-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Sawafta, Ameer Awashra, Zaid Sawaftah, Ali Bani Odah, Amer Khatib, Huthayfa Dababat, Anas Yasin, Jehad Khamaysa, Muath Daraghmeh, A rare case of gastric schwannoma mimicking GIST: diagnostic and therapeutic approach, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae525, https://doi.org/10.1093/jscr/rjae525
Close - Share Icon Share
Abstract
Gastric schwannomas are rare, benign neurogenic tumors originating from Schwann cells within the gastrointestinal tract, comprising only 0.2% of all gastric tumors. This report presents the case of a 32-year-old female patient who experienced severe periumbilical pain, nausea, and vomiting, ultimately diagnosed with gastric schwannoma. Initial imaging and endoscopic evaluations suggested a gastrointestinal stromal tumor (GIST), but postoperative histopathological analysis confirmed schwannoma, showing S-100 positivity and negativity for CD117, DOG-1, SMA, Desmin, and CD34. The patient underwent successful central gastrectomy with negative surgical margins and no metastasis. Despite a postoperative complication of small bowel obstruction, which was managed conservatively, the patient remained symptom-free with no recurrence over the follow-up period. This case underscores the importance of differential diagnosis, distinguishing schwannomas from GISTs and other submucosal lesions through thorough histopathological and immunohistochemical analyses, and highlights the efficacy of complete surgical resection in preventing recurrence.
Introduction
Gastrointestinal mesenchymal stem cells give rise to spindle-shaped tumors known as gastrointestinal mesenchymal tumors. These tumors primarily include nerve sheath tumors (Schwannomas), smooth muscle tumors (leiomyomas or leiomyosarcomas), and gastrointestinal stromal tumors (GISTs). Among these, GISTs are the most common, with 60%–70% occurring in the stomach, while Schwannomas rarely arise in the gastrointestinal tract. gastric schwannoma (GS), a type of nerve sheath tumor that develops from Schwann cells of peripheral nerves, is typically benign, slow-growing, and asymptomatic. However, in some cases, it can cause bleeding, epigastric pain, and a palpable mass. Schwannomas can only be definitively diagnosed by postoperative immunohistochemistry staining, which typically shows S-100 positivity. Surgery is the primary treatment for GS, with total tumor removal potentially preventing recurrence [1, 2].
In this context, we present a case study of a 32-year-old female with no significant medical history, who presented with severe periumbilical pain, nausea, and vomiting. Imaging detected a gastric mass suspected to be a GIST. The patient underwent a successful central gastrectomy with negative surgical margins and no signs of metastasis. Histopathological examination revealed the mass to be a Schwannoma.
Case presentation
A 32-year-old female with no significant medical history presented to our emergency department with persistent periumbilical pain and fullness for 2 months, accompanied by episodes of nausea and vomiting. On physical examination, she was found to be conscious, oriented, and afebrile, with normal oxygen saturation and stable vital signs. Additionally, periumbilical tenderness was noted, but no palpable masses were detected.
Consequently, initial laboratory tests were conducted and returned normal results. However, an ultrasound revealed a 5 × 6 cm cystic lesion. Therefore, further investigation through an abdominal CT scan with oral and intravenous contrast was warranted, which identified an oval-shaped lesion in the gastric lesser curvature (see Fig. 1), raising suspicion for a GIST. To further evaluate, an upper endoscopy and endoscopic ultrasound-guided fine needle biopsy (EUS-FNB) were performed, revealing a gastric mass extending from the lesser curvature to the greater curvature anterior wall. As a result, a central gastrectomy with clear surgical margins was performed, yielding a well-defined, elastic mass measuring 6 × 6 cm. Notably, the resected specimen exhibited no necrosis, lymph node enlargement, or additional lesions. Additionally, a follow-up abdominal CT scan confirmed the absence of metastasis.
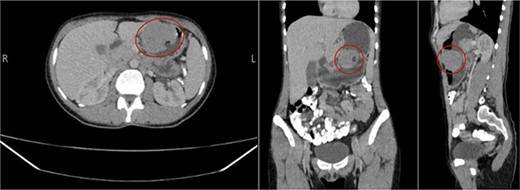
Well-defined enhancing oval-shaped gastric lesion seen in the gastric lesser curvature with intra and extra luminal components; it presents a small ulcer at the intraluminal component.
