-
PDF
- Split View
-
Views
-
Cite
Cite
Yazeed Alshaalan, Thamer Althunayan, Fahad Alwadi, Mohammed Alessa, Sheikh Waheed, Oropharyngocutaneous fistula—a case report of conservative management in a diabetic patient, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae526, https://doi.org/10.1093/jscr/rjae526
Close - Share Icon Share
Abstract
Oropharyngocutaneous fistula following deep neck space infections is a rare entity. Patients can present with feeding difficulty and food leakage through the wound. The fistula is suspected to have formed not only due to the infectious process but also due to the combination of transoral and transcervical approach. Infection eradication, aggressive wound care, control of risk factors, and strict NPO with NGT feeding are all important parts of management.
Introduction
Oropharyngocutaneous fistula is an abnormal communication between oropharynx and skin. It might occur following tumor resection in the upper aerodigestive tract. However, its development following deep neck space infection is rare. Several risk factors might increase the risk of development of fistula including medical comorbidities such as diabetes [1]. Fistula Patients will not only suffer from feeding difficulties and extended hospital stay but also local wound complications [2].
This article will describe the development of oropharyngocutaneous fistula and its management in a young diabetic patient after an odontogenic deep neck space infection.
Case presentation
This is a 26-year-old male known to have diabetes mellitus on metformin. He presented to another hospital with neck swelling, odynophagia, and fever for 3 weeks. He was admitted there as a case of an odontogenic infection. Contrasted CT neck showed a left parapharyngeal abscess, so incision and drainage was done by maxillofacial team utilizing a left trans-cervical approach with removal of affected teeth with daily dressing of the wound. A repeated CT neck was done due to worsening of the patient condition with persistent discharge from the neck wound, which revealed a residual collection with extension into left peritonsillar space for which peritonsillar space incision and drainage was done by otolaryngology team while maintaining the patient on IV antibiotics. Hospital stay was complicated with multiple intubations. First intubation was for airway safety due to the abscess even though the patient was not in severe respiratory distress. Reintubation was then done as patient had severe agitation requiring sedation. General status of the patient worsened as he developed ventilatory acquired pneumonia. Cultures from neck wound showed Streptococcus Sanquis. Bronchoalveolar lavage samples showed Stenotrophomonas maltophilia and Candida tropicalis, and virology showed low positive titer of Cytomegalovirus. Patient was kept on multiple antibiotics including Meropenem, Acyclovir, Anidulafungin, and Levofloxacin.
Patient was evacuated to our center 3 weeks after his initial admission. He had a hoarse voice and could not tolerate oral feeding as food would leak from his left side of his neck with choaking episodes. Therefore, the admission diagnosis to our hospital was left pharyngo-cutaneous fistula following parapharyngeal and left peritonsillar abscess drainage and debridement. Clinical examination showed a left 3 × 2 cm peritonsillar wound with mild discharge. In the neck, he had a left sided 3 × 3 cm wound with mild discharge (Fig. 1). A probe was inserted from left neck wound and was almost reaching the left peritonsillar wound. A flexible fiber optic nasoendoscopy was done for the patient and showed a clear patent airway with left vocal cord immobility. Contrasted CT neck was done in our center and showed an almost complete resolution of the left parapharyngeal and peritonsillar abscess with expected postsurgical changes with a non-drainable subcutaneous fluid collection with peripherally enhancing walls located at the subcutaneous tissue of the left antero-lateral aspect of the neck tracking into the area of the thyroid, the collection measured 3.3 × 0.5 × 5.3 cm with evident fistula from the left peritonsillar area to antero-lateral aspect of the neck (Fig. 2).

Clinical exam showing a left sided 3 × 3 cm wound with mild discharge.
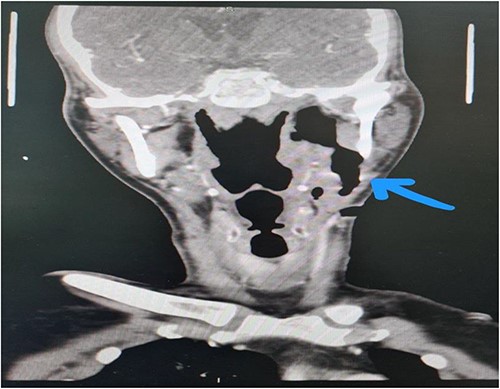
Contrasted neck CT showing fistula from the left peritonsillar area to antero-lateral aspect of the neck with a non-drainable subcutaneous fluid.
Patient was kept NPO with enteral feeding allowed only through nasogastric tube. A wound culture was taken. Neck wound was irrigated with half-strength povidone and packed with silvercel dressing (Systagenix) and covered with Paraffin gauze (Jelonet, Covidian) dressing twice daily for 2 weeks and then once daily for another 2 weeks. Patient was kept on insulin sliding scale to control his diabetes. Patient underwent upper GI series after 1 month which showed no fistula, yet positive for aspiration. The patient was discharged once the fistula was closed, on NGT feeding to optimize nutritional status and to do swallowing reassessment in 6 weeks with a referral to a laryngologist for his left vocal cord immobility (Fig. 3).

Discussion
Head and neck fistulas are a well-known complication that usually present after tumor resection. Very limited data are available on oropharyngocutaneous fistula in non-oncological patients. Pharyngo-cutaneous fistula is an uncommon complication following parapharyngeal space infection and peritonsillar abscess [3]. Orocutaneous fistula formation following deep neck space infections had a rate of 1.1% out of 277 cases in one Turkish study [4]. The identification of patients at high risk is crucial as it allows for the anticipation, prevention, and minimization of wound healing complications. Peritonsillar abscess incidence was higher in T2DM patients than in non-T2DM patients [3]. In this case, the patient’s neglected odontogenic infection, coupled with underlying diabetes, likely contributed to the development and persistence of deep neck infections.
Most small fistulae can heal on their own with local wound care, adequate nutrition, and blood volume maintenance. The closure of large fistulae requires the provision of sufficient epithelial lining to complete the pharyngeal wall and a cervical skin substitutes [5]. Parikh et al., Redaelli de Zinis et al., and Virtaniemi et al. have determined that 50%, 70%, and 80% of fistulas, respectively, will heal without the need for surgical intervention in patients postlaryngectomy [6–8].
Various wound dressings were described in literature, and no specific material nor a specific frequency of dressing change were prescribed. Silvercel was used in this patient to allow for both antimicrobial properties of the dressing and facilitation of epithelization process [9].
Our patient had an odontogenic infection that progressed into a parapharyngeal abscess and eventually developed pharyngo-cutaneous fistula following surgical management. Having Diabetes Mellitus, delayed presentation, and the fact that multiple incisions were done to drain the parapharyngeal, and later, the peritonsillar abscess could have contributed to fistula formation. Optimization of local and systemic factors affecting wound healing is paramount. Early NPO and NGT feeding contribute to early recovery of such patients while minimizing the risk of fatal complications.
Conflict of interest statement
In compliance with the ICMJE uniform disclosure form, all authors declare the following. All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.



