-
PDF
- Split View
-
Views
-
Cite
Cite
Marco E Guerrero, Natalia A Lacouture, Ricardo Manzur Ayala, Thermal imaging for monitoring the treatment of hemangioma in pediatric patient: case report, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae536, https://doi.org/10.1093/jscr/rjae536
Close - Share Icon Share
Abstract
Pediatric hemangiomas are benign vascular malformations or angiodysplasias characterized by the proliferation of endothelial cells in blood vessels. Their incidence is 4%–10% in children under 1 year of age, and they most frequently occur on the head and neck [1, 2]. In addition to causing facial deformities, facial hemangiomas can lead to both functional and aesthetic issues, often resulting in significant complications. These complications negatively impact the quality of life for patients and can also affect the psychological well-being and self-esteem of their families [3]. With the expected global smartphone penetration reaching 70% [4], this case report explores the use of smartphones integrated with thermographic cameras to monitor the involution of hemangiomas during sclerosing treatment. This approach represents a promising advancement in managing and assessing hemangioma treatment through accessible, real-time monitoring technology.
Introduction
Congenital vascular malformations are developmental abnormalities that occur during the third week of gestation, characterized by structural and clinical polymorphism [5].
Pediatric hemangiomas (PH) are a specific type of benign vascular malformation characterized by the proliferation of endothelial cells in blood vessels. Although the exact incidence is unknown, estimates suggest that PH occurs in ~4%–10% of children under 1 year of age, and about 12% of these patients will require treatment. PH most commonly occurs on the head and neck (60%), followed by the trunk (25%) and extremities (15%) [2]. The presentation is associated with various prenatal factors such as maternal rubella, toxoplasmosis, use of certain drugs (e.g. thalidomide, cyclophosphamide), advanced maternal age, multiple gestation, and preeclampsia [5].
PH typically exhibits continuous growth, becoming more evident as the child ages. Initial lesions often present as pale or hyperpigmented areas with telangiectasias or ecchymosis, which can lead to misdiagnosis and delayed intervention [6]. The evolution of PH is generally described in three phases: the proliferative phase, followed by a period of stability or plateau, and finally, a phase of spontaneous involution, which usually begins around 1 year of age [7].
PH can be categorized based on depth into superficial and deep hemangiomas. Mixed hemangiomas, which appear later and tend to proliferate for a longer duration, typically exhibit both superficial components—responsible for the reddish color—and deep components—contributing to the volume of the lesion. Facial hemangiomas in pediatric patients can significantly impact function and cause severe deformities, with some cases potentially obstructing the airway. Therefore, each case must be individually assessed based on the size, type, and location of the lesion [7].
The integration of smartphones with thermal cameras offers a novel approach for distinguishing vascular malformations by detecting temperature variations, which helps in determining their location and size. This method provides a practical alternative to traditional imaging techniques such as Doppler ultrasound or tomography, which can be time-consuming and less accessible. Furthermore, it enables real-time monitoring of PH involution during sclerosing treatment [8].
Several sclerosing agents are available for treating venous malformations. These agents work by inducing vessel irritation and inflammation, leading to retraction and scar formation, which reduces the vessel’s caliber, causes necrosis, and decreases lesion size [9]. Effective sclerotherapy requires precise dosing and uniform distribution of the sclerosant over the entire endothelial surface of the vessel or hemangioma lacuna. The sclerosant must remain in contact with the endothelium for a sufficient duration to achieve the desired therapeutic effect [10]. However, standardization of dosage and concentration remains challenging due to the functional and morphological variability of the lesions [10].
Case presentation
A 6-year-old female patient presented to the outpatient plastic surgery service at Queen Catalina Clinic in March 2022, accompanied by her mother. The patient had a 6-year history of a mass on the left hemiface, which initially manifested as a hyperpigmented area on the cheek and subsequently expanded, leading to significant deformity of the affected hemiface (Fig. 1).

Photograph provided by the patient’s mother at 6 months of age, showing a hyperpigmented area on the left cheek and a mild deviation of the left nasal ala.
The vascular lesion resulted in occlusion of the left eye, deviation of the left nasal ala, and enlargement of the left cheek (Fig. 2).

