-
PDF
- Split View
-
Views
-
Cite
Cite
Maimuna Ibrahim, Alfred Chibwae, Benard Magoda, Ayubu Philipo, Shafii Ramadhan, Mohamed Salim, A road to surgical success: a case report of huge retroperitoneal idiopathic non-pancreatic cyst in a 6-year-old child at tertiary hospital, Muhimbili National Hospital, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae552, https://doi.org/10.1093/jscr/rjae552
Close - Share Icon Share
Abstract
In most reported cases, pancreatic pseudocysts are the most commonly reported cases and mostly occur in adults. Idiopathic non-pancreatic pseudocyst is rarely reported among children. We are reporting a rare case of retroperitoneal pseudocyst in a 6-year-old male with a 4-week history of abdominal swelling. He had asymmetrical abdominal distention on the right lumber and iliac regions with a smooth surface measuring 12 × 22 cm in its largest dimension. CT scan showed a mesenteric cyst, ipsilateral hydronephrosis, and intrahepatic duct dilatations. Intraoperatively, a retroperitoneal cystic mass was completely excised histologically confirmed pseudocyst. The patient was discharged home after fully recovery after 4 days of surgery. Surgical interventions remain to be the stay management of retroperitoneal pseudocysts with an earlier full recovery. Open surgical technique remains to be a preferred approach, especially for the large and complex retroperitoneal cysts.
Introductions
Retroperitoneal non-pancreatic pseudocysts are rare lesions that originate in retroperitoneal spaces [1]. Retroperitoneal space is divided anatomically into three parts: anterior pararenal retroperitoneal space, pararenal retroperitoneal spaces, and perirenal retroperitoneal spaces [2]. Primary retroperitoneal pseudocysts are diagnosed as a diagnosis of exclusion once they are confirmed that they are located in retroperitoneal space and do not originate from any retroperitoneal organ [3, 4]. The diagnosis of retroperitoneal pseudocyst is commonly reached with the help of imaging studies, and in most cases as an incidental finding during ultrasonography or CT scan studies [3]. In most reported cases, pancreatic pseudocysts are the most commonly reported cases and mostly occur in adults. Idiopathic non-pancreatic pseudocyst is rarely reported among children [4].
There is no known pathogenesis of most of the retroperitoneal pseudocysts, however, pseudocysts are defined by the accumulation of the unabsorbed fluids in retroperitoneal spaces lacking epithelial lining within the retroperitoneal spaces [5]. Most of the retroperitoneal pseudocysts have no specific presentations and have vague presentations [5, 6]. Most of the studies have reported abdominal pain and abdominal distension as the most common presentations. Retroperitoneal pseudo cysts can grow to be large enough to compress the adjacent structures [7]. Pain becomes the most presenting complaint when the pseudocyst becomes infected. Our current case report aimed at presenting a pediatric patient with retroperitoneal pseudocyst successfully cured after surgical excision.
Case presentation
We reviewed a 6-year-old male presented with a 4-week history of abdominal swelling more on the lower right abdomen. It was of gradual onset and progressive increase in size with the feeling of heaviness in the abdomen and early satiety. No history of change in the frequency of micturition habits, and no change in bowel habits. There was no history of fever, excessive night sweats unintentional weight loss, or history of living with TB patients.
On examination, he was fully conscious and well-nourished with vital signs within the normal limits. He had asymmetrical abdominal distention on the right lumber and iliac regions with the umbilicus centrally located and inverted (Fig. 1). He had a palpable nontender mass at the right lumbar and iliac regions, irregular in shape, firm with smooth surface ~12 × 22 cm in its largest dimension. Liver and spleen were not palpable and kidneys were not ballotable. Normal bowel sounds with no vascular bruits. Full blood counts, renal function test, coagulation profile, serum amylase, and lipase were within the normal ranges.

Black arrows show asymmetrical abdominal distension on the right lumber and iliac regions.
