-
PDF
- Split View
-
Views
-
Cite
Cite
Faris Alsobyani, Khadijah Alshakri, Hanin Mohammed Attar, Hatem Abada, Hassan Abu Rokbah, Conservative management in a spontaneous pneumoperitoneum post breast augmentation and abdominoplasty: a rare case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae814, https://doi.org/10.1093/jscr/rjae814
Close - Share Icon Share
Abstract
This case report discusses a 32-year-old woman with no significant medical history who underwent elective bilateral breast reduction with auto-augmentation and abdominoplasty. Initially, her recovery was smooth, but on the third postoperative day, she exhibited tachycardia, tachypnea, and mild shortness of breath, while other vital signs remained stable. A chest X-ray revealed pneumoperitoneum, and a subsequent abdominal CT confirmed moderate pneumoperitoneum without gastrointestinal leakage. Due to the lack of peritoneal signs and normal bowel sounds, conservative management was chosen. Over 2 days, her condition improved, and she was discharged without complications. This case emphasizes the need to recognize nonsurgical pneumoperitoneum after recent abdominal surgery and suggests that conservative management can be effective in the absence of perforation. This report is the first documented instance of spontaneous pneumoperitoneum following breast augmentation and abdominoplasty, highlighting the need for awareness in similar cases.
Introduction
Pneumoperitoneum, a feature usually associated with a hollow viscus perforation requiring an emergency surgery, can be in some instances nonsurgical or spontaneous [1–4], with conservative management being sufficient in these cases. We present a case report of a female who underwent an uneventful breast augmentation and abdominoplasty surgery who developed a spontaneous pneumoperitoneum and was treated conservatively.
Case report
This is a case of a 32-year-old female smoker and not known to have any past medical illness. The patient was admitted electively under the plastic surgery service in our hospital for bilateral breast reduction with auto-augmentation and abdominoplasty with plication of the recti. The operation was done smoothly without complications, and the patient had smooth postoperative course. On the third postoperative day, the patient was doing well and only had mild surgical site tenderness and mild shortness of breath. She is tolerating orally with no nausea and passed a bowel motion.
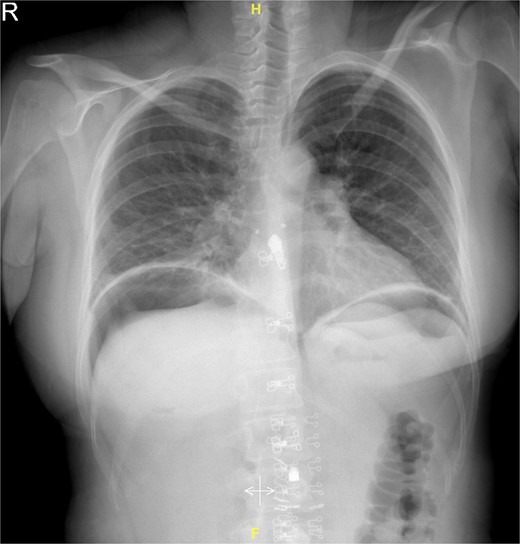
Upon examination, she had tachycardia and was tachypneic. However, the blood pressure, temperature, and oxygen saturation were within normal limit. The abdomen was soft and not distended, with mild surgical site tenderness. Surgical wound was clean and dry. Analgesia was given to the patient, but her vital signs showed no improvement. The hemoglobin (Hb) level was 9 g/dl, with the white blood cells (WBCs) count of 12 × 10%/l. Electrolytes, liver, and renal function tests were all within normal parameters. On erect chest film, there was air under the diaphragm (Fig. 1).
The general surgery team was consulted regarding the finding in chest X-ray film, and after assessment, an urgent abdominal computed tomography (CT) with intravenous, oral, and rectal contrast (Fig. 2A and B) was done showing a moderate amount of pneumoperitoneum as well as an extraperitoneal subcutaneous air foci was noted. However, the oral contrast is passing freely with no evidence of leak or extravasation.
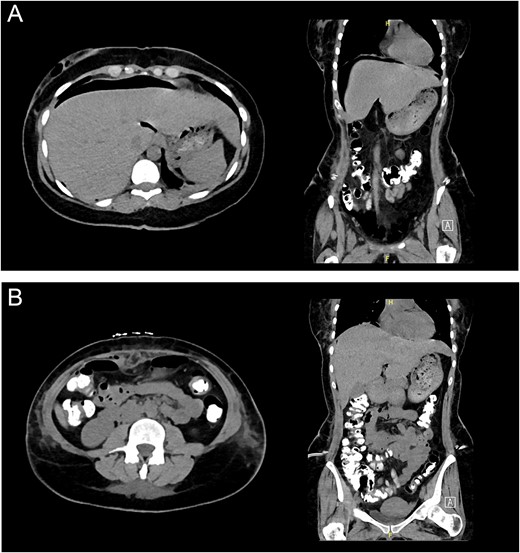
(A) Abdominal CT demonstrating subphrenic pneumoperitoneum. (B) Abdominal CT with triple contrast without any contrast extravasation.
