-
PDF
- Split View
-
Views
-
Cite
Cite
Rahel Abebayehu Assefa, Henok Teklesilassie Zeleke, Dawit Gebregiorgis Debena, Simultaneous bilateral deep femoral artery aneurysms: case report of a rare peripheral arterial aneurysm, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae821, https://doi.org/10.1093/jscr/rjae821
Close - Share Icon Share
Abstract
Deep femoral artery aneurysms are very rare; particularly when isolated and occur simultaneously in both limbs. We report such a case of a misdiagnosed 16-year-old male presenting after hematoma evacuation was attempted for painful swelling in the left groin. Once the diagnosis was confirmed by computed tomography angiography (CTA), an emergency aneurysmectomy with deep femoral artery (DFA) ligation was performed on the left limb. Subsequently, an elective aneurysmectomy with DFA ligation was done for the contralateral limb during the same admission, with no postoperative complications. Echocardiography, performed with suspicion for infective endocarditis as the cause for possible mycotic aneurysm, revealed Chronic Rheumatic Valvular Heart Disease, without evidence of vegetations, abscesses, or intracardiac thrombi. This case report seeks to discuss the patient’s clinical presentation, CTA findings, and surgical management in a low-resource setting, underscoring the risks of this rare condition if misdiagnosed.
Introduction
Deep femoral artery aneurysms (DFAA), also known as profunda femoris aneurysms, are very rare, especially when isolated and occurring bilaterally. Only 0.5% of peripheral aneurysms are isolated DFAAs, representing 1 ± 2.6% of femoral aneurysms [1, 2]. DFAA commonly present with other aneurysms, necessitating investigation for concomitant aneurysms [1–3]. Due to high complication rate – including rapid sudden expansion, rupture, thromboembolism, and limb loss – prompt surgical intervention is crucial [4, 5]. Patients may present with atypical symptoms so a high index of suspicion is needed [6]. Doppler ultrasound, computed tomography angiography (CTA), and arteriography are valuable for diagnosis as well as assessing distal arterial flow and concomitant aneurysmal disease [3, 7]. Traditionally, aneurysmectomy and deep femoral artery (DFA) ligation was done to prevent thromboembolism, especially with patent superficial femoral artery and uncomplicated distal DFAA [4, 5, 7–11]. Recently, surgical reconstruction of the DFA using vein or prosthetic graft has become preferred even with patent distal flow [3–5, 8, 11]. Bypass may be required to address concomitant femoro-popliteal occlusions [11]. Although open, endovascular (trans-catheter coil embolization or stenting) and hybrid treatment options are documented, no standard approach exists due to rarity of DFAA [11–14].
Case presentation
A 16-year-old male presented to a rural hospital with a 1-year history of left groin swelling with progressive growth. The swelling became painful and suddenly increased in size one week prior to presentation. He had sustained blunt trauma to the upper thighs and fell over a metal bar prior to noticing the swelling. An initial surgery was attempted at the hospital to evacuate hematoma, but due to torrential bleeding, the wound was packed, and the patient referred for vascular intervention with an impression of femoral artery pseudoaneurysm.
Upon arrival at our facility, the patient was experiencing intermittent shortness of breath, easy fatigability, tinnitus and palpitation but no orthopnea or paroxysmal nocturnal dyspnea. Otherwise, he had no other pertinent history indicative of symptoms or risk factors for cardiovascular disease.
At presentation, he was febrile with tachycardia, tachypnea and borderline blood pressure. He had pale conjunctiva and a grade III holosystolic murmur at the apex radiating to the left lower sternal border. His left upper thigh was swollen with blood soaked surgical dressing. All distal pulses were palpable; motor and sensory function were intact in both lower limbs.
White blood cell count was 13,700 and hemoglobin was 3.4 mg/dl. CTA revealed bilateral DFAAs with the left measuring a maximal diameter of 9.32 mm with adjacent surgical pack pushing the vessels medially and a right concentric unruptured DFAA measuring 2.05 cm (Figs 1–3).
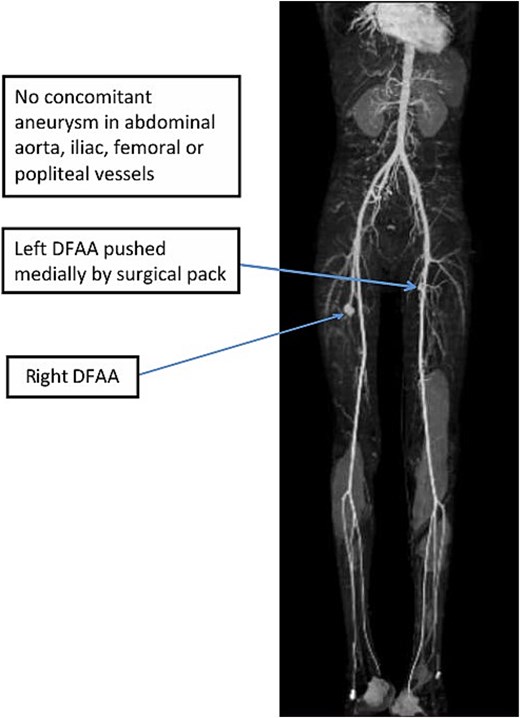
3D-maximum intensity projection frontal view of lower limb CTA showing bilateral DFAA.
