age/Sex . | BMI/Obesity Grade . | Time from IGB Insertion to Event . | Clinical Presentation . | Diagnostic Modality . | Location of Balloon . | Management . | Surgical/Endoscopic Approach . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Ntyl et al. [5], 2023 | 17 / F | 48.8 (morbid obesity) | Not specified | Early obstruction symptoms (vomiting, pain) | CT abdomen | Small bowel | Laparoscopic removal | Emergency laparoscopy | Full recovery |
| Bamakhrama et al. [6], 2023 | 33 / F | Not specified | 2 months | Epigastric pain, nausea, vomiting | CT abdomen | Proximal jejunum | Endoscopic retrieval | Endoscopic extraction with surgical backup | Full recovery |
| Di Saverio et al. [9], 2021 | 49 / F | 31.2 (obesity grade I | 9 months | Cramp-like pain, vomiting, no flatus/stools | X-ray + CT (triple contrast) | Distal jejunum | Laparoscopic enterotomy + intracorporeal suture | Laparoscopic surgery | Full recovery |
| Brizuela et al. [7], 2022 | 30 / F | Not specified | 18 months (delayed removal) | Severe abdominal pain, obstruction symptoms | CT abdomen | Not specified | Surgical enterotomy | Laparotomy | Full recovery |
| Moszkowicz & Lefevre [8], 2020 | 49 / M | Not specified | 11 months | Acute bowel obstruction | CT abdomen | Ileum | Enterostomy and suture | Laparotomy | Full recovery |
| Rzepa et al. [10], 2019 | Adult / M | 28 (overweight) | Not specified | Abdominal pain, IGB deflation | CT abdomen | Ileum | Enterotomy | Laparoscopy | Full recovery |
| Handaya et al. [11], 2020 | 46 / F | Not specified | 10 months | Gastric distension, salivation, nausea | CT scan + X-ray | 40 cm before ileocecal junction | Ileotomy | Laparoscopy | Full recovery, Discharged after 5 days |
| Mousavi Naeini & Sheikh [12], 2021 | 25 / M | Not specified | 5 months | Abdominal pain, methylene blue urine | CT + Endoscopy | Not specified | Enterotomy | Surgery | Full recovery |
| Muñoz-Palomeque et al., 2025 (This Case) | 37 / F | 24.09 (post-obesity) | 12 months | Bilious vomiting, abdominal pain, no flatus | CT abdomen | 60 cm distal to Treitz | Enterotomy + transverse closure (Vicryl) | Laparotomy | Uneventful recovery, discharged on day 4 |
Comparative summary of reported cases of small bowel obstruction secondary to intragastric balloon migration.
| Author/Year . | Age/Sex . | BMI/Obesity Grade . | Time from IGB Insertion to Event . | Clinical Presentation . | Diagnostic Modality . | Location of Balloon . | Management . | Surgical/Endoscopic Approach . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Ntyl et al. [5], 2023 | 17 / F | 48.8 (morbid obesity) | Not specified | Early obstruction symptoms (vomiting, pain) | CT abdomen | Small bowel | Laparoscopic removal | Emergency laparoscopy | Full recovery |
| Bamakhrama et al. [6], 2023 | 33 / F | Not specified | 2 months | Epigastric pain, nausea, vomiting | CT abdomen | Proximal jejunum | Endoscopic retrieval | Endoscopic extraction with surgical backup | Full recovery |
| Di Saverio et al. [9], 2021 | 49 / F | 31.2 (obesity grade I | 9 months | Cramp-like pain, vomiting, no flatus/stools | X-ray + CT (triple contrast) | Distal jejunum | Laparoscopic enterotomy + intracorporeal suture | Laparoscopic surgery | Full recovery |
| Brizuela et al. [7], 2022 | 30 / F | Not specified | 18 months (delayed removal) | Severe abdominal pain, obstruction symptoms | CT abdomen | Not specified | Surgical enterotomy | Laparotomy | Full recovery |
| Moszkowicz & Lefevre [8], 2020 | 49 / M | Not specified | 11 months | Acute bowel obstruction | CT abdomen | Ileum | Enterostomy and suture | Laparotomy | Full recovery |
