-
PDF
- Split View
-
Views
-
Cite
Cite
Kaifan Li, Lei Yang, Yeyang Wang, Rare nontraumatic thoracic spondylolisthesis: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf802, https://doi.org/10.1093/jscr/rjaf802
Close - Share Icon Share
Abstract
Nontraumatic thoracic spondylolisthesis is extremely rare due to the thoracic spine’s inherent stability. We report the case of a 66-year-old male presenting with chronic low back pain and bilateral lower limb numbness. Imaging revealed anterior displacement of the T10 vertebral body with significant spinal cord compression at T10–T11. The patient underwent posterior spinal decompression, thoracic interbody fusion, and screw fixation, achieving complete neurological recovery at 1-year follow-up. Nontraumatic thoracic spondylolisthesis can result from facet joint laxity and disc degeneration causing vertebral micromovements. Early diagnosis and timely surgical intervention are crucial for preventing neurological damage and restoring function, highlighting the importance of comprehensive thoracic spine evaluation in patients with atypical lumbar symptoms.
Introduction
Thoracic spondylolisthesis represents an exceedingly rare spinal pathology, particularly in nontraumatic cases. The thoracic spine’s inherent stability, conferred by the rib cage and facet joints, renders degenerative spondylolisthesis uncommon in this region [1]. Most nontraumatic cases are associated with systemic conditions, including diffuse idiopathic skeletal hyperostosis, neurofibromatosis, and congenital deformities [2–4]. However, isolated degenerative spondylolisthesis leading to myelopathy remains extremely rare and clinically challenging. This condition often presents with insidious symptoms, including numbness, weakness, and gait disturbance in the lower limbs, and occasionally urinary dysfunction due to spinal cord compression [5]. Diagnosis is frequently delayed due to low incidence and nonspecific symptoms, often leading to misdiagnosis or attribution to more common lumbar pathologies. The clinical course varies widely, with some patients remaining asymptomatic while others develop debilitating neurological symptoms. Imaging modalities, particularly magnetic resonance imaging (MRI) and computed tomography (CT), are crucial in confirming diagnosis and assessing the extent of spinal cord compression. Timely intervention, including surgical decompression and fusion, is essential to prevent neurological deterioration and improve outcomes.
Case description
A 66-year-old male presented with a 1-year history of progressive low back pain and bilateral lower limb numbness, intensifying over the preceding month. Symptoms began insidiously without trauma and progressively worsened with prolonged standing and walking, improving with rest. The patient described deep, aching pain that significantly impacted his daily activities. Physical examination revealed bilateral lower limb numbness, especially prominent in the anterior thighs, an unsteady gait with a broad-based stance, decreased quadriceps muscle strength, reduced sensation below the navel extending to the groin, and positive bilateral Babinski signs indicating upper motor neuron involvement. Initial external X-rays suggested only L4 vertebral displacement, inconsistent with the clinical findings, prompting hospital admission for further evaluation. Refined imaging studies revealed previously unrecognized pathology. X-ray (Fig. 1A) and CT (Fig. 1B–D) demonstrated concomitant T10 vertebral body slippage, while MRI (Fig. 1E) showed severe T10/11 spinal cord compression with associated signal changes. The patient was diagnosed with thoracic spinal stenosis due to T10–T11 vertebral slip, explaining the bilateral lower extremity neurological symptoms and gait instability. Given the prolonged symptom duration, recurrent nature, and functional impact, surgical intervention was indicated after multidisciplinary discussion. The patient underwent T10–T11 thoracic interbody fusion with comprehensive decompression under general anesthesia. The procedure included herniated disc material removal, extensive posterior decompression, precise pedicle screw and titanium rod placement for stabilization, and autologous iliac crest bone grafting for interbody fusion. Postoperative management included comprehensive pain control and neurological monitoring. Follow-up X-ray (Fig. 2A and B) and CT (Fig. 2C–E) demonstrated successful vertebral realignment with the internal fixation in the ideal position. By postoperative Day 6, the patient reported significant back pain and leg numbness relief. Progressive improvement with structured physical therapy led to discharge on Day 10. One-year follow-up examination (Fig. 3) revealed stable fixation with continued symptom resolution, enabling free ambulation and complete return to normal activities.
