-
PDF
- Split View
-
Views
-
Cite
Cite
Dung Anh Vu, Nhat Dinh Vu, Tien Thanh Pham, Ngoc Binh Thai, Linh Thai Nguyen, Salvage re-revision total hip arthroplasty for severe femoral and acetabular bone defect complicated by periprosthetic joint infection and stem loosening: insights from geriatric orthopedics, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf932, https://doi.org/10.1093/jscr/rjaf932
Close - Share Icon Share
Abstract
Revision total hip arthroplasty with massive femoral and acetabular bone loss plus chronic periprosthetic joint infection is formidable in geriatric patients. A 73-year-old woman managed with a staged, soft-tissue-first pathway: extensive debridement, targeted antibiotics, and dead-space/coverage optimization, followed by defect-specific re-reconstruction. The acetabulum was rebuilt with a porous cup–cage anchored in reliable host bone; cavitary defects were buttressed with antibiotic-loaded cement. The femur was reconstructed using a modular tapered, fluted stem achieving diaphyseal fixation, with distal interlocking to enhance torsional control in a short, compromised isthmus. At 10 months, the patient had marked pain relief, community ambulation with a cane, and no reinfection, dislocation, or stem subsidence; radiographs demonstrated a stable cup–cage and maintained hip center. Although the techniques are established, this report highlights a pragmatic sequence integrating infection control, soft-tissue readiness, and fixation choices in a frail host, offering practical decision points for similarly complex re-revisions.
Introduction
Bipolar hip arthroplasty (BHA) and total hip arthroplasty (THA) remain established treatments for femoral neck fractures and end-stage osteoarthritis in older adults, reliably improving pain and function [1]. Advances in metallurgy, surfaces, and technique have expanded primary THA; as indications reach younger, active patients, concerns about longevity and reintervention have intensified notably [2]. Compared with primary surgery, revision THA (rTHA) carries greater technical difficulty and perioperative risk [3]. A central obstacle is deficient bone stock from chronic loosening, osteolysis, or deep infection. Although acetabular failures are more common than femoral loosening, they generate substantial periacetabular defects that jeopardize fixation and require advanced reconstruction [4]. On the femoral side, Paprosky type II–IV deficiencies reflect progressive proximal loss, predisposing to subsidence, renewed loosening, and mechanical failure; conserving native bone and promoting osseous regeneration are pivotal for durable stability and fewer re-revisions [5, 6]. Periprosthetic joint infection (PJI) affects roughly 0.57%–2.23% of cases yet exerts disproportionate clinical and economic impact, including heightened morbidity and psychological burden [7]. Infection-driven osteoclastic activity accelerates resorption, degrades bone quality, and increases fracture risk, compounding reconstructive complexity [8]. With a growing arthroplasty population, PJI cases will likely rise, reinforcing the need for rigorous infection control and staged protocols [9]. Periprosthetic acetabular fractures, though uncommon (0.07%–0.8%), are especially challenging when accompanied by loosening or PJI; soft-tissue deficiencies after debridement may necessitate plastic-surgical collaboration for reliable coverage. Given the likelihood of multiple revisions across a lifetime, salvage rTHA should pair definitive infection eradication with robust structural reconstruction using options such as bulk allograft, modular proximal femoral megaprosthesis, and porous metal augments, selected by defect pattern, comorbidities, and infection status [10]. This report describes an elderly patient with combined femoral and acetabular bone loss and chronic PJI managed by staged salvage re-rTHA, highlighting a multidisciplinary, stepwise algorithm from risk assessment to defect-specific reconstruction and coordinated perioperative care.