| Rzepa et al. [10], 2019 | Adult / M | 28 (overweight) | Not specified | Abdominal pain, IGB deflation | CT abdomen | Ileum | Enterotomy | Laparoscopy | Full recovery |
| Handaya et al. [11], 2020 | 46 / F | Not specified | 10 months | Gastric distension, salivation, nausea | CT scan + X-ray | 40 cm before ileocecal junction | Ileotomy | Laparoscopy | Full recovery, Discharged after 5 days |
| Mousavi Naeini & Sheikh [12], 2021 | 25 / M | Not specified | 5 months | Abdominal pain, methylene blue urine | CT + Endoscopy | Not specified | Enterotomy | Surgery | Full recovery |
| Muñoz-Palomeque et al., 2025 (This Case) | 37 / F | 24.09 (post-obesity) | 12 months | Bilious vomiting, abdominal pain, no flatus | CT abdomen | 60 cm distal to Treitz | Enterotomy + transverse closure (Vicryl) | Laparotomy | Uneventful recovery, discharged on day 4 |
| Author/Year . | Age/Sex . | BMI/Obesity Grade . | Time from IGB Insertion to Event . | Clinical Presentation . | Diagnostic Modality . | Location of Balloon . | Management . | Surgical/Endoscopic Approach . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Ntyl et al. [5], 2023 | 17 / F | 48.8 (morbid obesity) | Not specified | Early obstruction symptoms (vomiting, pain) | CT abdomen | Small bowel | Laparoscopic removal | Emergency laparoscopy | Full recovery |
| Bamakhrama et al. [6], 2023 | 33 / F | Not specified | 2 months | Epigastric pain, nausea, vomiting | CT abdomen | Proximal jejunum | Endoscopic retrieval | Endoscopic extraction with surgical backup | Full recovery |
| Di Saverio et al. [9], 2021 | 49 / F | 31.2 (obesity grade I | 9 months | Cramp-like pain, vomiting, no flatus/stools | X-ray + CT (triple contrast) | Distal jejunum | Laparoscopic enterotomy + intracorporeal suture | Laparoscopic surgery | Full recovery |
| Brizuela et al. [7], 2022 | 30 / F | Not specified | 18 months (delayed removal) | Severe abdominal pain, obstruction symptoms | CT abdomen | Not specified | Surgical enterotomy | Laparotomy | Full recovery |
| Moszkowicz & Lefevre [8], 2020 | 49 / M | Not specified | 11 months | Acute bowel obstruction | CT abdomen | Ileum | Enterostomy and suture | Laparotomy | Full recovery |
| Rzepa et al. [10], 2019 | Adult / M | 28 (overweight) | Not specified | Abdominal pain, IGB deflation | CT abdomen | Ileum | Enterotomy | Laparoscopy | Full recovery |
| Handaya et al. [11], 2020 | 46 / F | Not specified | 10 months | Gastric distension, salivation, nausea | CT scan + X-ray | 40 cm before ileocecal junction | Ileotomy | Laparoscopy | Full recovery, Discharged after 5 days |
| Mousavi Naeini & Sheikh [12], 2021 | 25 / M | Not specified | 5 months | Abdominal pain, methylene blue urine | CT + Endoscopy | Not specified | Enterotomy | Surgery | Full recovery |
| Muñoz-Palomeque et al., 2025 (This Case) | 37 / F | 24.09 (post-obesity) | 12 months | Bilious vomiting, abdominal pain, no flatus | CT abdomen | 60 cm distal to Treitz | Enterotomy + transverse closure (Vicryl) | Laparotomy | Uneventful recovery, discharged on day 4 |
Clinical presentation
Our patient’s presentation—progressive abdominal pain, bilious vomiting, absence of flatus—parallels the 17-year-old woman reported by Ntyl et al. [5], who developed SBO due to balloon migration and was treated laparoscopically with full recovery. Bamakhrama et al. [6] described a 33-year-old woman presenting two months post-placement with jejunal obstruction successfully treated by endoscopic retrieval, emphasizing that endoscopic removal may be feasible in partial obstruction without perforation.