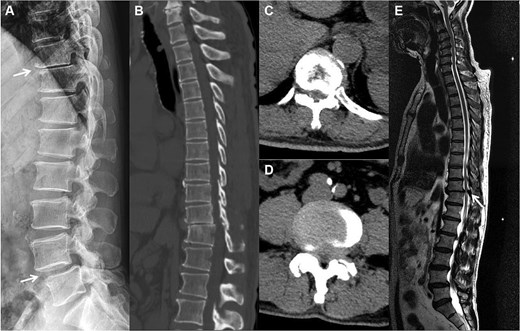
The preoperation imaging examinations. A sagittal X-ray (A) shows concomitant anterior displacement and instability of T10 and L4. A sagittal CT image (B) similarly demonstrates vertebral body slippage at T10, with stenosis and disc herniation of the spinal canal at the corresponding segments (C, D). T2-weighted imaging MRI (E) demonstrates severe spinal cord compression, with neurologic ischemic degeneration.

Postoperative X-ray and CT showed that the slipped thoracic 10 vertebra was reset, the internal fixation device was ideally positioned, and the spinal cord compression had disappeared.
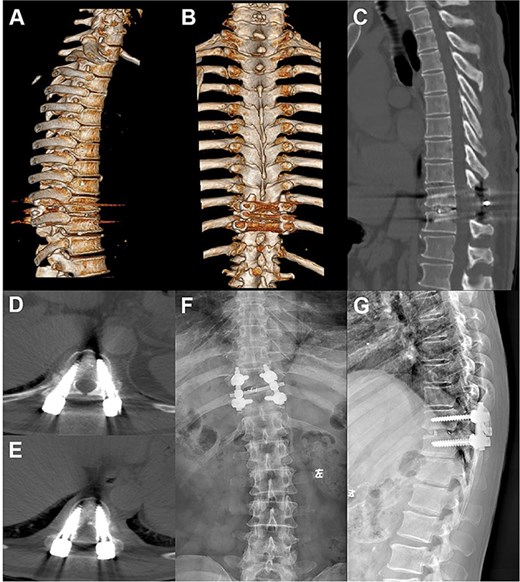
Postoperative follow-up images. (A–D) Repeat CT plain and 3D reconstruction at 6 months postoperatively showed ideal position of the T10–11 internal fixation and fusion device, straight posterior margin of the vertebral body, and no obvious signs of compression of the dural sac. (E, F) Review X-ray at 1 year postoperatively showed that the internal fixation device was in place without obvious dislocation, and the vertebral body slippage was satisfactorily repositioned.
Discussion
Primary nontraumatic thoracic spondylolisthesis represents an uncommon spinal condition with a complex pathophysiology. The etiology is multifactorial, involving degenerative changes such as disc degeneration, facet joint osteoarthritis, and ligamentous laxity contributing to gradual vertebral stability loss [6]. These age-related processes result in vertebral micromovements, leading to slippage. Nontraumatic spondylolisthesis may also affect younger patients with systemic connective tissue disorders. Additional factors include congenital vertebral abnormalities and conditions like neurofibromatosis causing structural weakness.
Thoracic spondylolisthesis’s incidence remains significantly lower than those of lumbar or cervical variants, which is attributed to the increased mechanical stability from rigid rib cage attachment and reduced thoracic mobility [1]. However, with aging populations and increasing degenerative conditions, the diagnosis frequency has increased. The clinical course demonstrates considerable variability, with some patients remaining asymptomatic while others experience rapidly progressive neurological symptoms.