Subsequent histopathological examination of the resected specimen confirmed the diagnosis of GS. The tumor displayed a dense proliferation of spindle cells with numerous blood vessels. Immunohistochemical staining was positive for S100 and negative for CD117, DOG-1, SMA, Desmin, and CD34.
Postoperatively, the patient was initially transferred to the intensive care unit and then to the general ward, where she demonstrated clinical improvement and was subsequently discharged. However, 2 weeks postdischarge, the patient experienced a recurrence of symptoms, including nausea, vomiting, abdominal pain, acute back pain, and abdominal distention. Consequently, an abdominal and pelvic CT scan was performed, which revealed multiple air-fluid levels and small bowel dilation, indicative of small bowel obstruction.
The patient was urgently readmitted and treated with a pain management regimen that included morphine sulfate and scopolamine. Her response to the treatment was favorable, resulting in complete symptom resolution as confirmed by clinical evaluation and imaging studies. Follow-up plans included CT scans at 6 months and 1 year to monitor for recurrence or complications. Since then, the patient has remained asymptomatic, with no further complications or recurrence observed.
Discussion
Schwannomas, also known as neurilemmomas or neurinomas, are benign neurogenic tumors originating from Schwann cells, which form the myelin sheath around peripheral nerve axons. These tumors most commonly appear in the head and neck regions; however, they are rare in the gastrointestinal (GI) tract, where they arise from the nerve plexus within the gut wall. In the GI tract, the stomach is the most prevalent site for schwannomas, followed by the colon, whereas the small intestine and esophagus are less frequently affected. Specifically, schwannomas constitute 0.2% of all gastric tumors, 6.3% of gastric mesenchymal tumors, and 4% of all benign gastric tumors. To date, over 221 cases of GS have been reported globally. These tumors can occur at any age, with a slight female predominance [2, 3].
GS must be differentiated from several other gastric submucosal lesions. The primary differential diagnoses include GISTs, which are the most common mesenchymal tumors with a significant malignant potential, unlike the typically benign schwannomas. Leiomyomas and leiomyosarcomas are also important considerations, as they present similarly but require distinct histopathological analysis for differentiation. Neurofibromas, although also benign nerve sheath tumors, differ significantly in clinical and pathological features of Carcinoid tumors, another potential differential diagnosis, are neuroendocrine in nature and identified through specific histological staining. Additionally, peptic ulcer disease can mimic schwannomas when presenting with ulceration or bleeding. Accurate diagnosis of GS relies on thorough histopathological and immunohistochemical analyses to distinguish these conditions effectively [3–5].
The primary treatment for GS is complete surgical resection, typically via wedge resection or partial gastrectomy. Studies have shown that complete surgical excision with negative margins is curative, and long-term follow-up often reveals no recurrences or metastases. For instance, in a clinicopathologic study of 51 cases, patients were followed for a median duration of 4.7 years, during which no recurrences or metastases were reported [2].
Conclusion
We describe the rarity and clinical significance of GSs, benign tumors that can mimic other gastrointestinal submucosal lesions such as GISTs. The definitive diagnosis relies on histopathological and immunohistochemical analysis, which is crucial for appropriate treatment planning. Surgical resection remains the cornerstone of treatment, offering excellent prognostic outcomes with minimal risk of recurrence when negative margins are achieved. The postoperative complication of small bowel obstruction in this case was managed successfully, emphasizing the need for vigilant postoperative monitoring. Ultimately, this case emphasizes the importance of considering GSs in the differential diagnosis of gastric masses and demonstrates the efficacy of surgical intervention in ensuring favorable patient outcomes.
Acknowledgements
We express our deep gratitude to the medical ward staff for their invaluable support in completing this report.
Conflict of interest statement
The authors state that they have no conflict of interest to be mentioned.
Funding
No specific grant from funding agencies was received for this work.
Ethics approval
Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent
Written informed consent was obtained from the patient himself for his anonymized information to be published in this article.