Case presentation
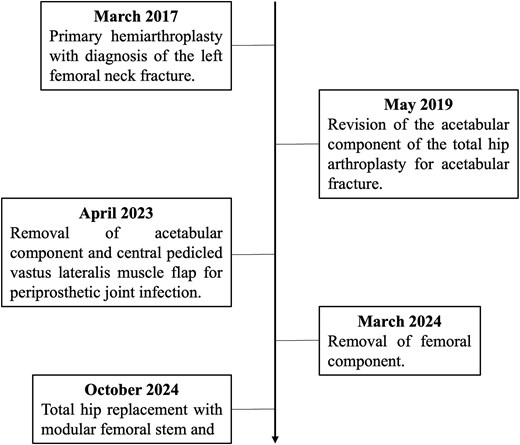
A 73-year-old woman presented with severe bone loss of the left proximal femur and extensive acetabular deficiency with pelvic discontinuity (Fig. 1). Initial treatment in 2017 for a displaced femoral neck fracture was bipolar hemiarthroplasty (Fig. 2A and B). After a new injury in 2019, an acetabular fracture with intrapelvic migration of the bipolar head occurred (Fig. 2C), leading to conversion to total hip arthroplasty with a revision acetabular component supported by a cup–cage (“trap”) construct (Fig. 2D). In 2023, PJI developed with loosening of both components; the acetabular component was explanted and a central pedicled vastus lateralis flap transposed to manage dead space (Fig. 2E and F). In May 2024, the femoral component was removed (Fig. 3A). CT confirmed mixed cavitary–segmental acetabular defects and marked metaphyseal loss of the proximal femur (Fig. 3B). After normalization of inflammatory markers and soft-tissue healing, salvage re-revision THA was performed. Acetabular reconstruction used a 52-mm porous shell–cage; two 45-mm tongues engaged host ilium and ischium, and cavitary defects were filled with antibiotic-loaded polymethylmethacrylate. Fixation comprised three intra-shell screws, four rim screws, and two tongue screws (Fig. 3C). On the femoral side, 2 cm of compromised proximal femur was resected to bleeding bone; the canal was reamed to 15 mm for circumferential endosteal contact. A modular tapered, fluted stem (14 × 260 mm) achieved distal fixation, supplemented by two distal interlocking screws; prophylactic cerclage mitigated iatrogenic fracture risk (Fig. 3C). Postoperatively, weight bearing advanced as tolerated. Serial AP pelvis radiographs showed a stable cup–cage without migration or progressive radiolucency and a well-seated stem without subsidence. At 10 months there were no complications, no infection or dislocation, and the patient ambulated with a cane; radiographs remained stable (Fig. 2D).
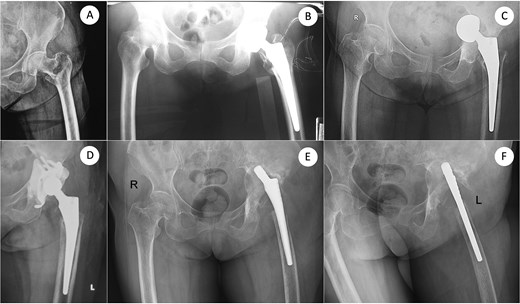
From femoral neck fracture and bipolar hemiarthroplasty to acetabular perforation, conversion THA, and acetabular component removal. (A) Anteroposterior (AP) pelvis radiograph demonstrating a displaced femoral neck fracture. (B) Immediate postoperative AP view after bipolar hemiarthroplasty using a standard femoral stem. (C) Subsequent acetabular perforation with intrapelvic migration of the bipolar head. (D) Conversion to total hip arthroplasty with an acetabular component supported by a cup–cage construct. (E, F) Same sitting: AP and cross-table lateral views obtained at the time of acetabular component explantation, delineating extensive acetabular bone loss. AP, anteroposterior.