Clinical manifestations range from mild discomfort to severe neurological deficits (Table 1). The common symptoms include chronic back pain, stiffness, and in advanced cases, radiculopathy or myelopathy. Spinal cord and nerve root compression from vertebral slippage can cause motor deficits, sensory disturbances, and bladder dysfunction. Secondary thoracic spinal stenosis may develop, further exacerbating neurological impairment.
Summary of clinical features and treatment strategies for reported nontraumatic thoracic spondylolisthesis
| Study . | Publication year . | Age (years), sex . | Level . | Symptom . | Treatment methods . |
|---|---|---|---|---|---|
| Fedorchuk et al. [2] | 2022 | 27, M | T9–10 | Back pain | Nonsurgical spinal rehabilitation |
| Wang et al. [7] | 2021 | 56, F | T11–12 | Gait disturbance, bilateral lower extremity numbness | Posterior decompression, internal fixation, and transforaminal fusion (T11/12) |
| Yuan et al. [8] | 2020 | 26, F | T2–5 | Weakness and numbness in legs | Posterior decompression, internal fixation, and fusion |
| Takagi et al. [9] | 2017 | 78, M | T3–4, T10–11 | Gait disturbance | Posterior decompression, internal fixation, and fusion (T9–T12) |
| Hsieh et al. [3] | 2014 | 61, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| 71, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T9–T11) | ||
| 58, F | T10–11 | Leg weakness, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) | ||
| 71, F | T10–11 | Gait disturbance, paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T9–T10) | ||
| 58, M | T11–12 | Low back pain, gait disturbance, and paraparesis | Thoracolumbar orthosis | ||
| Muhammad et al. [5] | 2012 | 15, M | T12–L1 | Back pain, bilateral lower limb pain | Posterior decompression, internal fixation, and posterolateral fusion (T8–L4) |
| Shimada et al. [10] | 2006 | 44, F | T11–12 | Gait disturbance, lower-extremity bilateral numbness | Posterior decompression, internal fixation, and posterolateral fusion (T10–12) |
| Otoshi et al. [6] | 2000 | 68, F | T11–12 | Thigh numbness, anterior pain | Posterior laminectomy decompression and interbody fusion (T11/T12) |
| Ishibashi et al. [4] | 1999 | 68, F | T12–L1 | Intermittent claudication, lower-extremity numbness | Posterior laminectomy decompression (T12/L1) |
| 70, M | T11–12 | Gait disturbance, lower extremity sensory disturbance | Posterior fenestration decompression (T11/T12) | ||
| Present case | 66, M | T10–11 | Low back pain, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| Study . | Publication year . | Age (years), sex . | Level . | Symptom . | Treatment methods . |
|---|---|---|---|---|---|
| Fedorchuk et al. [2] | 2022 | 27, M | T9–10 | Back pain | Nonsurgical spinal rehabilitation |
| Wang et al. [7] | 2021 | 56, F | T11–12 | Gait disturbance, bilateral lower extremity numbness | Posterior decompression, internal fixation, and transforaminal fusion (T11/12) |
| Yuan et al. [8] | 2020 | 26, F | T2–5 | Weakness and numbness in legs | Posterior decompression, internal fixation, and fusion |
| Takagi et al. [9] | 2017 | 78, M | T3–4, T10–11 | Gait disturbance | Posterior decompression, internal fixation, and fusion (T9–T12) |
| Hsieh et al. [3] | 2014 | 61, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| 71, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T9–T11) | ||
| 58, F | T10–11 | Leg weakness, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) | ||
| 71, F | T10–11 | Gait disturbance, paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T9–T10) | ||
| 58, M | T11–12 | Low back pain, gait disturbance, and paraparesis | Thoracolumbar orthosis | ||
| Muhammad et al. [5] | 2012 | 15, M | T12–L1 | Back pain, bilateral lower limb pain | Posterior decompression, internal fixation, and posterolateral fusion (T8–L4) |
