-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Tarik Abdul Wahid, Zahraa Monjed Abdulghani, Nabeel Al-Fatlawi, Sajjad Ghanim Al-Badri, Lumbosacral posterior meningocele in adult patient: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf018, https://doi.org/10.1093/jscr/rjaf018
Close - Share Icon Share
Abstract
Spinal dysraphism is the incomplete fusion of the neural arch, which can be seen as an occult or open neural tube defect. Meningoceles are a form of open neural tube defect characterized by cystic dilatation of the meninges containing cerebrospinal fluid without the involvement of neural tissue. Neurosurgical intervention is necessary in the newborn period since survival in advancing ages is often impossible. Therefore, meningoceles are rarely reported in adulthood. Here, we discussed a case of a 23-year-old female who presented with a meningocele in the lumbosacral area since birth, which had not been operated on. Surgical management and intraoperative findings are also discussed.
Introduction
Spina bifida is the failure of closure of the posterior arch of the neural tube with or without herniation of neural tissue. There is a spectrum of conditions associated with spinal dysraphism, including spina bifida occult, spina bifida cystica (meningocele), and spina bifida aperta (myelomeningocele). Meningocele is a sac of meninges, covered by skin and containing cerebrospinal fluid (CSF) alone, herniates through an anterior or posterior bony defect [1].
The definite etiology of meningocele remains poorly understood. Most isolated neural tube defects appear to be caused by folate deficiency, likely combined with genetic and environmental risk factors such as advanced and young maternal age, low socioeconomic status, maternal alcohol use during pregnancy, smoking, caffeine use, obesity, high glycemic index, or gestational diabetes and maternal use of anti-seizure medications during pregnancy [2].
Meningocele results from a failure to develop the caudal end of the neural tube, resulting in a protrusion that contains cerebrospinal fluid, meninges, and overlying skin and does not have the spinal cord as its content [3].
Neurologic manifestations of the meningoceles depend on their size and location, including back pain, neurogenic bladder, paresthesias, and paraparesis. Other neurologic findings can include syringomyelia, Chiari I malformation, and hydrocephalus [4, 5].
To manage the complications of meningitis, meningocele cases should be operated on after birth, if possible, in the first 24 hours, especially when it is perforated. Here, we report a rare case of an adult meningocele patient who was not operated on in childhood [6].
Case presentation
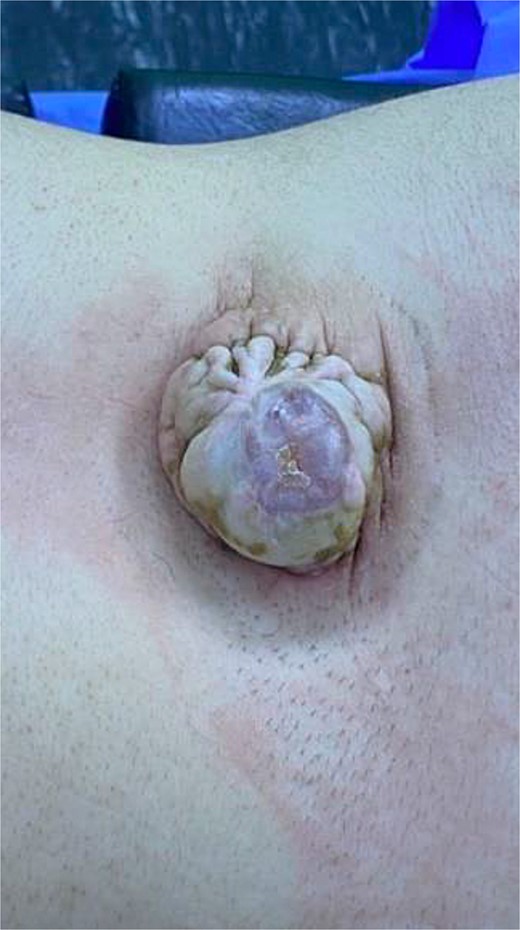
A 23-year-old female presented with severe local pain and local soft tissue infection. She reported a lifelong history of cystic swelling in the lower back, first noted at birth. Despite its presence, the patient had not sought medical attention previously, as significant symptoms had been absent until the current presentation. She now complained of severe pain at the site of the swelling, as well as redness, swelling, and warmth in the affected area. She denied any history of trauma, urinary or fecal incontinence, or progressive neurological symptoms. Her family and personal medical histories were unremarkable, with no known congenital anomalies or genetic conditions.
The patient was conscious, alert, and well-oriented on general examination, with stable vital signs. The affected area on the lower back showed erythema, swelling, and tenderness, consistent with a soft tissue infection. The neurological assessment revealed no motor or sensory deficits. She could stand and walk independently and exhibited normal urinary and bowel functions.
