-
PDF
- Split View
-
Views
-
Cite
Cite
Hisashi Ro, Shun Ishiyama, Makoto Takahashi, Kiichi Sugimoto, Laparoscopic repair of recurrent inguinal hernia via a contralateral high-peritoneal-incision approach: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf912, https://doi.org/10.1093/jscr/rjaf912
Close - Share Icon Share
Abstract
Recurrent inguinal hernias remain surgically challenging, especially after anterior mesh repair, due to dense adhesions and altered anatomy. Laparoscopic transabdominal preperitoneal (TAPP) repair offers diagnostic and therapeutic advantages, but severe adhesions may limit ipsilateral dissection. We report a 77-year-old man with bilateral inguinal hernias, including a recurrent left hernia after mesh plug repair. Anticipating adhesions, a high peritoneal incision was made on the contralateral side, and dissection was extended across the midline. This approach allowed safe identification and repair of the recurrent defect using a ProGrip™ mesh. Although the overlap was limited, additional fixation ensured stability. The patient had an uneventful postoperative course. The contralateral high-incision TAPP approach may represent a feasible and effective option when ipsilateral access is hazardous, highlighting the importance of flexible strategies for mesh placement and fixation in complex recurrent hernias.
Introduction
Inguinal hernia repair is a common general surgical procedure. The transabdominal preperitoneal (TAPP) approach provides superior visualization, less chronic pain, and faster recovery than open repair [1]. However, recurrence after anterior mesh repair remains challenging because of adhesions and distorted anatomy. Laparoscopic repair offers lower recurrence and pain rates in such cases [2]. We report a recurrent inguinal hernia successfully treated by a contralateral high-peritoneal-incision TAPP approach, enabling safe dissection through an unscarred plane.
Case presentation
A 77-year-old man (162 cm, 71.8 kg) with hypertension and benign prostatic hyperplasia presented with a left groin bulge. He had undergone open anterior mesh plug repair 15 years earlier using two L-size plugs for left direct and indirect hernias (EHS classification: M1, L1) [3]. Current examination and prone CT with abdominal compression revealed a recurrent left inguinal hernia containing omentum (Fig. 1a and b).
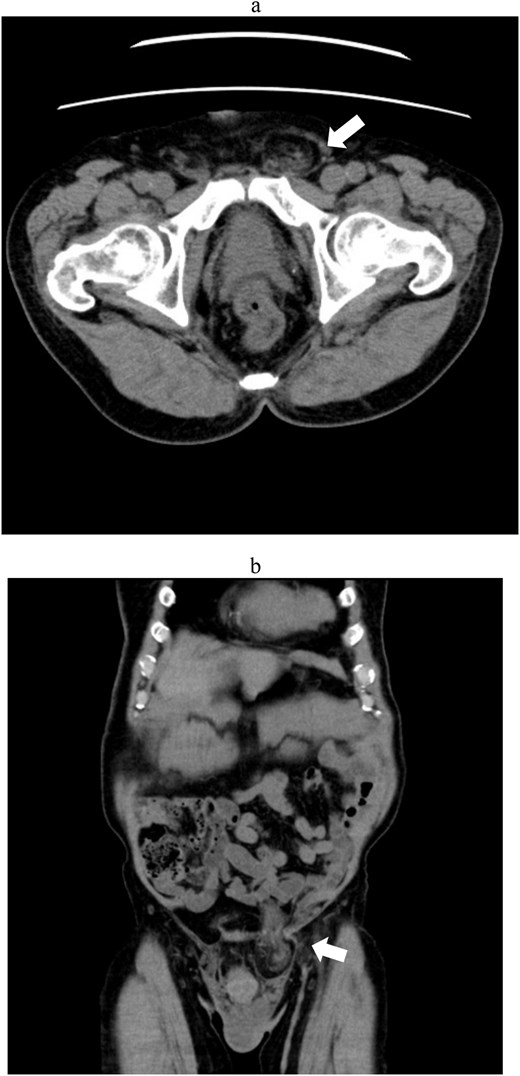
Abdominal computed tomography showing a recurrent left inguinal hernia (arrows) containing omental tissue. (a) Axial view. (b) Coronal view.