| Shimada et al. [10] | 2006 | 44, F | T11–12 | Gait disturbance, lower-extremity bilateral numbness | Posterior decompression, internal fixation, and posterolateral fusion (T10–12) |
| Otoshi et al. [6] | 2000 | 68, F | T11–12 | Thigh numbness, anterior pain | Posterior laminectomy decompression and interbody fusion (T11/T12) |
| Ishibashi et al. [4] | 1999 | 68, F | T12–L1 | Intermittent claudication, lower-extremity numbness | Posterior laminectomy decompression (T12/L1) |
| 70, M | T11–12 | Gait disturbance, lower extremity sensory disturbance | Posterior fenestration decompression (T11/T12) | ||
| Present case | 66, M | T10–11 | Low back pain, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
Summary of clinical features and treatment strategies for reported nontraumatic thoracic spondylolisthesis
| Study . | Publication year . | Age (years), sex . | Level . | Symptom . | Treatment methods . |
|---|---|---|---|---|---|
| Fedorchuk et al. [2] | 2022 | 27, M | T9–10 | Back pain | Nonsurgical spinal rehabilitation |
| Wang et al. [7] | 2021 | 56, F | T11–12 | Gait disturbance, bilateral lower extremity numbness | Posterior decompression, internal fixation, and transforaminal fusion (T11/12) |
| Yuan et al. [8] | 2020 | 26, F | T2–5 | Weakness and numbness in legs | Posterior decompression, internal fixation, and fusion |
| Takagi et al. [9] | 2017 | 78, M | T3–4, T10–11 | Gait disturbance | Posterior decompression, internal fixation, and fusion (T9–T12) |
| Hsieh et al. [3] | 2014 | 61, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| 71, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T9–T11) | ||
| 58, F | T10–11 | Leg weakness, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) | ||
| 71, F | T10–11 | Gait disturbance, paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T9–T10) | ||
| 58, M | T11–12 | Low back pain, gait disturbance, and paraparesis | Thoracolumbar orthosis | ||
| Muhammad et al. [5] | 2012 | 15, M | T12–L1 | Back pain, bilateral lower limb pain | Posterior decompression, internal fixation, and posterolateral fusion (T8–L4) |
| Shimada et al. [10] | 2006 | 44, F | T11–12 | Gait disturbance, lower-extremity bilateral numbness | Posterior decompression, internal fixation, and posterolateral fusion (T10–12) |
| Otoshi et al. [6] | 2000 | 68, F | T11–12 | Thigh numbness, anterior pain | Posterior laminectomy decompression and interbody fusion (T11/T12) |
| Ishibashi et al. [4] | 1999 | 68, F | T12–L1 | Intermittent claudication, lower-extremity numbness | Posterior laminectomy decompression (T12/L1) |
| 70, M | T11–12 | Gait disturbance, lower extremity sensory disturbance | Posterior fenestration decompression (T11/T12) | ||
| Present case | 66, M | T10–11 | Low back pain, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| Study . | Publication year . | Age (years), sex . | Level . | Symptom . | Treatment methods . |
|---|---|---|---|---|---|
| Fedorchuk et al. [2] | 2022 | 27, M | T9–10 | Back pain | Nonsurgical spinal rehabilitation |
| Wang et al. [7] | 2021 | 56, F | T11–12 | Gait disturbance, bilateral lower extremity numbness | Posterior decompression, internal fixation, and transforaminal fusion (T11/12) |
| Yuan et al. [8] | 2020 | 26, F | T2–5 | Weakness and numbness in legs | Posterior decompression, internal fixation, and fusion |
| Takagi et al. [9] | 2017 | 78, M | T3–4, T10–11 | Gait disturbance | Posterior decompression, internal fixation, and fusion (T9–T12) |
| Hsieh et al. [3] | 2014 | 61, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
| 71, M | T10–11 | Leg weakness, gait disturbance | Posterior decompression, internal fixation, and posterolateral fusion (T9–T11) | ||
| 58, F | T10–11 | Leg weakness, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) | ||
| 71, F | T10–11 | Gait disturbance, paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T9–T10) | ||
