-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Hendrix, Ankur Makani, Thomas Crafton, Camille Graham, Carlos Torres-Medina, Michael Cicchillo, Open treatment of infected abdominal aortic aneurysm stemming from perineal infection, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae495, https://doi.org/10.1093/jscr/rjae495
Close - Share Icon Share
Abstract
Infected abdominal aortic aneurysms (AAAs) make up a small minority of AAAs yet are characterized by a high fatality rate, largely attributed to their increased risk of aneurysm rupture. This case details a rare presentation of a 56-year-old man that developed Proteus mirabilis bacteremia secondary to a perineal abscess and subsequently experienced a 3 cm growth of his previously stable AAA over an 8 day period. This case underscores the importance of maintaining a heightened suspicion for infected aortic aneurysms in sick patients and highlights the critical role of surgical management in achieving source control.
Introduction
Infected abdominal aortic aneurysms (IAAAs) represent roughly 1% of all AAAs. [1] These aneurysms are most commonly described as occurring in the lower abdominal aorta with roughly 50% below the level of the renal artery [2]. Risk factors include male sex, smoking, prior infections, weakened immune system, atherosclerosis, existing aneurysms, and aging (>65 years) [3]. Several retrospective studies have demonstrated an increased rate of rupture in infected aneurysms with latest estimates upwards of 50–85% [1]. This makes IAAA a dangerous diagnosis to miss. Unfortunately, patients with IAAA generally present with nonspecific symptoms with only 16% having the classic triad of fever, back pain, and pulsatile mass [4]. Thus, diagnosis is frequently delayed and made in late stages with the presentation of fulminant sepsis or aneurysm rupture [4].
The advent of antibiotics not only decreased the incidence of IAAAs, but also changed the most common offending microbial agents. Endocarditis caused by gram-positive cocci used to be the primary culprit behind IAAA occurrences, however, gram-negative organisms have surged in prevalence, now representing up to 40% of cases [5]. Among these, Staphylococcus and Salmonella spp emerge as the leading pathogens accounting for 21 and 16%, respectively [6]. While less frequent, Escherichia coli has also been linked to IAAAs [5]. The authors describe a rare case of a 56-year-old immunocompetent man with a known, asymptomatic 4.7 cm AAA that developed Proteus mirabilis bacteremia secondary to a perineal abscess and subsequently had a rapid growth of his AAA to 7.8 cm over the span of 8 days. The patient provided written informed consent for the report of his case details and imaging studies.
Case report
A 56-year-old male with no reported past medical history and a 70 pack year smoking history presented with a chief complaint of lower abdominal pain and body aches. On presentation, the patients white blood cell count (WBC) was 39.6 and procalcitonin was 43.4. Blood cultures were drawn and demonstrated P. mirabilis bacteremia. Computed tomography (CT) abdomen/pelvis was performed as well as ultrasound (US) of scrotum demonstrating a complex fluid collection within scrotal sac that was determined to be a scrotal wall abscess. The patient was started on a course of Unasyn and Urology promptly took him to the operating room (OR) for incision and drainage. Vascular surgery was consulted due to an incidental finding of an abdominal aortic aneurysm on CT measuring 4.7 × 4.6 cm (Figs 1 and 2). The patient was evaluated by the vascular surgery team following his urological procedure and denied any history of abdominal pain or back pain. Physical exam was largely unremarkable however the patient’s bilateral toes were noted to have blue discoloration with motor and sensation intact. Outpatient follow up with routine US scans for the AAA was recommended. Ankle brachial index (ABI) as well as an echocardiography was ordered to further work up the patient’s dusky toes. On Day 2 of hospitalization, ABIs returned showing severe peripheral vascular disease (PVD) and the echocardiography ruled out endocarditis. At this time an angiogram was planned to further the patient’s PVD workup however this was deferred as the patient remained septic with a WBC of 30. Over the course of the next few days the patient refused antibiotics and remained septic with a WBC in the 20s. At this time his toes quickly deteriorated from dusky to dry gangrene. On Day 8 of hospitalization the patient remained septic and was now complaining of new onset mid-abdominal pain. Emergent CT showed AAA was now 7.7 × 7.8 cm with periaortic fat stranding concerning for impending rupture (Figs 3 and 4). The patient was taken emergently to the OR for open repair. Upon visualization, the abdominal aortic aneurysm was clearly infected with signs of impending rupture on the left lateral wall and purulent material including infected thrombus. Tissue was cultured however showed no growth, likely due to the fact that the patient had been on antibiotic therapy for a week at this time. Reconstruction with an aorto-biiliac bypass using rifampin-soaked dacron graft was performed. A piece of omentum was mobilized over the graft and the retroperitoneum was closed over it. The abdomen was left open for a return to the OR for a second look which showed no concerns for bowel ischemia, worsening infection or bleeding. On post-op Day 5 the patient was extubated, off pressor support, and transferred to the floor. The patient’s postoperative course was unremarkable except for bilateral toes demarcating to dry gangrene.
