-
PDF
- Split View
-
Views
-
Cite
Cite
Renaldi Prasetia, Rio Aditya, Greesea Dinamaria Whitiana, Joshua Edward Hananto, Siti Zainab Bani Purwana, Greater tuberosity osteotomy: a treatment breakthrough in a case of bilateral old-unreduced malunion fracture-dislocation of proximal humerus, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf854, https://doi.org/10.1093/jscr/rjaf854
Close - Share Icon Share
Abstract
Anterior shoulder dislocation occurs in 95% of all shoulder dislocation. Pathological changes such as bone loss may occur in neglected cases, which can cause locking of the humeral head, complicating the procedure needed for reduction. A 26-year-old male patient presented to the clinic with pain and limited range of motion 2 months after a fall, with a history of unsuccessful treatment by a traditional bonesetter and recurrent right shoulder dislocations. The patient was diagnosed with bilateral neglected closed fracture dislocation of proximal humerus Neer 2-part and underwent open reduction with greater tuberosity (GT) osteotomy and PHILOS plate fixation. GT osteotomy for locked fracture-dislocations of the proximal humerus allowed for enhanced posterior visualization, enabling a safer reduction while preserving the subscapularis muscle and facilitating the reconstruction of the Hill-Sachs lesion.
Introduction
Anterior shoulder dislocation occurs in 95% of all shoulder dislocation [1, 2]. When these injuries are neglected, they often complicated with pathological changes such as bone loss, contracted capsules, and damages to the rotator cuff [1, 3, 4]. Furthermore, fractures of the greater tuberosity (GT), present in ~15% of anterior shoulder dislocations, may indicate rotator cuff damage [2, 5].
Conservative treatment for old, unreduced dislocations tends to yield poor results [3, 6, 7]. Adequate approach and visualization have previously been done with osteotomy, often through coracoid osteotomy, with the osteotomized bone utilized to fill the glenoid defect [6].
This report details the complex management of a young male who presented with debilitating bilateral, old-unreduced malunion fracture-dislocations of the proximal humerus. The bilateral nature of this case, combined with the chronicity, malunion, and extensive associated pathology including GT fractures and Hill-Sachs lesions, presented a unique and substantial therapeutic challenge.
Case report
A 26-year-old man came into the orthopaedic clinic with pain and instability in his right shoulder. Two months before admission he slipped and fell backwards with both arms supporting his bodyweight. There was no sensory deficit found. The patient had a history of recurrent dislocation on his right shoulder which occurs twice over the past 4 years. The patient previously sought treatment from a bone setter, however, no improvements were achieved. After seeking help to a proper medical facility, the patient was eventually referred to our tertiary hospital.
Physical examination was conducted. The deltoid contour was lost on the right and left shoulder. There was no swelling, bruising, wound, or scar found. Neurovascular test on the distal part of both shoulders indicates intact structures. Limitation of shoulder range of motion (ROM) was noted (Fig. 1). Plain radiographs and CT scan (Fig. 2) showed a bilateral anterior dislocation of the glenohumeral joint with GT fracture.
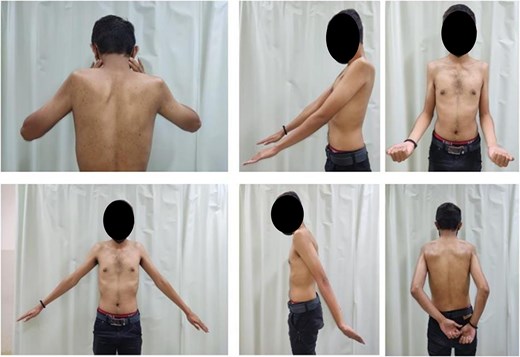
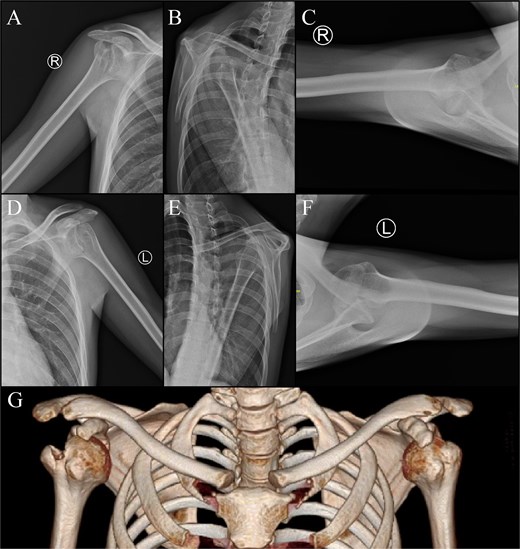
Imaging of the right shoulder : (A) anteroposterior view; (B) scapular Y view; (C) axillary view. Imaging of the left shoulder : (D) anteroposterior view, (E) scapular Y view, (F) axillary view. (G) 3D computed tomography scan.