| 58, M | T11–12 | Low back pain, gait disturbance, and paraparesis | Thoracolumbar orthosis | ||
| Muhammad et al. [5] | 2012 | 15, M | T12–L1 | Back pain, bilateral lower limb pain | Posterior decompression, internal fixation, and posterolateral fusion (T8–L4) |
| Shimada et al. [10] | 2006 | 44, F | T11–12 | Gait disturbance, lower-extremity bilateral numbness | Posterior decompression, internal fixation, and posterolateral fusion (T10–12) |
| Otoshi et al. [6] | 2000 | 68, F | T11–12 | Thigh numbness, anterior pain | Posterior laminectomy decompression and interbody fusion (T11/T12) |
| Ishibashi et al. [4] | 1999 | 68, F | T12–L1 | Intermittent claudication, lower-extremity numbness | Posterior laminectomy decompression (T12/L1) |
| 70, M | T11–12 | Gait disturbance, lower extremity sensory disturbance | Posterior fenestration decompression (T11/T12) | ||
| Present case | 66, M | T10–11 | Low back pain, gait disturbance, and paraparesis | Posterior decompression, internal fixation, and posterolateral fusion (T10/11) |
In clinical practice, particular attention should be paid to patients with apparent lumbar pathology who lack typical lumbar symptoms or whose presentation seems inconsistent with imaging findings. A comprehensive thoracic spine evaluation should systematically exclude thoracic spondylolisthesis or stenosis that may mimic lumbar disorders [10]. Given the anatomical complexity and biomechanical interconnections, thoracic cord pathology symptoms frequently present in adjacent regions, making diagnosis challenging without comprehensive imaging. Early imaging examination of thoracic spinal cord facilitates timely intervention and improves outcomes.
Surgical treatment represents the gold standard for symptomatic thoracic spondylolisthesis with significant neurological compromise or spinal instability (Table 1). Posterior short-segment decompression and fusion with internal fixation aims to relieve compression, restore alignment, and provide long-term stability. Clinical results demonstrate consistently favorable outcomes with high symptom improvement rates.
For carefully selected patients without significant neurological symptoms, conservative management may be considered. Nonsurgical treatments, including physical therapy [9] and bracing [5], have demonstrated effectiveness in symptom alleviation. However, conservative management requires careful patient selection and monitoring for neurological progression.
Caution is warranted regarding potential thoracic–lumbar spondylolisthesis co-occurrence, given the anatomical and biomechanical relationships between spinal regions, especially in degenerative conditions [5]. When both conditions are diagnosed, assessment of the clinical significance and symptomatic contribution of each level is crucial. If thoracic spondylolisthesis primarily contributes to neurological symptoms, targeted thoracic intervention may provide substantial relief while avoiding unnecessary lumbar procedures. In conclusion, timely diagnosis and appropriate surgical intervention are critical for preventing irreversible neurological damage in this rare but potentially devastating condition.
Conflict of interest statement
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This study was supported by the Guangzhou Science and Technology Plan Project (2023A03J0266) and the Guangdong Second Provincial General Hospital’s Special Fund for the Lifting Project (TJGC-2023009).
References
- bone marrow diseases
- bone screws
- decompression, surgical
- follow-up
- spinal cord compression
- spinal cord diseases
- spinal fusion
- spondylolisthesis
- surgical procedures, operative
- nervous system trauma
- zygapophyseal joint
- diagnostic imaging
- degenerative spondylolisthesis
- vertebrae
- thoracic spine
- degenerative disc disease
- spinal cord decompression
- chronic low back pain
- vertebral body
- limb numbness
- early diagnosis