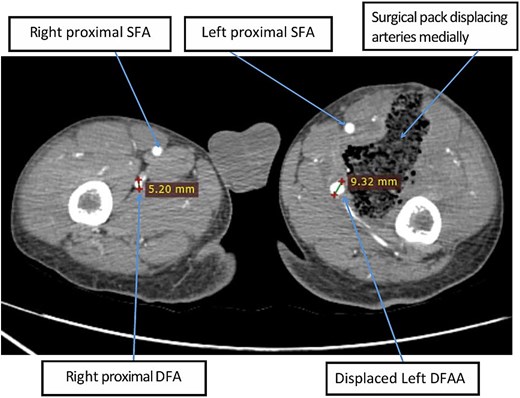
Axial image of lower limb CTA at the level of upper thigh showing left DFAA with maximal diameter of 9.32 mm (anteroposterior diameter of 8.58 mm) with adjacent surgical pack.
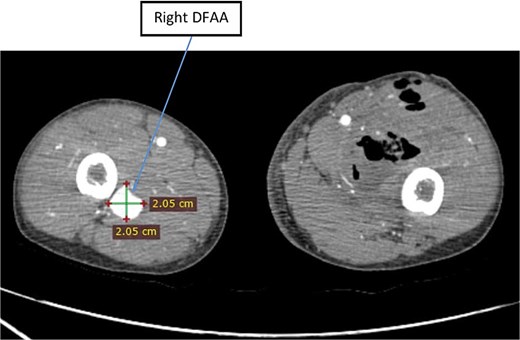
Axial image of lower limb CTA showing right unruptured DFAA with concentric aneurysmal sac.
The patient was resuscitated, given multiple transfusions, started on double antibiotics and hemodynamically stabilized with hemoglobin rising to 11.9 mg/dl. He was urgently operated with finding of minimal non offensive pus in gauze packed surgical wound, aneurysmal dilated left DFA with thinned out wall defect of the vessel, and necrotic surrounding muscles. Aneurysmectomy with proximal and distal DFA ligation was done along with debridement of necrotic tissue.
Postoperatively, further investigations were done with the suspicion of mycotic aneurysm (MA) secondary to infective endocarditis (IE); however, blood culture was negative, and echocardiography showed thickened and calcified mitral and aortic valve leaflets with moderate mitral and mild aortic regurgitation; no vegetations, abscesses, or intracardiac thrombi. With an additional diagnosis of Chronic Rheumatic Valvular Heart Disease, the patient was initiated on monthly Benzathine penicillin injections.
For the incidental finding of the contralateral DFAA, the patient’s guardians were advised on revascularization but, due to difficulty to continue follow up, they opted for ligation instead. The patient underwent elective aneurysmectomy with DFA ligation for the right DFAA on the 9th postoperative day. Intraoperative finding was a 2 × 2 cm aneurysmal dilatation of the right DFA. The patient had smooth postoperative course, and he was discharged after 2 days. The patient was lost from the follow-up thereafter.
Discussion
With a high index of suspicion, thorough physical examination of groin and extremity masses, noting pulsation or thrill, along with color flow study will diagnose peripheral pseudo or true aneurysms. In this case, the failure to check color flow within the mass led to a misdiagnosis, despite a history of incidental swelling after trauma and possibility of pseudoaneurysm.
Unavailability of endovascular therapies, poor health-seeking behavior, and a lack of follow-up in this patient mandated ligation over revascularization, a viable option in resource limited the setup.
Peripheral MA can rarely occur as a complication of IE [15, 16]. The spectrum of clinical findings in patients with MAs range from ‘acute catastrophic sepsis, to insidious, indolent infection’ [17]. In developing countries like Ethiopia, the diagnosis and treatment of IE and its complications can be challenging, and it is likely for cases of IE to be missed [18]. Although uncommon, MAs caused by bacterial endocarditis usually affect the superior mesenteric artery, followed by the aorta and femoral arteries. It can also occur after trauma in the extremity. Negative blood cultures occur in 18–50% of MA cases [19].
Several aspects of MA occurrence and management in IE patients remains under-researched with significant gaps in knowledge about risk factors, clinical presentation and outcomes [19]. In a study conducted over 14 years at a single center, only 10 out of 238 patients with IE underwent surgery for peripheral MAs [16]. Similarly, in a 13-year multicenter prospective study, out of 4548 definite IE cases, <2% (85 patients) developed MAs, of which 28.9% occurred in the lower limbs [19].
In our report, although there was no history of treatment for IE, considering the patients’ age, no underlying atherosclerosis, no risk factors for aneurysmal disease and echocardiography findings, there is a high suspicion for the etiology of the DFAA to be IE. Further research into the prevalence, causality, and surgical outcome of peripheral MAs in patients with IE is needed.
Conclusion
Due to the rarity of DFAA, misdiagnosis is likely if there is no high index of suspicion. Physical examination and color flow study of all masses in extremities are crucial. With the lack of proven standard of care, surgical treatment should be individualized based on the available setup and patient factors. Additional research is needed to identify the prevalence, causality, and outcome of IE with peripheral MAs.
Conflict of interest statement
None declared.
Funding
None declared.
References
- echocardiography
- bacterial endocarditis
- edema
- vegetation
- rheumatic disorders
- intracardiac thrombosis
- mycotic aneurysm
- profunda femoris artery
- aneurysm
- aneurysmectomy
- heart valve diseases
- abscess
- limb
- ligation
- pain
- surgical procedures, operative
- diagnosis
- groin
- arterial aneurysm
- computed tomographic angiography
- aneurysm, peripheral
- misdiagnosis