Photograph taken during the patient’s initial evaluation at our clinic at 6 years of age, revealing severe deformation of the left hemiface with significant involvement of the left cheek and upper eyelid.
A CT scan revealed a hemangioma localized in the left upper eyelid and zygomatic region. The patient’s medical history was otherwise unremarkable. Due to the case’s complexity, surgical options were deemed unsuitable, and the patient was referred to palliative care services. The pediatric and anesthesiology teams endorsed sclerotherapy as a suitable treatment to reduce the size of the malformations.
Sclerotherapy was administered using Monoethanolamine Oleate at a concentration of 0.5 g/ml. Lesions were infiltrated based on the mapping provided by thermal imaging. A total of eight sclerotherapy sessions were performed. The sclerosants were diluted to 0.05 g/ml in 3 ml for the upper eyelid (3:1 dilution) and to 2 ml (2:1 dilution) for the left malar region. An insulin syringe was used to inject the sclerosant into the deepest areas of the lesions to prevent necrosis of adjacent tissues [9]. Thermographic imaging demonstrated a reduction in lesion size, enabling effective monitoring of treatment progress (Figs 3 and 4).
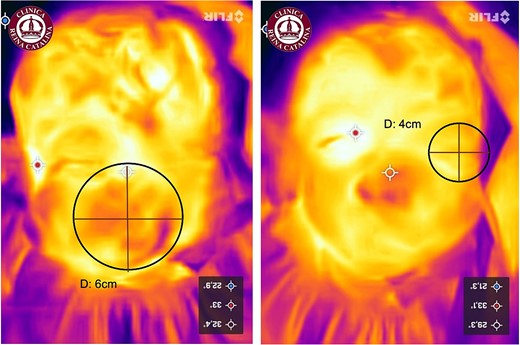
Thermographic image of the pediatric hemangioma highlighting the areas affected by the hemangioma. The blue regions indicate areas with lower temperatures. Left: Diameter of the left cheek hemangioma (6 cm). Right: Diameter of the upper eyelid hemangioma (4 cm). Note: Images were taken at the first encounter.

Intraoperative photograph showing the injection of the sclerosant (Ethamolin) into the left upper eyelid and left cheek.
Thermal imaging was conducted from a distance of 30 cm from the skin after applying an ice pack to delineate the affected areas, which retained cooler temperatures longer due to the hemangioma. Measurements of the affected areas were taken at two stages: before and the day after the intervention. In vivo measurements were recorded using a metric tape and entered into the database.
Weekly follow-ups were performed to evaluate changes in the size, appearance, and dimensions of the lesions.
Results
We demonstrate that sclerotherapy can be effectively monitored using thermal imaging, proving it to be safe, noninvasive, and effective in reducing the size of infantile hemangiomas. In the case presented, we performed a total of eight sclerotherapy sessions to facilitate lesion involution, with intervals of 7 days between sessions, under sedation in the operating rooms of our institution. This approach was chosen to minimize patient discomfort and pain during the initial 56-day treatment period. Each session involved the administration of a full ampoule of Ethamolin (0.05 g/ml), diluted in 3 ml for the upper eyelid and 2 ml for the left malar region. Treatment may result in edema, local bleeding, and pain in the treated area, which typically subsides within 1–3 days following the sclerosing agent infiltration (Figs 5–7). As shown in the photographic sequence, the diameter of the hemangioma decreased by 1 cm in the upper eyelid and 2 cm in the left cheek after eight sessions of sclerotherapy. Additionally, the cool spots observed during the initial evaluation demonstrated a significant reduction in the hemangioma’s size.
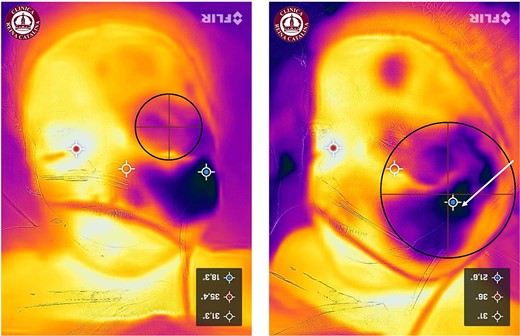
Thermographic monitoring of the pediatric hemangioma, showing marked areas indicating hemangioma lacunae prior to the placement of ice packs. Left: upper eyelid; Right: left cheek. The white arrow highlights the center and the largest affected area. Note: Images taken before the initiation of sclerotherapy.