Contrasted abdominal pelvic computed tomography was done. A large well-defined homogenous enhancing cystic mass lesion with internal septations and lobulated with outlines of peritoneal cavity extending from the below right renal inferiorly to the mid of the lower abdomen. Occupying the right iliac fossa and reaching the pelvis. It measured 13.1 × 15.5 cm with ipsilateral hydronephrosis and mild intrahepatic duct dilatations. The pancreas and the spleen appear normal, left kidney has normal size shape and secretory functions. Paraaortic regions are normal. The bowel loops are unremarkable. Urinary bladder appears normal (Fig. 2).
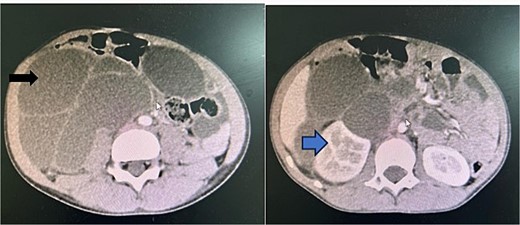
A contrasted preoperative abdominal pelvic computed tomography Image with IV contrast. The black arrow shows an intraabdominal multiseptated fluid cyst. The blue arrow shows hydronephrosis of the right kidney as the result of the pressure effect of the mass.
Intraoperatively, a retroperitoneal cystic mass with bowels adherent to the mass was identified (Fig. 3). Massive right hydroureters and hydronephrosis with encased right ureters in the inferior surface of the kidney and para-aortic lymph nodes. Bowels were reflected to the left from the tumor and enucleation of the tumor was done from the peritoneum (Fig. 3) right kidney, right ureter, and right psoas major. Chocolate colored fluid ~1200 ml drained. A complete resection of the cyst was done. The right kidney and ureter were freed from the tumor. Peritoneal washing with warm saline was done and the abdomen closed in layers. Hemostasis achieved. Tissue submitted for histopathological studies. The patient was available for follow-up after 14 days after discharge and then after six weeks with no features of recurrence.
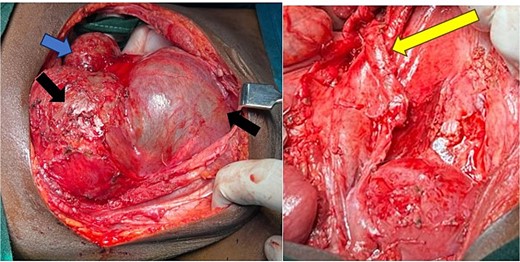
Intraoperative image, black arrow shows a mass after reflection of the adherent bowels from the tumor. Blue arrow showing a right kidney with hydronephrosis. The yellow arrow shows a dilated ureter post cyst excision.
Histological sections from the cyst show absence of the lining epithelium, the wall of the lesion is composed of fibrous tissue, congested blood vessels, edema, and aggregates of mononuclear inflammatory cells (A). These inflammatory cells were predominantly lymphoplasmacytic infiltrates (B and C), with no features of malignancy, granulomas, or necrosis. From these findings, the lesion was concluded as a benign inflammatory pseudocyst due to the absence of the lining epithelium (Fig. 4).
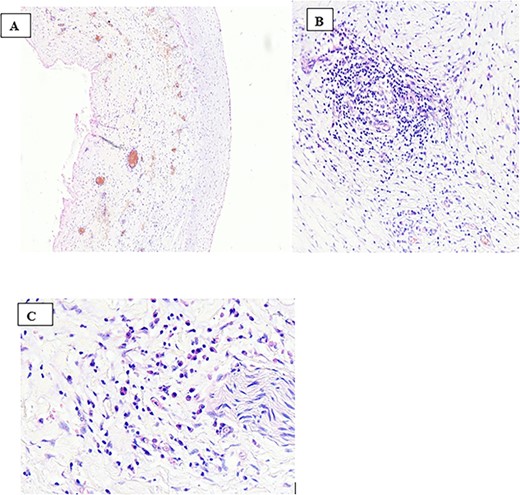
Histological sections from the cyst (haematoxylin and eosin stain ×100 (A), ×200 (B) and ×400 (C), respectively) showing the absence of the lining epithelium with a wall of the lesion composed of fibrous tissue and congested blood vessels, edema and aggregates of mononuclear inflammatory cells (A). These inflammatory cells were predominantly lymphoplasmacytic infiltrates (B and C) with no features of malignancy, granulomas, or necrosis.