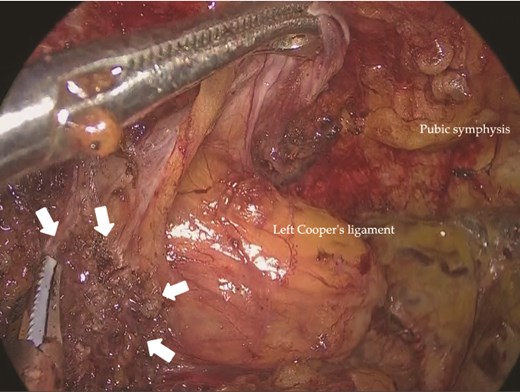
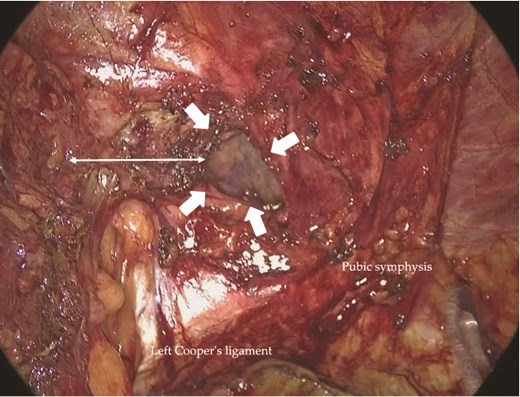
Under general anesthesia, a 12-mm camera port was inserted through the umbilicus, and two 5-mm ports were placed in the lower quadrants. Laparoscopic exploration revealed two mesh plugs on the left with fibrotic scarring and adhesions, which obscured the exact hernia orifice (Fig. 2). An incidental right direct hernia (M3) was also identified intraoperatively. Because severe adhesions were anticipated on the left, the operation was initiated on the right. A high peritoneal incision was initiated medial to the right anterior superior iliac spine (Fig. 3). The pseudosac was dissected while preserving the retropubic fascia, and the preperitoneal dissection was extended across the midline into the left side (Fig. 4). Approaching from the contralateral side allowed progressive entry into the adhesion-laden region through an unscarred plane, improving visualization and minimizing peritoneal injury.
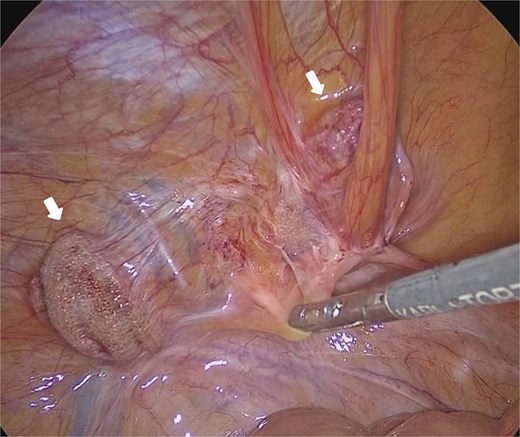
Laparoscopic view of the left inguinal region showing two previously placed mesh plugs (arrows). No definite recurrent hernia orifice was identified. Dense adhesions were present around the plugs.
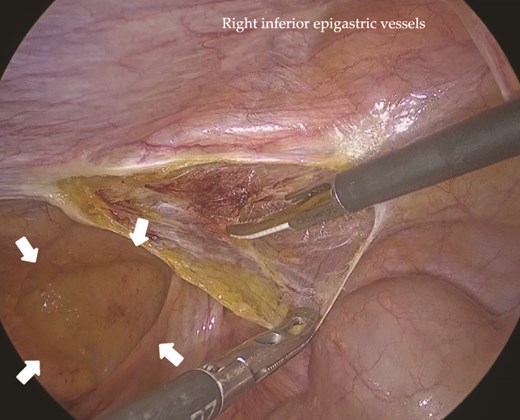
Intraoperative view of the right inguinal region before repair. A right indirect inguinal hernia with a defect measuring >30 mm was observed (arrows). A high peritoneal incision was made near the right anterior superior iliac spine.
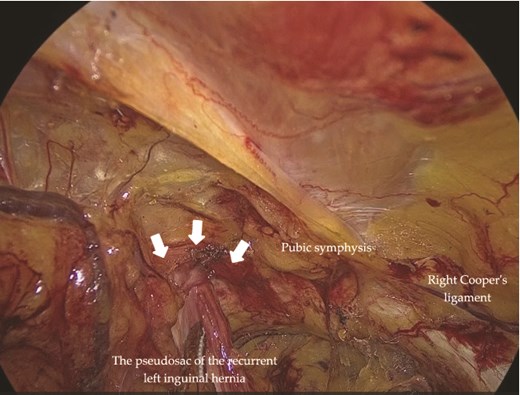
Intraoperative view of the left inguinal region. The recurrent hernia orifice (arrows) and pseudosac were located adjacent to the pubic symphysis. Dense fibrotic adhesions were present around the pseudosac.
On the left, the recurrent hernia orifice was identified adjacent to one of the mesh plugs, with the pseudosac firmly adherent to the plug (Fig. 5). After careful sharp and blunt dissection, a recurrent orifice was clearly exposed in the left pubic region and classified as R1M2 (Fig. 6). A circumferential margin of ~2.5 cm was secured around the defect. The laterally placed plug did not interfere with the repair and was left in situ. A 15 × 10 cm self-gripping mesh (ProGrip™) was placed to cover the recurrent defect with a 2.5 cm margin and was supplemented with tacker fixation because overlap was limited (Fig. 7). Although the left-sided mesh covered the right hernia orifice, overlap on the right was insufficient (Fig. 8), so an additional mesh was applied for reinforcement. The right-sided high peritoneal incision was sutured and closed in a standard fashion (Fig. 9). The postoperative course was uneventful. At 5-month follow-up, there was no clinical evidence of recurrence.
Adhesions between the previously placed mesh (arrows) and the peritoneum in the left inguinal region.
Intraoperative view of the left inguinal region. An R1M2-type recurrent hernia orifice (arrows) was identified adjacent to a mesh plug. A circumferential margin of ~2.5 cm (double-headed arrow) was secured around the defect.
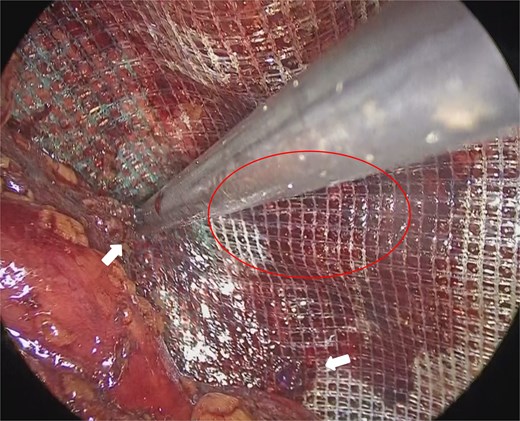
Mesh fixation using a tacker (arrows). The distance from the recurrent hernia orifice (circle) was limited.
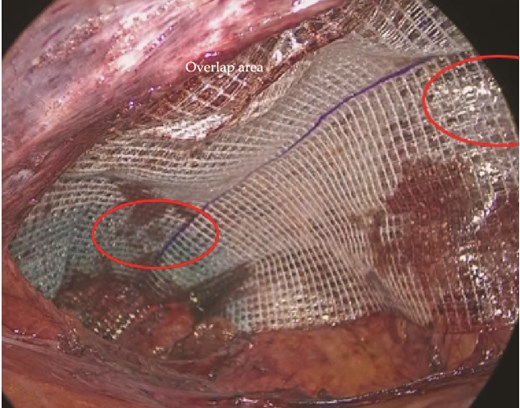
Mesh placed on the left side (circle) and secured with tackers. The right-sided hernia orifice (circle) was fully covered.
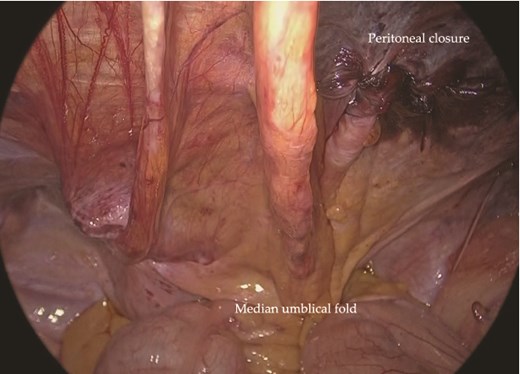
Completed repair of the left recurrent hernia using contralateral high-peritoneal access from the right side.
