-
PDF
- Split View
-
Views
-
Cite
Cite
Mohamad M Khachab, Ali M Al Moussawe, Tiara Nabbout, Jana Warde, Hilda E Ghadieh, Ghassan Nabbout, Recurrent lymphangiomatous lesion of the chest wall and axilla in a young female: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf815, https://doi.org/10.1093/jscr/rjaf815
Close - Share Icon Share
Abstract
Lymphangiomas are uncommon, benign lymphatic malformations predominantly identified in infancy, with adult presentations being exceedingly rare—particularly when involving the chest wall and axillary region. We report the case of a 20-year-old woman presenting with a painless, progressively enlarging mass in the right axilla extending into the chest wall. Magnetic resonance imaging and computed tomography revealed a large, multiloculated cystic lesion compressing adjacent neurovascular structures. Notably, the patient’s history included resection of an oral lymphangiomatous mass during childhood, raising suspicion for a shared embryological origin. This case underscores the importance of considering lymphangiomas in the differential diagnosis of adult cystic masses and highlights the critical role of imaging in diagnosis and surgical planning.
Introduction
Lymphangiomas are rare, benign malformations of the lymphatic system, most commonly presenting as fluid-filled cysts involving the skin and subcutaneous tissues. They predominantly occur in the cervicofacial region but may arise anywhere in the body. Fewer than 5% of lymphangiomas are located in the axilla, chest wall, or mediastinum [1, 2]. While typically diagnosed in infants or young children, adult-onset lymphangiomas are uncommon and often represent recurrences or delayed manifestations of congenital malformations. Their variable and often ambiguous clinical presentations can complicate diagnosis, especially as they may mimic other soft tissue masses. Imaging modalities, particularly magnetic resonance imaging (MRI), are indispensable for accurate diagnosis and surgical planning. Here, we present a rare case of a recurrent lymphangioma in a young adult female involving the right cheek (in childhood), chest wall, and axilla, emphasizing the embryological considerations and challenges in management.
Case presentation
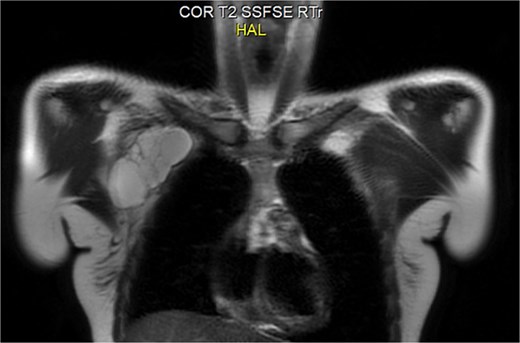
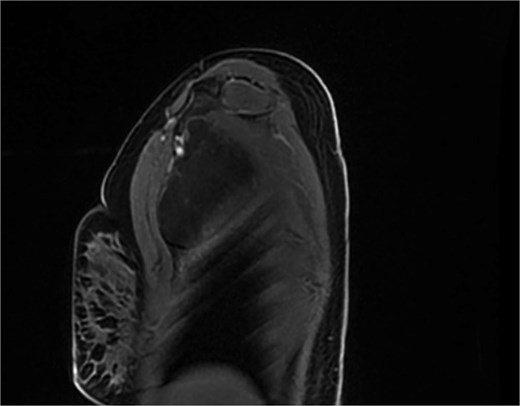
A 20-year-old previously healthy woman presented with a progressively enlarging, painless mass in the right chest wall extending into the axilla, associated with right arm heaviness, stiffness, and intermittent fatigue. She had a history of right cheek masses excised at ages 8 and 17, both histologically diagnosed as lymphangiomas. Examination revealed a large, soft, fluctuant, non-tender mass in the right axillary and lateral chest wall regions. MRI showed an 11.0 × 8.5 × 4.5 cm multiloculated cystic lesion with T2 hyperintensity and compression of the right axillary and subclavian veins (Figs 1 and 2). A diagnosis of recurrent cystic lymphangioma was established, and she underwent complete surgical excision with careful dissection to avoid neurovascular injury and management of lymphatic channels to reduce postoperative lymphocele formation. Postoperatively, her upper limb symptoms resolved, and she regained normal function. Given a recurrence risk of 10%–27% even with total excision, regular follow-up imaging was planned. This case underscores the need to consider lymphangiomas in adults with cystic masses, highlights the embryological explanation for ipsilateral recurrences along the cervicoaxillary pathway, and emphasizes the importance of MRI and computed tomography (CT) in diagnosis and surgical planning.
Discussion
Lymphangiomas result from congenital malformations of lymphatic channels due to failure of embryonic lymphatic sacs to establish normal venous connections. The jugular lymphatic sacs give rise to lymphatic drainage in the head, neck, and upper limbs [1, 2]. Residual embryonic lymphatic tissue along this pathway can explain ipsilateral recurrences, as in our patient, who presented with cheek lesions in childhood followed by axillary and chest wall involvement in adulthood.
While cervical lymphangiomas dominate pediatric presentations, adult-onset axillary and chest wall lymphangiomas are exceptionally rare [2, 3]. Symptoms often manifest only after significant enlargement causes mass effect on neurovascular structures, as seen in our patient’s arm weakness and heaviness. MRI is the modality of choice, demonstrating characteristic T2 hyperintensity and thin septations; CT adds value in delineating relationships with critical neurovascular structures for surgical planning [3, 4].
Surgical Excision remains the definitive treatment for symptomatic or functionally impairing lymphangiomas. Complete resection minimizes recurrence risk but may be challenging when lesions encase or abut neurovascular bundles, with reported recurrence rates reaching up to 50% following incomplete excision [5, 6]. Techniques such as partial decompression can improve intraoperative visualization [7].
Sclerotherapy, using agents such as OK-432, bleomycin, doxycycline, or ethanol, may be considered for unresectable or diffuse lymphangiomas [8, 9]. Macrocytic variants typically respond better to sclerotherapy than microcystic types [3, 5]. However, sclerotherapy often complements rather than replaces surgical intervention in adults due to limited efficacy and potential complications [10].
Surveillance is crucial given the risk of recurrence. Annual imaging or sooner if new symptoms arise is recommended. While syndromic associations (e.g. Noonan, Turner) warrant consideration in diffuse or recurrent cases, their absence here makes such diagnoses unlikely [6].
Adult lymphangiomas of the chest wall are exceptionally rare; most reported cases involve isolated, non-recurrent lesions [2, 3, 6]. Recurrences in anatomically distinct but embryologically related areas, as in our patient, are even less common. Misdiagnosis as lipomas or other benign masses is frequent, delaying treatment [2]. Imaging, particularly MRI and CT, is pivotal for diagnosis and operative planning [3, 4, 7]. While sclerotherapy shows promising results in children, surgical excision remains the standard in adults to confirm benignity and reduce recurrence risk [7].
Conclusion
This rare case of recurrent lymphangioma involving the ipsilateral cheek, chest wall, and axilla in a young adult underscores the embryological basis of lymphangiomatous spread along the cervicoaxillary continuum, the indispensable role of advanced imaging (MRI and CT) for accurate diagnosis and preoperative mapping, and the necessity of complete surgical excision to minimize recurrence, especially given the potential for neurovascular compromise [1–4, 7]. Clinicians should maintain a high index of suspicion for lymphangiomas in adults presenting with atypical cystic masses, particularly in patients with a history of prior lymphatic malformations, and multidisciplinary surgical planning with long-term follow-up is essential to detect potential recurrences in the same embryological field.
Conflict of interest statement
The authors have no conflict of interest.
Funding
No funding was used for this case report.