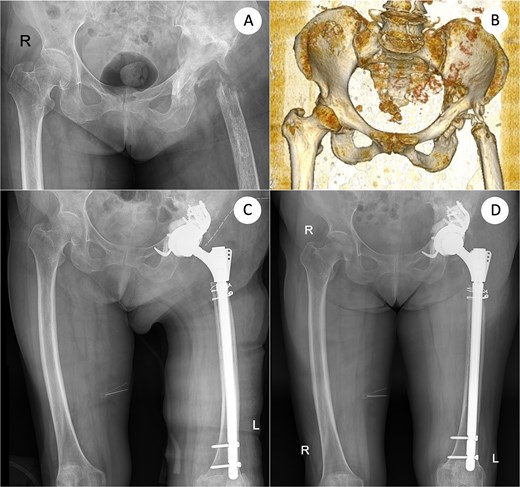
Definitive salvage re-revision THA: Defect assessment after femoral explant (AP and 3D-CT) and final reconstruction. (A) AP pelvis after removal of the femoral component showing severe acetabular and proximal femoral bone defects. (B) Three-dimensional computed-tomography (3D-CT) reconstruction corresponding to (A), confirming mixed cavitary–segmental acetabular defects. (C) Immediate postoperative AP radiograph after salvage re-revision total hip arthroplasty using a cup–cage acetabular reconstruction and a 260-mm modular tapered femoral stem secured with two distal interlocking screws. (D) AP X-ray taken 10 months after re-revision. AP, anteroposterior; 3D-CT, three-dimensional computed tomography; THA, total hip arthroplasty.
Discussion
Massive combined bone loss of the acetabulum and femur reframes rTHA as a problem of strategy rather than simple component exchange. Contribution lies less in implant novelty and more in operationalizing a pragmatic, staged pathway that integrates infection eradication, soft-tissue restoration, and defect-specific fixation in a frail, elderly host. We deliberately adopted a “soft-tissue-first” sequence, wide debridement, dead-space control, and vascularized coverage, before any reconstruction. Only after inflammatory markers normalized and the flap had matured did we pursue implants. This ordering, while familiar conceptually, is seldom illustrated with concurrent pelvic discontinuity and a short femoral canal, and we believe the case clarifies how to translate principles into stepwise decisions.
For the acetabulum, a porous cup–cage was selected to bridge the discontinuity, re-establish the hip center, and obtain purchase in reliable host bone. In chronically infected, comminuted sockets, cup–cage constructs provide off-the-shelf adaptability and intraoperative flexibility when custom triflange or distraction strategies may be impractical or slower to obtain [11]. Technical priorities included fully seating the cage before final screw tightening, directing screws into intact ilium and ischium, and packing cavitary voids with antibiotic-loaded cement to buttress the shell and reduce early micromotion. This approach permitted constrained orientation to lower dislocation risk in a deconditioned patient.
Profound metaphyseal loss made dependable diaphyseal purchase the nonnegotiable objective. A modular tapered, fluted stem provided axial and rotational stability through circumferential endosteal contact; because the isthmus was short and compromised, distal interlocking was added to enhance torsional control, a choice supported for B3-like patterns with limited isthmus bone [12]. Prophylactic cerclage mitigated iatrogenic fracture during preparation. This construct over proximal femoral replacement to preserve host bone, maintain modularity for future exchange, and provide reproducible rotational control during transfers and rehabilitation.
Infection control anchored the plan. Two-stage exchange remains a widely used standard for chronic PJI and, within coordinated pathways, achieves favorable infection-free survivorship despite increased procedural burden [13]. Where coverage is tenuous or dead space persists, vascularized muscle flaps, such as the vastus lateralis, improve perfusion, obliterate cavities, and facilitate subsequent reimplantation [14]. Limitations: a single case and 10-month follow-up limit generalizability. Even so, the report contributes explicit decision rules under real-world constraints, frailty, infection, discontinuity, and a short femoral canal, demonstrating early construct stability without dislocation or reinfection. Future work should test this algorithm prospectively with larger cohorts, longer follow-up, patient-reported outcomes, and cost analyses to define durability and scalability.
Acknowledgements
The study group extended their sincere appreciation to all participants for their valuable contributions.
Conflict of interest statement
The authors declare the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
No funding to declare.
References
- antibiotics
- diagnostic radiologic examination
- debridement
- acetabulum
- canes
- dislocations
- femur
- frail elderly
- hip region
- hip joint
- infectious disease prevention / control
- pain
- prosthesis-related infections
- reconstructive surgical procedures
- respiratory dead space
- arthroplasty
- hip replacement arthroplasty
- osteopenia
- geriatric orthopedics
- ambulation
- prosthetic joint infections
- older adult
- anatomical dead space
- community
- hip arthroplasty revision
- soft tissue
- reinfection



