-
PDF
- Split View
-
Views
-
Cite
Cite
Amanda Skogsberg, Allison Porter, Robotic-assisted repair of an anterior diaphragmatic hernia secondary to Xiphoidectomy, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae464, https://doi.org/10.1093/jscr/rjae464
Close - Share Icon Share
Abstract
Anterior diaphragmatic hernias manifest when a diaphragmatic defect permits abdominal contents to enter the thoracic cavity. They may be congenital or acquired; when acquired, the typical etiology is traumatic injury. Without treatment, they risk incarceration or strangulation. A 55-year-old male with a history of xiphoidectomy during sternotomy for cardiac disease was incidentally found to have an anterior diaphragmatic hernia on a screening chest CT (computed tomography) scan. He developed gastric obstruction shortly after an outpatient surgical consultation. He was admitted to the hospital, and further workup revealed a right-sided type-4 diaphragmatic hernia with an incarcerated colon, antrum, and pylorus. Nasogastric decompression was performed, followed by robotic-assisted transabdominal preperitoneal (r-TAPP) repair with mesh. He recovered without complications. There are currently no reports in the literature of an anterior diaphragmatic hernia secondary to a xiphoidectomy. This case demonstrates the successful use of r-TAPP for this rare presentation of an anterior diaphragmatic hernia.
Introduction
Anterior diaphragmatic hernias occur when a defect in the diaphragm permits abdominal contents to breach into the thoracic cavity. These hernias may arise congenitally or be acquired, often secondary to trauma. Symptoms commonly associated with diaphragmatic hernias encompass respiratory distress, along with gastrointestinal or cardiac manifestations. Prompt surgical intervention is the recommended treatment modality, as untreated defects pose risks of bowel obstruction and incarceration [1]. Currently, the laparoscopic approach is the most utilized, with few cases in the literature using a robotic approach. Here, we present a case of robotic-assisted repair of a symptomatic anterior diaphragmatic hernia ten years after xiphoidectomy.
Case presentation
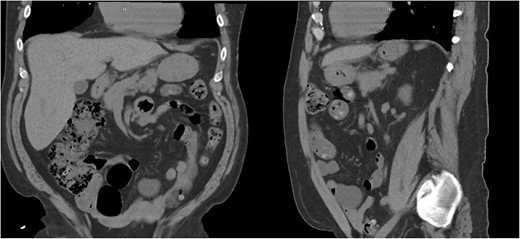
A 55-year-old male underwent lung cancer screening with a chest CT scan (Fig. 1) and was incidentally found to have an anterior diaphragmatic hernia just inferior to the sternum.
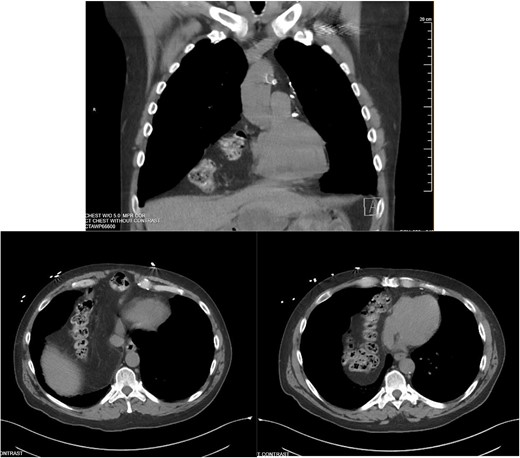
Approximately ten years prior, he had undergone coronary artery bypass surgery (CABG) with a xiphoidectomy. His symptoms at the time of the CT were right upper quadrant pain and epigastric fullness. He was referred for outpatient surgical evaluation. Shortly after the initial surgical assessment, he presented to the emergency department with gastric outlet obstruction. An abdominal CT was performed, showing a right-sided type 4 anterior diaphragmatic hernia with herniation of the antrum and pylorus causing the obstruction (Fig. 2). A loop of the transverse colon was also herniated into the thorax but without colonic obstruction.
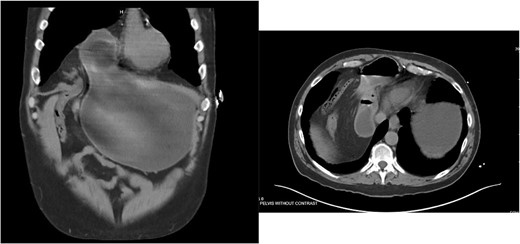
Right-sided type 4 anterior diaphragmatic hernia with antrum and pylorus herniation.
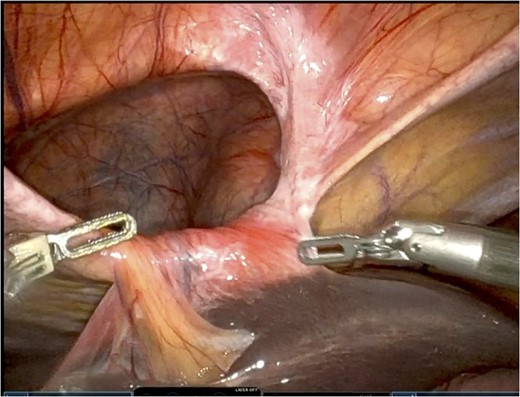
He was admitted for nasogastric decompression and underwent an upper endoscopy with benign findings. Once stable, he was discharged and optimized as an outpatient by adhering to a high-protein liquid diet. He underwent a scheduled robotic-assisted transabdominal preperitoneal (r-TAPP) repair of a type 4 anterior diaphragmatic hernia with mesh. The robot was docked and targeted with four 8 mm robotic ports across the mid-abdomen. A moderately sized hernia containing a loop of the transverse colon was identified. This was gently reduced (Fig. 3).