A decision was made to proceed with conservative management. The patient was assessed in the following 2 days and was doing fine. The symptoms improved significantly, and he was discharged home.
Discussion
The most common cause of pneumoperitoneum is a hollow viscus perforation. A surgical laparotomy is typically necessary to treat this condition, with a few exceptions. Conservative management, however, might be enough in some individuals whose pneumoperitoneum is not brought on by a perforation. Awareness of unusual reasons behind pneumoperitoneum is necessary to prevent needless surgical intervention. This condition is known as “non-surgical pneumoperitoneum” [1, 2] or “spontaneous pneumoperitoneum without peritonitis” [3, 4].
In this case, vital signs are relatively normal with a slightly elevated pulse rate possibly due to pain at the site of surgery as indicated by patient complaining of pain at the incision site. Lack of peritoneal signs and the presence of normal bowel sounds also contribute to discounting the possibility of acute surgical abdomen. CT scan results also support this, showing the oral contrast passing through the gastrointestinal tract without leakage or extravasation and that may explain the presence of pneumoperitoneum.
Numerous factors have been linked to nonsurgical pneumoperitoneum [2, 5, 6], including oropharyngeal conditions like tonsillectomy and tooth removals; intraabdominal conditions like pneumatosis cystoides intestinalis, aerophagia, jejunal diverticulum, endoscopy, laparotomy, laparoscopy, pneumocholecystitis, dialysis of the peritoneum, and paracentesis; and gynecologic conditions like pelvic examination, postpartum knee–chest exercises, vaginal douching, oral-genital insufflation, tubal insufflation, and coitus after hysterectomy. In addition, there are instances of “idiopathic pneumoperitoneum,” where the etiology is uncertain.
The patient under presentation had a pneumoperitoneum, although the cause was not recognized. Despite the widespread belief that barotrauma is the root cause of this medical issue, the patient’s presentation included a rapidly growing pneumoperitoneum, a significant amount of free air in the abdominal region, lack of air in any of the other body cavities, and no previous record of barotrauma [7, 8]. While certain individuals with nonsurgical pneumoperitoneum are completely without symptoms and others might experience acute abdominal discomfort with minor peritoneal irritation, most patients with this condition complain of nonspecific abdominal discomfort and distention. Pain may arise only from distension of the abdomen, and irritation of the peritoneum may result from air [9]. Contrast-enhanced CT can predict the site of a possible perforation with 86% accuracy [10]. Conservative therapy is a simple choice for people with asymptomatic nonsurgical pneumoperitoneum, but it might be challenging to decide whether to use it for patients who have severe symptoms and peritoneal discomfort. Our experience indicates that individuals with idiopathic pneumoperitoneum can be handled conservatively regardless of whether they present with symptoms and signs of peritonitis. Sanchez et al. [11] suggested conservative therapy in symptomatic individuals with pneumoperitoneum when sufficient assessments have excluded a perforate viscus. Various established methods of treatment are in practice, including intravenous antibiotics, total parenteral nutrition, bowel rest, serial examinations, and imaging [10]. In conclusion, in situations of pneumoperitoneum lacking a perforated hollow viscus, cautious care seems to be the best course of action.
To our knowledge, there has not been a published case in the English literature discussing a similar presentation of spontaneous pneumoperitoneum post breast augmentation and/or abdominoplasty surgery.
Conclusion
This case report highlights the importance of recognizing nonsurgical causes of pneumoperitoneum, particularly in patients who have undergone procedures such as breast augmentation or abdominoplasty. The absence of signs indicative of acute surgical abdomen, coupled with imaging findings that rule out hollow viscus perforation, suggests that conservative management can be an appropriate approach in such scenarios. Given the diverse etiologies of nonsurgical pneumoperitoneum and the varied clinical presentations, it is crucial for healthcare providers to maintain a high index of suspicion and thoroughly evaluate each case. This awareness can prevent unnecessary surgical interventions and lead to more tailored patient management. Our findings contribute to the limited literature on spontaneous pneumoperitoneum, reinforcing the need for further studies to better understand this condition and its implications in postoperative care.
Conflict of interest statement
None declared.
Funding
The authors have received no assistance or funding for this paper and declare no conflicts of interest.