Local examination of the lower back revealed a 5 cm × 4 cm soft, cystic, midline mass located in the lumbosacral region. The mass was tender, with overlying skin showing signs of inflammation, including redness and warmth. There was no discharge or ulceration noted. Magnetic resonance imaging (MRI) of the spine identified a spina bifida defect at the L4-L5 level with a protruding meningocele sac containing CSF but no neural tissue involvement. The findings confirmed the diagnosis of a meningocele complicated by soft tissue infection (Fig. 1).
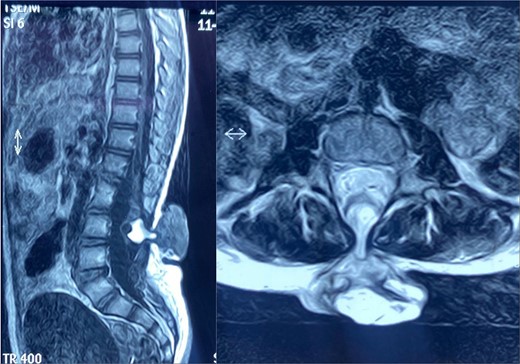
Sagittal (left) and axial (right) spinal MRI shows a meningocele sac.
The patient underwent elective surgical excision of the meningocele; the indication for surgery included the patient’s presenting symptoms of severe local pain and local soft tissue infection. The dura was opened during the procedure, revealing a lipomatous tissue inside the meningocele sac, which was carefully excised (Figs 2 and 3). The surgical site was then closed in layers, ensuring watertight dural closure to prevent CSF leakage. Postoperatively, the patient had an uneventful recovery. She reported complete resolution of her back pain and was able to lie supine comfortably. There were no immediate complications, such as wound infection, CSF leakage, or new neurological deficits. At follow-up, the surgical site was well-healed, and the patient expressed satisfaction with the cosmetic and functional outcomes of the procedure.
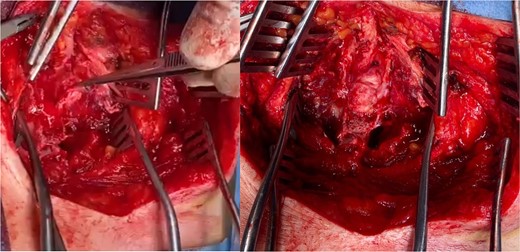
Intraoperative view demonstrates lipoma (the tip of the forceps in the left picture) and after removal of lipoma (right).
Discussion
A meningocele is a congenital anomaly of neural arch fusion in association with an open neural tube defect and characterized by protrusion of the spinal meninges, which contain CSF without involvement of the neural tissue [6, 7]. Most spinal meningoceles are found in the female gender in about three-quarters of cases [8]. the case presented is female, also conforming to most literature. Meningoceles are frequently located posteriorly over the lumbar and sacral areas at birth [9]. Our case also presented with a mass bulging from a defect in the posterior aspect of the fourth and fifth lumbar vertebrae since birth, conforming to most literature.
Spinal meningoceles often cause neurological deficits, skeletal deformities, anorectal and urinary bladder dysfunctions, paraplegia, and sensory loss below the cord level of involvement. The presented case did not have any neurological deficits. However, any meningocele patient who has deteriorating clinical symptoms such as progressive orthopedic deformities, lower extremity weakness, or urinary and fecal incontinence associated with low back pain should be considered a tethered cord. The case presented had a herniation tissue or lipoma discovered during surgical intervention at the site of the meningocele, which may predispose to the occurrence of tether cord syndrome.
Tethered cord syndrome is a rare neurological disorder where the spinal cord is attached, or tethered, to the tissues around the spine, this can limit its movement and cause tension, which can cause the spinal cord to stretch and may damage it and restrict blood flow to spinal nerves [9].
The degree of traction of the conus is thought to determine the age of onset of symptoms. In cases of marked tethering and severe stretching of the conus, neurological symptoms appear in infancy or early childhood. Minimal tethering may remain subclinical until adulthood [7]. About 29% of patients with symptomatic tethered cord are older than 35 years [10, 11], the case presented is 23 years old.
Direct trauma to the lumbosacral region may precipitate the symptoms, causing deformation of the marginally functioning neuronal elements within the stretched cord [12]. The bending movements, lithotomy position during childbirth, and movements occurring during motor accidents may precipitate symptoms [12, 13]. The presented case denied any trauma motor accidents, and she is not yet married.
Most meningoceles are surgically repaired during the newborn period or at least in childhood. The incidence of survival is low without intervention, so adult meningoceles are rarely seen.
Early surgical intervention is recommended in meningocele cases. Surgical repair aims to prevent neurological deficits, prevent infection, and for cosmetic purposes [14]. In the presented case, there was no obvious neurological deficit, but the patient had backache when she was lying supine, so she avoided lying on her back. However, symptoms subsided after surgical repair, preventing future neurological deficits, and a good cosmetic result was obtained.
Acknowledgements
Inapplicable.
Conflict of interest statement
No conflict of interest to report.
Funding
No source of funding was received.
Informed consent
Written informed consent was obtained from the patient for their anonymized information to be published in this article.
Ethics approval
Our institution does not require ethical approval for reporting individual cases or case series.



