-
PDF
- Split View
-
Views
-
Cite
Cite
Özlem Okumus, Thomas P H Koester, Hafsa Kaman, Theresa Stork, Stéphane Collaud, Computer tomography-based three-dimensional reconstruction of an extended AB-thymoma: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf819, https://doi.org/10.1093/jscr/rjaf819
Close - Share Icon Share
Abstract
Thymomas are rare malignancies, constituting nearly half of anterior mediastinal tumors. We present a case of a large AB-Thymoma infiltrating adjacent structures. We evaluated computer tomography (CT)-based three-dimensional (3D) reconstruction to assess its utility in preoperative planning. The reconstructed images elucidated the spatial relationships between the tumor and surrounding structures and the findings from the reconstruction aligned with the surgical resection extent. Due to inherent imaging modality, the reconstruction had limitations in visualizing nerves and the pericardium. Nevertheless, 3D CT-based reconstruction of mediastinal tumors enhanced surgical planning by providing a detailed roadmap, facilitating preoperative discussions with patients, and serving as an educational tool for medical students.
Introduction
Mediastinal tumors most commonly arise from the anterior mediastinum [1]. Although thymomas are rare malignant tumors, they account for nearly half of the anterior mediastinal tumors. The World Health Organization (WHO) classifies thymomas into types A, AB and B (B1-B3 subtypes) based on the structure of the thymic epithelial cells (TECs), the ratio of non-tumoral lymphocytes, and their resemblance to the normal architecture of the thymus [2]. In advanced stages, infiltration of surrounding structures including great vessels and chest wall may occur [3]. Computed tomography (CT) is considered the gold standard in diagnostic, providing information on tumor size, characteristics, the relationship of the tumor to surrounding structures, and any possible pulmonary and/or pleural changes [4]. Surgery and complete resection are major prognostic factors in thymoma. An adequate assessment of the resectability of an extended thymoma is crucial [5].
CT-based 3D reconstruction is already established for surgical planning of pulmonary anatomic resection, especially segmentectomy for lung cancer. The European Society of Thoracic Surgeons (ESTS) highly recommends preoperative 3D reconstruction to obtain more information about tumor localization and the vascular anatomy of the segments [6]. When planning the resection of large mediastinal tumors, accurate assessment of tumor relationship to the surrounding structures is essential. 3D reconstruction softwares could be very helpful in this regard.
We hereby present a case of a patient with a large thymoma infiltrating neighboring structures and evaluate the benefits of a CT-based 3D reconstruction for surgical planning. Written informed consent for publication was obtained from the patient.
Case report
A 71-year-old female presented to her general practitioner with unintentional weight loss of 30 kg over the course of 6 months. She denied any further complaints. Her medical history included arterial hypertension and type II diabetes mellitus with no previous oncological history. Clinical examination revealed a cachectic patient without other relevant findings. A chest X-ray was performed as the initial imaging study, which showed an enlarged mediastinum (Fig. 1). In the case of a suspected mediastinal tumor, a chest CT scan was conducted and confirmed the presence of a 11.4 × 9.2 cm mediastinal tumor in the anterior mediastinum (Fig. 2). CT imaging revealed, in addition to the infiltration of the chest wall, a very close relationship with the aortic arch and the left subclavian artery. Further evaluation took place at a local hospital. First, an endobronchial ultrasound with transbronchial needle aspiration (EBUS-TBNA) of left paratracheal tumor mass revealed a B2 thymoma. Staging was completed with magnetic resonance tomography (MRI) of the brain, which excluded cerebral metastases. Due to suspicion of infiltration of the aorta, a complementary MRI of the mediastinum was performed but provided no additional information. The case was presented at a multidisciplinary tumor board in the presence of thoracic surgeons. The tumor was deemed inoperable and treated with four cycles of carboplatin and paclitaxel. At restaging, definitive radiotherapy was recommended. The patient sought a second opinion in our department. Re-staging with CT showed stable disease. The tumor was suspected to invade the sternum, left 1st to 3rd ribs, pericardium, and left upper lobe. Infiltration of the aorta appeared unlikely but could not be completely excluded.
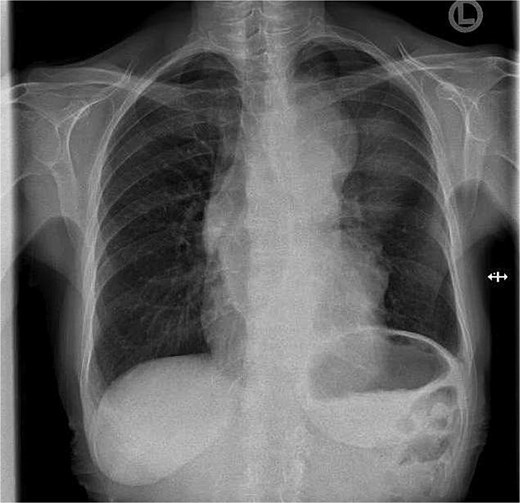
Chest X-ray at first presentation showing an enlarged mediastinum.

Chest CT in sagittal view showing a large tumor mass in the anterior mediastinum.