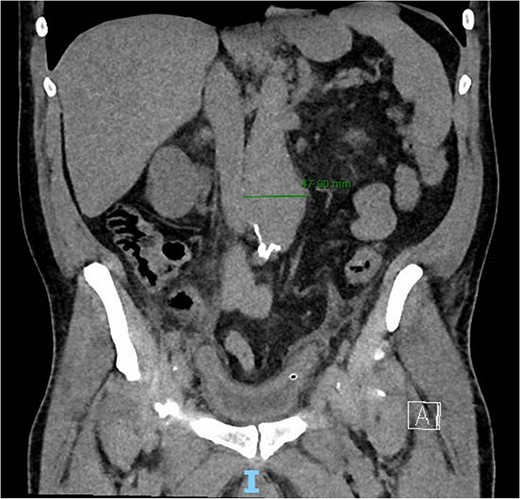
Frontal CT of the abdomen and pelvis demonstrating 4.79 cm AAA.
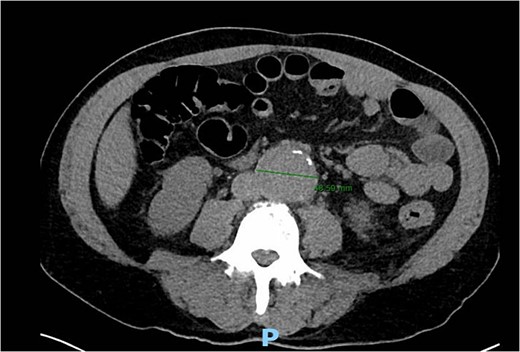

Frontal CT angiography of the abdomen and pelvis demonstrating 7.75 cm AAA with fat stranding.
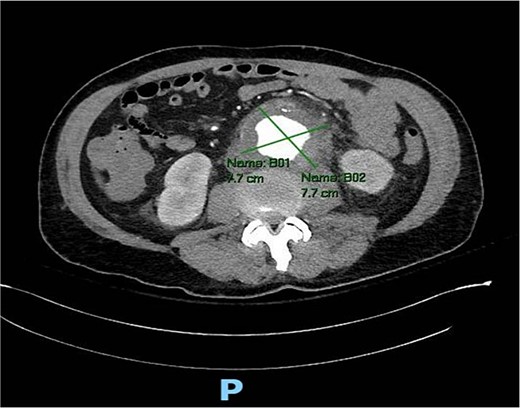
Axial CT angiography of the abdomen and pelvis demonstrating 7.7 cm AAA with fat stranding.
Discussion
This case is unique in its acute presentation and involvement of atypical bacteria. To the best of the authors’ knowledge, no report has yet to demonstrate an asymptomatic AAA undergo 3 cm of growth over the course of just 8 days in a hospitalized patient. The large majority of cases of IAAA are found on initial presentation. Additionally, only one other case has been reported demonstrating IAAA secondary to P. mirabilis bacteremia [7]. The large majority of cases reported in the literature involve Staphylococcus, Salmonella, and Escherichia spp with few reports of rarer bugs such as Treponema [8], Coxiella [9], and Yersinia [10].
Furthermore, this case highlights the importance of maintaining a heightened suspicion for IAAA in critically ill patients even if it is not present on initial presentation. Not only do symptomatic IAAAs have an increased risk of rupture, but a near 100% mortality rate upon rupture if prompt intervention with intensive resuscitation and surgery is not performed [11]. Several retrospective studies have found medical therapy alone resulted in rapid aortic dilatation leading to rupture and/or uncontrolled sepsis in the early period [12, 13]. In fact, medical therapy alone was found to be the highest risk factor for mortality due to rupture in the acute phase [12]. Thus, this case highlights the critical role of surgical management in achieving source control for these patients.
Conflict of interest statement
None declared.
Funding
None declared.