Clinical discussion
From the literature, the pancreas is the commonest origin of the retroperitoneal pseudocyst, especially to adults, and as a complication of pancreatitis. Nonpancreatic pseudocysts are rare. There are also limited case reports for the retroperitoneal pseudocyst among children in the literatures [8]. In most retroperitoneal cysts, neoplasm cystic lesions have been reported to be rare and most of the cystic masses are benign. However, still there is a great challenge in distinguishing between malignant cystic lesions and benign lesions as there are no specific symptoms and signs to differentiate.
Computed tomography and magnetic resonance imaging studies are standard diagnostic tools for retroperitoneal pseudocyst investigations. However, they cannot give a definitive diagnosis for the retroperitoneal pseudocysts. There are also challenges in the radiological diagnostic approaches. As for most of the reported cases, radiological imaging studies could not be able to rule out malignant lesions from the benign cystic retroperitoneal lesions. This has an impact on the decisions and plan of management [9]. The current case as well had a radiological dilemma in ascertaining the accurate origin. However, radiological investigations are of importance in providing information on the status of the adjacent structures and give the road map of the resectability of the tumor and so the success of surgical excision.
The origin of the tumor in our current case could not be ascertained radiologically and was presumed to be mesenteric cysts. The mass was big enough to cause the compression of other surrounding structures including the right ureter and right kidney that were evidenced by radiological studies and intraoperatively. Although retroperitoneal pseudocysts are commonly asymptomatic, they are reported to be large enough and compress the adjacent structures [7].
Surgical excision is dependent on the definitive diagnosis histologically and the retroperitoneal pseudocyst is confirmed by the absence of an epithelial lining of the cysts [5]. This is how it was confirmed in our current case presentation. Surgical excision of the retroperitoneal cyst remains to be a mainstay and definitive management. In most of the literature reviewed reported cases, surgical management had the best outcomes. In our present case report, the child had a full recovery after surgical excision of the lesion.
Approaches for the surgical management of the retroperitoneal cyst includes open surgical approach which is the most preferred over laparoscopic, especially for symptomatic and large masses of >6 cm [1, 10]. The experience of laparoscopic excision of the retroperitoneal pseudocyst is limitedly reported [1, 10]. In the present case, the mass was larger than 6 cm and intraoperatively there were multiple bowels adherent to it and it also involved the right kidney, right ureter, and psoas muscles. This could impair the success of the laparoscopic excision with increased risk for intraoperative complications.
Conclusion
Retroperitoneal pseudocysts are rare, especially in children, and in most cases are missed both clinically and radiologically. Histological results are the definitive diagnostic investigations after surgical excisions. Surgical interventions remain to be a mainstay approach for both diagnostic and therapeutic purposes. A complete surgical excision is recommended with an earlier full recovery. Open surgical technique remains to be a preferred approach, especially for the large and complex retroperitoneal cysts.
Acknowledgements
The authors would like to thank the whole pediatric surgery team for the total support on the pediatric surgical patient care including the patient presented in this report. We extend our gratitude to the Head of Surgery Department at Muhimbili University of Health and Allied Sciences, Dr Ally Mwanga for his mentoring and constant support to make this publication possible.
Author contributions
M.I.: Study concept, writing the paper. A.C.: Study concept, Literature review, writing the paper. B.M.: Assistant Surgeon. A.P.: Pathological slide review. S.R.: Review of pathological slides and reporting. M.S.S.: Primary surgeon and overall study Supervisor.
Conflict of interest statement
The authors declares that there are no competing interests.
Funding
None declared.
Data availability
This is not applicable to this article because it is a case report.
Disclosure
This case report has been published in accordance with the SCARE Criteria [11].
Ethical approval
This case study was exempt from the ethical approval at our institution as this paper reports a single case that emerged during normal surgical practices.