The patient was then diagnosed with bilateral neglected closed fracture dislocation of proximal humerus Neer 2-part and underwent open reduction with GT osteotomy and PHILOS plate fixation. The right shoulder surgery was performed first, with the left shoulder procedure delayed by three months due to administrative constraints related to public healthcare insurance.
Surgical techniques and findings
The patient was positioned in a beach-chair position. After identification of the biceps and pectoralis major tendon, tenotomy, and tenodesis were performed, respectively. Fibrotic tissues and adhesions found in subcoracoid and subacromial area were then released. The GT, along with supraspinatus and infraspinatus tendons were identified, then GT osteotomy was done in a straight-line manner (Fig. 3). Posterior capsulotomy was performed for better visualization. The Hill-Sachs lesion and glenoid were exposed by lifting and internally rotating the arm, allowing removal of adhesions. After preparation of the glenohumeral joint, the humeral head was reduced using a Hohmann retractor. The GT was initially secured with temporary K-wires which was then confirmed with fluoroscopy before performing definitive fixation using a PHILOS plate [8]. Illustration of the technique is described in Fig. 4. If intraoperative assessment reveals a shortened or tightened subscapularis muscle, the K-wire can be retained for up to 3 weeks postoperatively to maintain adequate stabilization, as done in the left shouldercase.
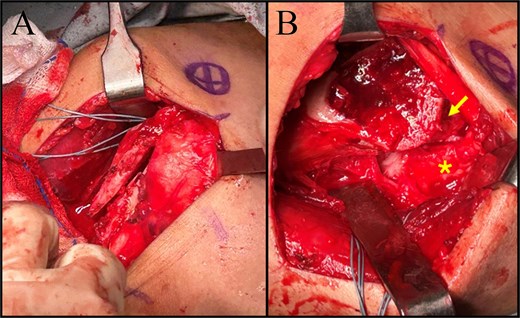
Intraoperative images. (A) Greater tuberosity osteotomy. (B) Exposed glenoid (asterisk) and Hill-Sachs lesion (arrow).
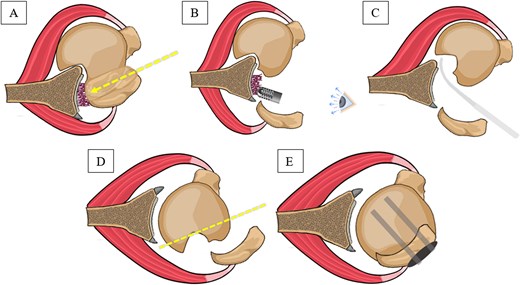
Surgical technique illustrations. (A) Greater tuberosity osteotomy to the old unreduced malunion fracture dislocation of proximal humerus. (B) Direct visualization to the posterior capsule, allowing accessible adhesion and fibrosis removal. (C) Humeral head reduction using levering mechanism. (D) Removal of the Hill-Sachs lesion. (E) Greater tuberosity fixation using proximal humerus internal locking system plate.
Outcome and follow-up
The patient was satisfied with the outcome, with normal activity regained 3 months after surgery. During the 1-year follow up of the right shoulder (Fig. 5), full ROM was achieved for flexion, extension, abduction, internal rotation, and external rotation (Table 1). Improvements of pain and functional score after 1 year was noticed with 0 visual analogue scale score, 100 The American Shoulder and Elbow Surgeons score and 0.8 disabilities of the arm, shoulder, and hand score. By the ninth month following the left shoulder surgery, improved ROM was noticed. Post-operative radiographic assessment of the right and left shoulders was conducted, as shown in Fig. 6.
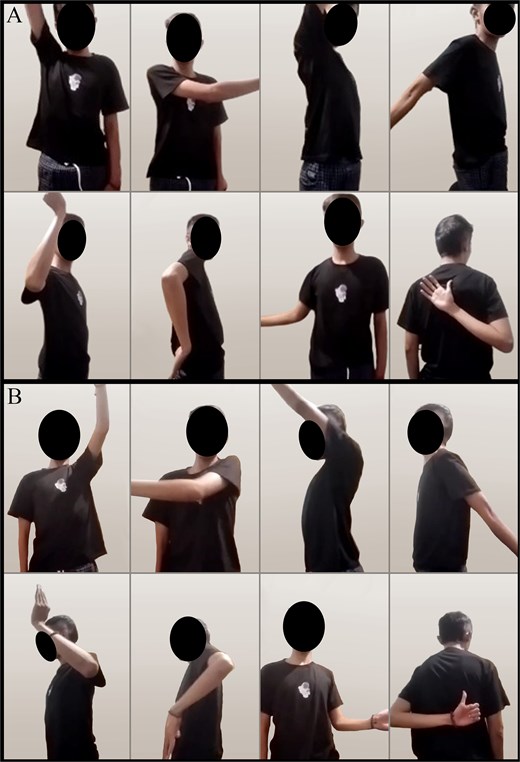
(A) Right shoulder range of movement 1-year post-surgery and (B) left shoulder range of movement 9 months post-surgery.
| Assessment tools . | Right shoulder . | Left shoulder . | ||
|---|---|---|---|---|
| Preoperative . | 1-Year follow-up . | Preoperative . | 9-Month follow-up . | |
| VAS | 6/10 | 0/10 | 5/10 | 1/10 |
| ASES Score | 27 | 100 | 15 | 57 |
| Dash Score | 76.7 | 0.8 | 76.7 | 17.5 |
| ROM | ||||
| Forward flexion | 0°–45° | 0°–180° | 0°–90° | 0°–150° |
| Backward flexion | 0°–30° | 0°–50° | 0°–30° | 0°–45° |
| Abduction | 0°–40° | 0°–180° | 0°–40° | 0°–130° |
| Internal rotation | Sacrum | T5 | Sacrum | T8 |
| External rotation | 0°–20° | 0°–90° | 0°–30° | 0°–45° |
| Assessment tools . | Right shoulder . | Left shoulder . | ||
|---|---|---|---|---|
| Preoperative . | 1-Year follow-up . | Preoperative . | 9-Month follow-up . | |
| VAS | 6/10 | 0/10 | 5/10 | 1/10 |
| ASES Score | 27 | 100 | 15 | 57 |
| Dash Score | 76.7 | 0.8 | 76.7 | 17.5 |
| ROM | ||||
| Forward flexion | 0°–45° | 0°–180° | 0°–90° | 0°–150° |
| Backward flexion | 0°–30° | 0°–50° | 0°–30° | 0°–45° |
| Abduction | 0°–40° | 0°–180° | 0°–40° | 0°–130° |
| Internal rotation | Sacrum | T5 | Sacrum | T8 |
| External rotation | 0°–20° | 0°–90° | 0°–30° | 0°–45° |
VAS, visual analogue scale; ASES, The American Shoulder and Elbow Surgeons; DASH, disabilities of the arm, shoulder, and hand.
| Assessment tools . | Right shoulder . | Left shoulder . | ||
|---|---|---|---|---|
| Preoperative . | 1-Year follow-up . | Preoperative . | 9-Month follow-up . | |
| VAS | 6/10 | 0/10 | 5/10 | 1/10 |
| ASES Score | 27 | 100 | 15 | 57 |
| Dash Score | 76.7 | 0.8 | 76.7 | 17.5 |
| ROM | ||||
| Forward flexion | 0°–45° | 0°–180° | 0°–90° | 0°–150° |
| Backward flexion | 0°–30° | 0°–50° | 0°–30° | 0°–45° |
| Abduction | 0°–40° | 0°–180° | 0°–40° | 0°–130° |
| Internal rotation | Sacrum | T5 | Sacrum | T8 |
| External rotation | 0°–20° | 0°–90° | 0°–30° | 0°–45° |
| Assessment tools . | Right shoulder . | Left shoulder . | ||
|---|---|---|---|---|
| Preoperative . | 1-Year follow-up . | Preoperative . | 9-Month follow-up . | |
| VAS | 6/10 | 0/10 | 5/10 | 1/10 |
| ASES Score | 27 | 100 | 15 | 57 |
| Dash Score | 76.7 | 0.8 | 76.7 | 17.5 |
| ROM | ||||
| Forward flexion | 0°–45° | 0°–180° | 0°–90° | 0°–150° |
| Backward flexion | 0°–30° | 0°–50° | 0°–30° | 0°–45° |
| Abduction | 0°–40° | 0°–180° | 0°–40° | 0°–130° |
| Internal rotation | Sacrum | T5 | Sacrum | T8 |
| External rotation | 0°–20° | 0°–90° | 0°–30° | 0°–45° |
VAS, visual analogue scale; ASES, The American Shoulder and Elbow Surgeons; DASH, disabilities of the arm, shoulder, and hand.
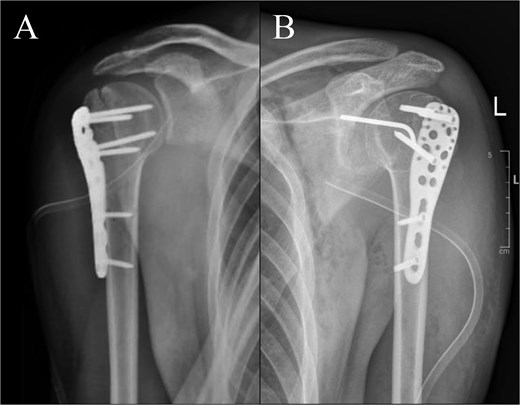
Post-operative radiographs: (A) right shoulder; (B) left shoulder.
Discussion
Neglected anterior shoulder dislocations are rare in the literature, making it challenging for clinicians to navigate the diverse surgical options and understand their long-term outcomes [6, 9–12]. With trauma as the main mechanism, anterior shoulder dislocation is frequently accompanied with bony injury such as Hill-Sachs lesions (38%–90%), GT fractures (12%–15%), and glenoid rim fractures (5.4%–11%) [13]. Reduction of the humeral head is commonly accomplished by laterally manoeuvring it through the rotator interval using a periosteal elevator. In a study by Dipit et al., complicated cases with GT fracture and/ or migration similar to ours, partial or complete tenotomy of the subscapularis was needed in order to achieve reduction [4]. With the critical stabilizing “sling effect” formed by the conjoined tendon and the subscapularis, the detachment of subscapularis produced anterior instability postoperatively and may cause further complications such as superior migration of the humeral head and glenohumeral arthritis [4, 10].
In this study, we performed GT osteotomy to achieve reduction by accessing the posterior compartment, which allows us to preserve the subscapularis. GT osteotomy offers enhanced visualization of the posterior humeral head and facilitates direct access to the glenoid, allowing for effective debridement of fibrotic tissue between the two structures. In neglected cases, there are often contracted posterior capsule, fibrotic tissues filling, and obstructing the view to the glenoid, which make visualization difficult [4]. Unlike reduction using a lever arm through a subscapular release, our technique minimizes complications such as iatrogenic fractures to the intact articular surface of the humeral head, which can occur when attempting reduction in cases involving a locking Hill-Sachs lesion combined with severe soft tissue shortening and arthrofibrosis [12].
Hill-Sachs lesion is often managed with bone humeral head augmentation, by filling the defect with grafts or soft tissue. Failure may occur with graft augmentation, and remplissage has the concern of infraspinatus shortening [14]. The use of GT osteotomy in this case allows for the modification of Hill-Sachs lesions by excising the indented portion and reconstructing the humeral head through reattachment of the osteotomized GT.
The patient’s final follow-up demonstrated improvements, comparable with those reported in prior studies [4, 15]. Our report presents satisfactory outcomes to the patient, however, further studies are needed to evaluate the effects of the technique in the long term and its applicability to cases with intact GT.
Conflict of interest statement
The authors declare that there is no conflict of interest in this study.
Funding
None declared.
Ethical approval
Written informed consent was obtained from the patient for publication of this case and accompanying images. No patient detail included in the manuscript of figures. Ethics approval was not required for this study.