Timing and risk factors
Most events occur within 6–12 months after insertion, often linked to delayed retrieval or lost follow-up. Brizuela et al. [7] reported severe complications 18 months post-placement, highlighting the risk of extended retention. Moszkowicz and Lefevre [8] similarly noted SBO 11 months after insertion of an air-filled balloon. Our case occurred 12 months after placement, again suggesting prolonged retention and unnoticed deflation.
Diagnosis
CT scanning remains the diagnostic gold standard, confirming balloon location, obstruction level, and ruling out perforation. Di Saverio et al. [9] used triple-contrast CT to identify a distal jejunal obstruction from a BioEnterics balloon before laparoscopic removal. CT accuracy and rapid interpretation allow for early surgical planning, as demonstrated both in their case and ours.
Management
Approach depends on obstruction severity, balloon integrity, and migration site:
Endoscopic retrieval—as in Bamakhrama et al. [6]—for proximal, partially obstructive, or accessible balloons.
Laparoscopic enterotomy—as performed by Ntyl et al. [5], Di Saverio et al. [9], and Rzepa et al. [10]—for complete obstruction in stable patients.
Open laparotomy—as in our case and Handaya et al. [11]—for marked distension, uncertain anatomy, or distal impaction.
All cases reported favorable outcomes when intervention was timely, reinforcing that early recognition and prompt surgery prevent perforation and peritonitis.
Proposed clinical guideline for suspected balloon migration
Clinical suspicion. Any patient with a history of IGB therapy presenting with abdominal pain, vomiting, or constipation should raise immediate suspicion of migration.
Initial assessment.
Full physical exam for distension, tenderness, rebound.
Laboratory studies for leukocytosis or metabolic derangements.
Abdominal X-ray: may show dilated loops but low specificity.
Imaging confirmation.
Contrast-enhanced CT: defines migration site, degree of obstruction, and excludes perforation.
CT is essential prior to any attempted endoscopic or surgical retrieval.
Management algorithm.
Partial obstruction, proximal location, no perforation: Endoscopic retrieval under surgical standby [6].
Complete obstruction, distal migration Laparoscopic or open enterotomy [5, 9, 11].
Perforation, diffuse peritonitis, or uncertain anatomy Urgent open laparotomy
Postoperative care and prevention.
Early mobilization and diet progression as tolerated.
Documentation of balloon excretion or endoscopic removal within recommended duration (4–6 months).
Scheduled radiologic follow-up if spontaneous passage is expected (EIGB).
Conclusions
Despite widespread perception of safety, intragastric balloon therapy is not risk-free. Migration-related SBO remains a rare but significant event that may manifest months after therapy completion. The case described emphasizes the pivotal role of CT diagnosis, timely surgical intervention, and long-term follow-up.
Clinicians should maintain vigilance for persistent or late abdominal symptoms in post-IGB patients and adopt structured surveillance to confirm balloon retrieval or passage. Awareness of this potential complication ensures safe continuation of a valuable minimally invasive therapy for obesity.
Acknowledgements
A special acknowledgement to the staff of this illustrious journal for the opportunity to publish this research in this prestigious journal, and to contribute to the scientific and surgical community through it.
Author contributions
Santiago Muñoz-Palomeque: methodology, formal analysis, investigation, data curation, original draft preparation, visualization. Diego Molina-Mosquera: conceptualization, methodology, validation, formal analysis, review and editing, visualization. Felipe Pacheco-Barzallo: validation, formal analysis, visualization.
Conflict of interest statement
The authors declare that we have no personal, financial, intellectual, economic or corporate conflict of interest with the members of the journal.
Funding
No funding was provided for the preparation of this article.