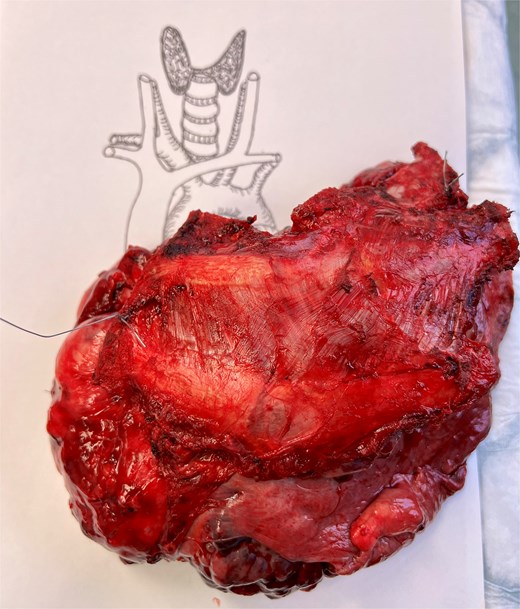
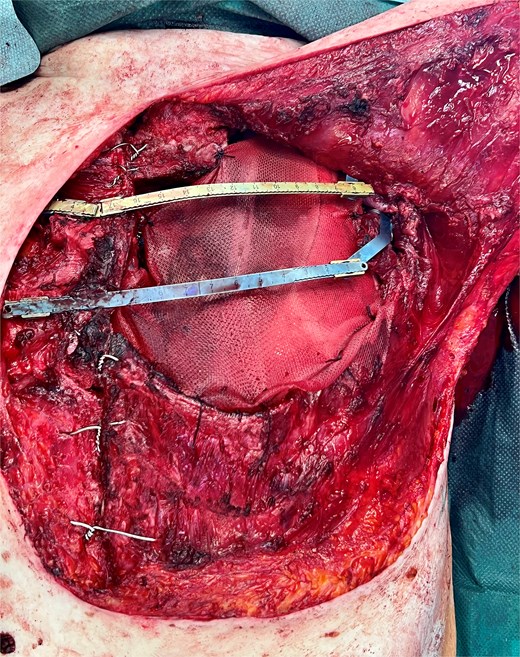
The patient was brought to the operating room for a median sternotomy including partial sternectomy. Exploration could exclude aortic infiltration. The incision was extended to a left hemiclamshell approach. Ribs 1 to 3 were prepared and cut laterally to the tumor. The left sternoclavicular joint was preserved. Further preparation was performed intrapericardially. The pericardium was sharply dissected and mobilized from the aorta and the pulmonary artery. Consequently, the ligamentum botalli was divided. The mammary vessels and the phrenic nerve were prepared and dissected with a safe distance to the tumor. Overall, an en bloc tumor resection was performed included extended thymectomy, partial resection of ribs 1–3, partial sternectomy, pericardectomy, left upper lobe lobectomy, and resection of the phrenic nerve and vagus nerve. A macroscopic view of the resected specimen is shown in Fig. 3. Subcarinal and hilar lymph node sampling was conducted. The chest wall was reconstructed with a vicryl mesh (ETHICON®) and titanium rib clips and bars (MedXpert®) (Fig. 4). Postoperative period was uneventful, and the patient was discharged on postoperative day 12. Histological examinations revealed an AB-Thymoma in Masaoka-Koga stage III with complete resection (R0). The patient was presented at our interdisciplinary tumor board, and adjuvant radiation was recommended.
Three-dimensional CT reconstruction with Mimics Planner (Materialize) was performed to explore its benefit in preoperative surgery planning. Mimics Planner is an interactive online surgical planning solution that utilize CT-based 3D models of the patient’s anatomy for lung resection planning. The AI-powered Mimics Medical (version 25) software was employed to convert CT images into detailed 3D models. A thorough review of the reconstruction images clarified the spatial relationship of the tumor to the neighboring structures. A very close relationship to the first three ribs on the left side and partially to the sternum was observed. In the lateral view, the encasement of the vessels and the bronchus of the left upper lobe is clearly visible. The course of the internal mammary artery through the tumor is also well depicted. The topographic relationship of the tumor to the aorta was reconstructed effectively. All the anatomical relationships of the tumor with its surrounding structures were confirmed intraoperatively.
Discussion
The assessment of the reconstruction images corresponds very well with the extent of the resection in the presented case. Images from various views of the reconstruction are shown in Fig. 5.
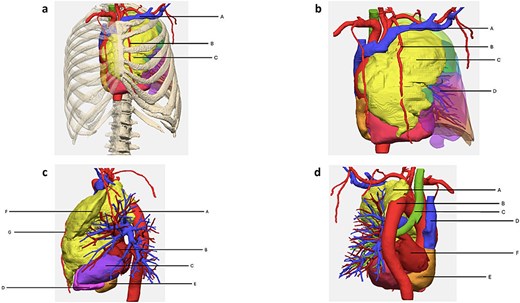
3D-reconstruction. (a) Anterior view with rib cage. A = vena subclavia; B = arteria mammaria interna; C = tumor. (b) Anterior view without rib cage. A = vena subclavia; B = arteria mammaria interna; C = tumor; D = lung. (c) Lateral view without lung. A = aorta; B = left atrium; C = left ventricle; D = right ventricle; E = right atrium; F = tumor; G = left arteria mammaria interna. (d) Posterior view with focus on aorta. A = tumor; B = aorta; C = trachea; D = vena cava superior; E = right atrium; F = left atrium.
Limitations of the reconstruction include depiction of nerves and pericardium; however, these limitations are due to the inability of the imaging modality to visualize these structures. In conclusion, three-dimensional CT-based reconstruction of mediastinal tumors and its surrounding structures allowed the surgeon to prepare a detailed roadmap for the operation. It also facilitated preoperative description of the extent of surgery to the patient as well as to medical students.
Conflict of interest statement
The corresponding author, Prof. Stéphane Collaud, reports receiving consulting fees from Materialise and Novocure, honoraria for lectures, presentations, educational events from Astra Zeneca and MedXpert and support for attending meetings and/or travel from Astra Zeneca, Intuitive and CMR Surgical. The authors declare that Materialise had no influence on data analysis, interpretation or manuscript preparation. The other authors declare no conlflict of interest.
Funding
This work was supported by Materialise, which provided the 3D reconstructions and covered the article processing charges.