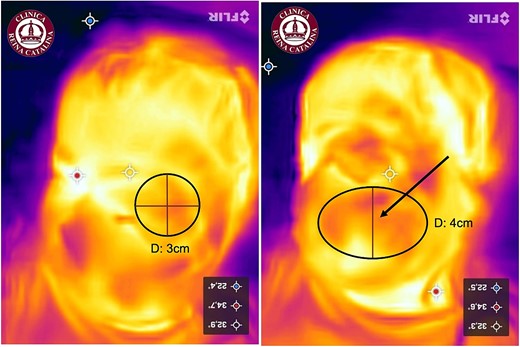
Thermographic monitoring of the pediatric hemangioma after six sclerotherapy sessions, demonstrating a reduction in the diameter of the lacunae. Left: upper eyelid, showing a 1-cm reduction in diameter. Right: left cheek, showing a 2-cm reduction in vertical diameter while maintaining the transverse diameter, transitioning from a round to an ovoid shape.
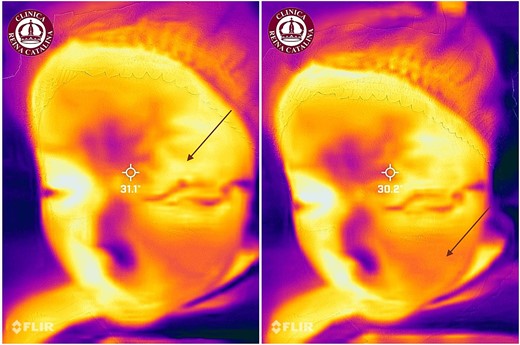
Thermographic monitoring of the pediatric hemangioma following eight sessions of sclerotherapy, showing decreased cold uptake and retention in both the upper eyelid and left cheek regions.
Discussion
This case was evaluated by other specialties, which did not recommend management due to a high risk of complications. In our service, a sclerotherapy protocol was initiated along with thermal monitoring to assess the involution of the hemangioma. Preoperatively, and prior to the infiltration of the intralesional sclerosant, thermal imaging was conducted using the FLIR ONE pro® camera coupled with a smartphone (iPhone®). This involved ensuring the skin was dry and capturing images from ~30 cm away. Ice packs were applied until a uniform cooling effect was observed. After removing the ice packs, images were taken to identify hot spots and cold spots, which marked the locations of the vascular and venous lacunae. These areas were identified by the camera as blue regions, indicating prolonged cold retention [8].
Ethamolin induces irritation of the endothelial lining of the vessels and elicits an inflammatory response, leading to subsequent involution and fibrosis of the hemangioma [9].
Given its availability, long-term safety, and efficacy in our setting, Ethamolin helps facilitate hemangioma involution. This approach allows us to assess the need for surgical resection after the hemangioma has decreased in size. It is important to note that while the sclerosant can cause serious complications such as hemolysis, renal failure, skin ulcers, and hypersensitivity reactions, it enables patients to resume their normal activities within a few hours posttreatment. The concurrent use of thermal imaging provides enhanced control over hemangioma involution, offering a fast and reliable means to evaluate treatment effectiveness and determine the appropriate timing for potential surgical intervention (Fig. 8).

Photographic comparison of the patient. Upper: frontal and lateral views at the initial consultation. Lower: frontal and lateral views after eight sessions of sclerotherapy, illustrating significant improvement in the hemangioma, particularly in the left upper eyelid with increased ocular opening and improved vision, along with minimal but clinically significant reduction of the zygomatic lesion.
Conclusions
Sclerotherapy with ethanolamine oleate, when guided by thermal imaging monitoring, is both effective and safe for the treatment of infantile hemangiomas. However, multiple infiltrations may be necessary in some cases. Further research with larger and more extensive studies is recommended to establish the full efficacy and optimal application of this treatment and monitoring options.
Conflict of interest statement
None declared.
Funding
None declared.
Informed consent
Written consent was obtained from the patient’s mother for the use of images for educational purposes.
References
Carriles RM. Chapter 78 - Malformaciones vasculares y tumores vasculares. In:



