-
PDF
- Split View
-
Views
-
Cite
Cite
James P Waters, Gena V Topper, Vineeth Romiyo, Ian P Hayden, Robert A Panico, David D Shersher, Open mesh repair of an iatrogenic post-nephrectomy Bochdalek hernia in an adult: a case study, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae696, https://doi.org/10.1093/jscr/rjae696
Close - Share Icon Share
Abstract
Bochdalek hernias arise from a developmental failure of the pleuroperitoneal canal to close, allowing abdominal contents to herniate into the thorax and compress the developing lung parenchyma. In rare cases, Bochdalek hernias may arise in adults and usually present with symptoms related to the hernia. Treatment consists of either open, laparoscopic, or robotic repair to close the defect. We present an unusual case in which an elderly patient presented with a large left-sided Bochdalek hernia containing both an incarcerated stomach and spleen following an uncomplicated robotic left nephrectomy. The hernia was successfully reduced and reconstructed with mesh via open abdominal repair with minimal complications. Repairing these hernias is challenging and, as in this case, required a complex reconstruction of diaphragm with mesh attachment to the ribs. Further reports on acute management of iatrogenic Bochdalek hernias in adults are warranted to better understand long-term post-operative outcomes and optimize management.
Introduction
Congenital diaphragmatic hernias are a rare condition with an incidence of 1 in 5000 live births and include several different subtypes [1]. Bochdalek hernias are the most common subtype and arise from a developmental failure of the pleuroperitoneal canal to close, allowing abdominal contents to herniate into the thorax and compress developing lung parenchyma. Due to earlier developmental closure of the left diaphragm, 85% of Bochdalek hernia cases are left-sided [2].
Bochdalek hernias are commonly diagnosed in early infancy or post-natal period. However, 0.17% to 6% of Bochdalek hernias may remain undetected into adulthood, and are either incidentally discovered on imaging or after presentation with pulmonary or gastrointestinal symptoms [3]. Adults may have precipitating factors leading to Bochdalek hernia, most often increased abdominal pressure from conditions such as pregnancy, severe coughing, or trauma [3]. Bochdalek hernias in adults may very rarely be iatrogenic, which has been detailed in a few case reports following a left lower lobe resection, a left colectomy, and a laparopscopic right nephrectomy [4–6]. To our knowledge, only one other case report of a Bochdalek hernia following nephrectomy has been published worldwide. Once diagnosed, surgical intervention is indicated due to the risks associated with herniated viscera such as cardiopulmonary compression, bowel incarceration, or intraabdominal organ dysfunction [2, 7, 8]. Treatment approaches consist of either open, laparoscopic, or robotic repair [9]. Anterolateral defects are easier to repair, thus minimally invasive approaches are preferred [10]. Although posterior defects may present anatomic difficulties, laparoscopic repair can be performed in hemodynamically stable adults.
We present a 69-year-old male who was diagnosed with a complex left-sided posterolateral diaphragmatic hernia following an uncomplicated robotic left nephrectomy requiring a robotic laparoscopy converted to open mesh repair.
Case report
A 69-year-old male with hypertension, hyperlipidemia, diabetes and a prior uncomplicated robotic left nephrectomy for renal cell carcinoma presented to the emergency room for evaluation of chest pain and emesis. He was uncomfortable, tremulous, and tachycardic with absent breath sounds over the left lower field. Initial CT scan showed a Bochdalek hernia containing distended stomach with left lower lobe collapse and transition to normal stomach at the level of the hernia (Fig. 1). Notably, the patient presented one month prior complaining of chest pain and abdominal discomfort that resolved with supportive care. CT scan at the time demonstrated a much smaller defect. At this visit, upper endoscopy showed viable gastric mucosa within the herniated stomach, but the hernia could not be traversed endoscopically.
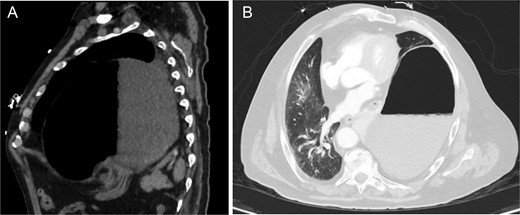
Pre-operative CT chest w/ contrast showing (A) large left Bochdalek hernia containing a large portion of distended stomach and (B) near-complete collapse of the left lower lobe with mediastinal shift.
Using robotic-assisted laparoscopy, significant adhesiolysis was performed throughout the superior abdomen to visualize the left diaphragm. The diaphragm was extremely thickened, and the hernia was difficult to reduce. Upon entering the chest through the diaphragmatic aperture, the patient became hemodynamically unstable, prompting repositioning and vasopressor support. The procedure was then converted to open repair via midline laparotomy.
After gaining exposure into the splenic sulcus, all attachments between the diaphragm, stomach, and spleen were circumferentially dissected. The stomach and spleen were reduced into the abdomen from the left chest. The diaphragm was then completely separated from the ribs posterolaterally. The diaphragmatic defect measured 8 × 8 cm. Due to the inability to close the diaphragm primarily without tension, an underlay piece of 2 mm Gore-Tex mesh measuring 10 × 10 cm with 2 cm of overlap on all sides was used. This was sewed to the closest rib posterolaterally and then to the edge of the diaphragm circumferentially via parachuted interrupted prolene sutures. Two 24-French chest tubes were placed into the left pleural space and abdomen towards the foregut.
The patient was kept intubated given his hemodynamic lability. His postoperative course was complicated by new-onset atrial fibrillation with rapid ventricular response that resolved with beta-blockade. On post-operative day (POD) 2, barium swallow study was negative for contrast extravasation (Fig. 2). After advancing to a mechanical soft diet and obtaining clearance from physical therapy, the patient was discharged home on POD 8 in good condition. On POD 21, he presented to clinic endorsing post-prandial nausea and occasional emesis. Follow-up CT scan with oral contrast showed no evidence of hernia recurrence or gastric distention, and demonstrated adequate gastric emptying and contrast progression to the colon. He was then transitioned back to a liquid diet. At the 1-month post-operative visit, he was doing well and was encouraged to advance his diet as tolerated.

Barium swallow status post left diaphragmatic hernia repair without evidence of leak or proximal obstruction.
Discussion
We present an unusual case in which an elderly patient with a large iatrogenic left-sided Bochdalek hernia was reduced and reconstructed with mesh via open abdominal repair. In 40% of these cases, the hernia sac will contain other viscera [11]. In cases where abdominal viscera become incarcerated or strangulated, there is a significant increase in risk of morbidity and mortality [12, 13]. In our patient, we successfully repaired the defect containing both an incarcerated stomach and spleen with minimal complications.
Minimally invasive surgery is preferred for repairing congenital diaphragmatic hernias [14]. However, due to hemodynamic instability intraoperatively, likely due to chronic comorbidities and hernia-related cardiopulmonary strain, open repair was necessary.
The hernia location along the posterior ribs was complicated and required mesh reconstruction of the entire posterolateral diaphragm. It is unclear why the patient developed this hernia many months after a left robotic nephrectomy. To our knowledge no iatrogenic Bochdalek hernias have been reported after a robotic procedure. Typically, adult-onset hernias present after a trauma; either acutely after abdominal contents herniation through a minor fascial defect, or they present late in patients who did not otherwise need surgical intervention initially, but had a delayed rupture of the peritoneal sac [11, 12, 15]. One potential etiology in our patient may have been a violation of Gerota’s fascia during the nephrectomy, creating a fascial separation between peritoneum and retroperitoneum, leading to herniation through a tiny congenitally present, now enlarged diaphragmatic defect. Alternatively, the defect may have occurred spontaneously after the nephrectomy and enlarged to accommodate intrabdominal organs.
Regardless of etiology, the approach to repair Bochdalek hernias is challenging and often requires a complex reconstruction of diaphragm with attachment of permanent mesh to the patient’s ribs. Further reports on management of Bochdalek hernias in adults are warranted to better understand long-term post-operative outcomes and optimize management.
Conflicts of interest statement
None declared.
Funding
None declared.