Discussion
Reoperative repair of recurrent inguinal hernia after anterior plug mesh repair is technically challenging because dense adhesions and fibrosis obscure the preperitoneal plane. Ipsilateral dissection in such cases increases the risk of peritoneal tearing and difficulty in primary closure. In our case, two pre-existing plugs and scarring made local incision hazardous. By initiating dissection from the contralateral side with a high peritoneal incision, we entered the Retzius and Bogros spaces through intact peritoneum and created a continuous, thick flap. This approach provided wide exposure of the myopectineal orifice and allowed safe crossover beneath an intact layer, facilitating controlled dissection around the previous mesh.
Guidelines recommend switching the operative plane in recurrent hernia repair—using a posterior approach (TAPP/TEP) after anterior repair and vice versa [1, 4]. Our method followed this principle and further refined it by performing a contralateral high incision to avoid fragile ipsilateral peritoneum. This approach preserved the advantages of laparoscopy, including excellent visualization and the ability to repair bilateral defects in one session. Although the management of asymptomatic contralateral hernias remains controversial, some reports discourage routine repair [5], whereas others advocate repair regardless of size [6]. When preoperative consent is obtained, inspection and repair of a contralateral hernia during TAPP can be performed in accordance with international recommendations [1]. Repairing bilateral defects in a single session may also reduce the risk of future contralateral occurrence and the need for reoperation [7, 8].
A key factor in achieving durable hernia repair is securing adequate mesh overlap. The European Hernia Society recommends at least 3–4 cm in all directions and 4–5 cm for large or recurrent hernias [9]. Although the 2024 Japanese guidelines do not specify an exact value, expert consensus similarly supports ≥3 cm for primary and 4–5 cm for recurrent cases, generally using meshes of at least 10 × 15 cm [4]. In our case, overlap was limited to ≈2.5 cm because of a residual plug and scarring. To compensate, a self-gripping mesh and selective absorbable tacker fixation were used within safe zones (Cooper’s ligament, medial edge of the internal ring) to avoid neurovascular injury. Nevertheless, limited overlap remains a potential cause of re-recurrence. Thorough preoperative planning and intraoperative flexibility—including mesh augmentation or modification of the approach—are essential for secure and lasting repair.
This contralateral high–peritoneal-incision TAPP approach is not applicable to all recurrences. It is particularly useful for (i) recurrence after anterior underlay mesh repair with fragile peritoneum; (ii) suspected contralateral occult hernia, especially direct type; and (iii) extensive adhesions between the ipsilateral peritoneum and bowel. Contraindications or cautious indications include (i) prior pelvic or prostate surgery, (ii) re-recurrence after posterior mesh repair (TAPP/TEP), (iii) large defects with insufficient mesh overlap, and (iv) contralateral occult indirect hernia requiring deep dissection. A simplified decision-making algorithm summarizing our selection process is shown (Fig. 10).
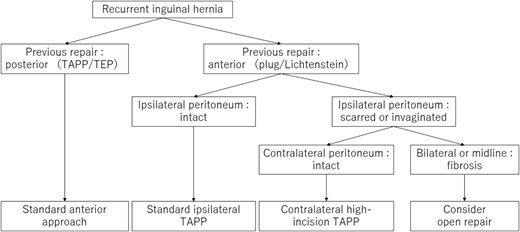
Simplified algorithm for choosing the operative approach in recurrent inguinal hernia.
This study has inherent limitations. It describes a single case has relatively short follow-up, and fixation relied on absorbable tackers, which may offer less durable anchoring. Nevertheless, the contralateral high-incision TAPP provided safe access through unscarred tissue, enabling reliable repair in a complex recurrent setting. Further accumulation of cases is needed to validate its role in recurrent inguinal hernia surgery.
This technique may expand the laparoscopic armamentarium for complex recurrent hernias, providing an additional option when ipsilateral access is compromised.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
The authors received no specific funding for this work.