The falciform ligament was taken down with bipolar cautery. A peritoneal flap was created commencing about 4 cm inferior to the defect. A preperitoneal dissection was then performed to create the flap and to reduce the sac out of the mediastinum (Fig. 4).
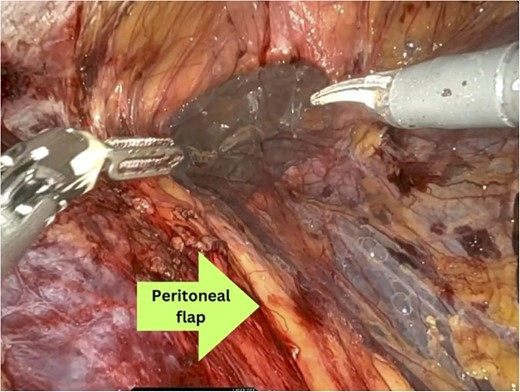
Care was taken to avoid injury to the pleura and the pericardium. Once the sac was reduced, the defect’s size was measured as 9 cm in horizontal length by 4 cm in vertical dimension. Primary closure of the defect was performed with a running 0 V-loc absorbable 180 suture.
Polypropylene ProGrip mesh was then cut to size to cover the primary defect. It was cut to 14 cm in horizontal dimension by 7 cm in vertical dimension, with rounded edges (Fig. 5).
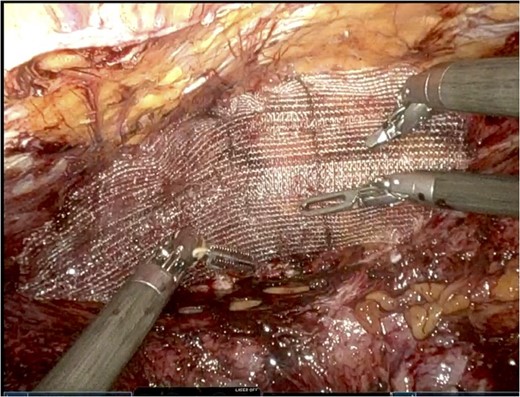
Once it was in an appropriate position to cover the defect, attention was turned to the peritoneal flap closure with a running 3–0 V-Loc suture.
His recovery course was without complication, and he was discharged post-operative day one. At three-month follow-up, he was asymptomatic. He could take deep breaths again, eat solid foods, and subsequently gained twenty pounds.
He underwent a CT scan ten months after surgery for flank pain with suspected nephrolithiasis, which demonstrated the successful repair (Fig. 6).
Discussion
Diaphragmatic hernias are predominately congenital but, in rare instances, can be acquired. Among congenital variants, Morgagni hernias manifest anteriorly, while Bochdalek hernias occur in a posterolateral position [1]. Hiatal hernias, including those at the esophageal hiatus and paraoesophageal hernias, may arise from traumatic events, be acquired, or occur spontaneously, further diversifying the etiology of diaphragmatic hernias. Increased abdominal pressure can precipitate herniation, leading to symptoms and complications [3, 5].
Anterior diaphragmatic hernias predominantly arise on the right side, attributed to the protective and supportive pericardial attachments to the diaphragm on the left side [1, 3].
The clinical presentation of diaphragmatic hernias varies, often masquerading as respiratory or cardiovascular ailments. Our patient initially experienced mild, nonspecific symptoms, which rapidly progressed to gastric outlet obstruction, highlighting the variable nature of symptomatology associated with these hernias.
Repair can be performed via an abdominal approach or transthoracic approach with no distinct evidence on which is superior. If there is strangulation, intra-abdominal adhesions, or bilateral diaphragmatic hernias, then an abdominal approach may be preferred for ease of access [3]. A study concluded that a thoracic approach may be better on a right-sided hernia due to better views and access to pericardial and pleural adhesions [3].
Small defects may be suitable for primary closure, while larger defects often necessitate reinforcement, such as the application of mesh, as in our patient [2]. If the defect is too large for primary closure, mesh can be used as a bridge. Creating the peritoneal flap and preperitoneal dissection allows for a pocket for mesh placement where the mesh will have no contact with abdominal viscera.
Laparoscopic repair is the most common method for addressing this defect, with the literature showing few cases of robotic-assisted approaches [4–6].
To our knowledge, this is the first case of an anterior diaphragmatic hernia secondary to xiphoidectomy. Limited literature exists on the robotic-assisted transabdominal preperitoneal (r-TAPP) approach for the primary repair of symptomatic diaphragmatic hernias. In our case, we employed this method to successfully address a rare case of symptomatic gastric outlet obstruction resulting from an incarcerated anterior diaphragmatic hernia secondary to a xiphoidectomy in an adult male. Our report contributes to the evolving understanding and management of diaphragmatic hernias, emphasizing the importance of tailored surgical approaches for optimal patient outcomes.
Conflict of interest statement
Dr. Allison Porter serves as a proctor for Intuitive Surgical Inc. The authors declare that there are no other conflicts of interest regarding the publication of this case report.
Funding
None declared.



