-
PDF
- Split View
-
Views
-
Cite
Cite
Muhammad Ismail, Myat Soe Thet, Kalim Ullah Khan, Nusrat Ullah, Dorsal ectopic breast—a cutaneous marker of occult spinal dysraphism, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae441, https://doi.org/10.1093/jscr/rjae441
Close - Share Icon Share
Abstract
Ectopic breasts represent uncommon medical anomalies characterized by the presence of additional breasts situated outside the typical milk line. In this case report, we present a case encompassing dorsal ectopic breasts accompanied by three nipples. A 14-year-old teen girl presented with a significant dorsal mass, exhibiting no clinical manifestations except mild pain and a sense of heaviness. She underwent investigations, and a magnetic resonance imaging scan revealed a large, inadequately encapsulated congenital mass with a fatty composition, alongside intraspinal epidural engagement and a bony structure bridging the spinous processes from the C6 to the T3 vertebral bodies. She subsequently underwent excision of the entire mass. The histopathological analysis identified the presence of a mammary hamartoma. Follow-up at 2 weeks postoperatively showed that there were no further complications. Dorsal ectopic breast necessitates careful and comprehensive evaluation to either confirm or exclude the presence of occult spinal dysraphism prior to intervention to avoid complications.
Introduction
Ectopic breast refers to a medical scenario characterized by the presence of an additional breast, while ectopic nipple denotes a clinical condition characterized by an extra nipple [1]. Commonly, these anomalies can be observed along the milk line extending from the axilla to the groin. Yet, they may manifest anywhere on the body, including the scapula [2], dorsum [1, 3], and thigh [4] among other areas. We present a case involving an ectopic breast located on the dorsal spine. There is a suggestion in the literature of a potential underlying occult spinal dysraphism (OSD) with the dorsal ectopic breasts [1, 3]; however, our case exhibited merely a rudimentary spinous process. OSD is an imperceptible clinical condition where the abnormal fusion of the posterior vertebral arch occurs with unexposed neural tissues and intact overlying skin [5]; however, it may manifest cutaneous stigmata [6] and clinical features [7], which clue toward underlying spinal lesion.
Case report
A 14-year-old teen girl was presented at the outpatient clinic, accompanied by a complaint of a progressively enlarging mass on the upper dorsal region, observed since early childhood. The increase in size was significantly noted over the last 3 years (Fig. 1). Concurrently, she experienced discomfort and a sensation of heaviness in the upper back. She also reported an inability to gain weight, hair loss, and facial acne. Physical examination revealed a soft tissue mass reminiscent of breast tissue, measuring ~9.5 cm cranio-caudally, 5 cm anteroposteriorly, and 11 cm in the transverse dimension, situated in the inferior segment of the neck region. Additionally, three nipples were identified: one centrally located at the upper end and two bilaterally positioned at the lower end. Among these, the nipple situated on the right lower end exhibited anatomical resemblance to a typical nipple, while the others did not. The mass demonstrated no lateral mobility, and neurological examination showed normal findings in both upper and lower extremities.
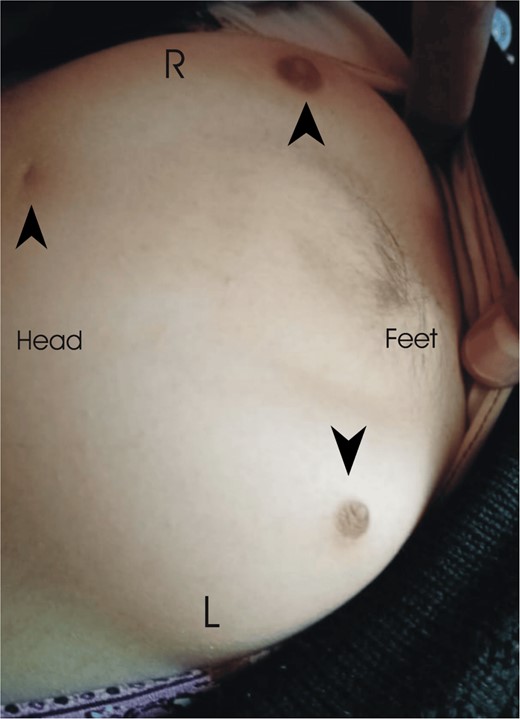
This is the dorsal spine of the patient showing bilateral ectopic breasts (R = right, L = left) and three ectopic nipples (black arrowheads).
A magnetic resonance imaging (MRI) scan of the neck, conducted with and without contrast following standard protocols, displayed a large, poorly encapsulated fat signal mass in the inferior neck and superior dorsal region, with intraspinal epidural extension at the C6-C7 vertebral level, protruding into the spinal canal and positioned posteriorly opposite to the C6 and C7 vertebral bodies, inducing moderate spinal compression of the cervical cord displacing anteriorly. A bony structure was observed connecting the spinous process at the C6 vertebral body to the T3 vertebral body. The prominent characteristics are indicative of a congenital fat-containing mass with intraspinal epidural involvement. The differential diagnosis encompasses, but is not restricted to, spinal dysraphism associated with lipoma, teratoma, or a dermoid mass (Fig. 2).
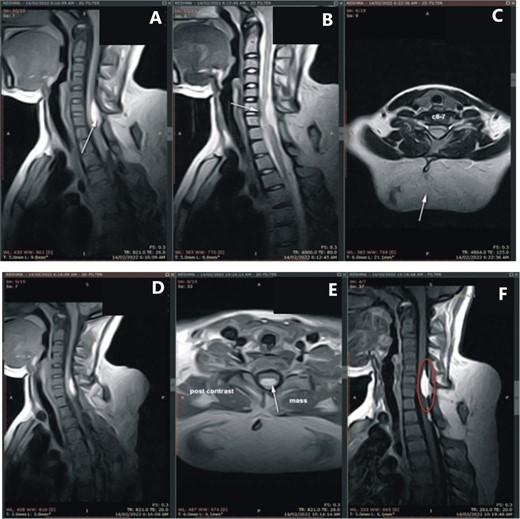
(A) MRI of the cervical and dorsal spine; (C) a large, poorly encapsulated fat signal mass in the inferior neck and superior dorsal region (white arrow), and (B, D) an intraspinal epidural extension at the C6-C7 vertebral level, protruding into the spinal canal and positioned posteriorly opposite to the C6 and C7 vertebral bodies (white arrows), and (A, F) a bony structure connecting the spinous process at the C6 vertebral body to the T3 vertebral body (white arrow and red circle).
Subsequently, the patient underwent surgery with the entire tissue mass, together with the rudimentary spinous process, was excised, and sent for histopathological examination. The spinal canal was not explored. The patient was sent home on the following day. Histopathology findings demonstrated breast ducts with a few intact lobules. Histological features showed mammary hamartoma; considering the clinically described site, this may represent a hamartoma in accessory breast tissue. Postoperative follow-up at 2 weeks revealed a fully healed, clean, and dry wound with no observed complications. Fortunately, the patient had no motor or sensory deficits in the upper and lower limbs. Subsequent multiple follow-up appointments reported the patient’s weight gain, cessation of hair loss, and absence of acne.
Discussion
In our case, the presence of ectopic breasts over the dorsal spine was observed, with clinical manifestations limited to pain and heaviness. A successful resection was performed, and subsequent histopathological analysis confirmed a diagnosis of mammary hamartoma. This case merits presentation due to its distinctive nature; within the existing literature, only two analogous cases have been identified, both exhibiting OSD [1, 3]. Contrarily, our examination only revealed a bony structure bridging the spinous processes of the C6 and T3 vertebrae, which were entirely excised during the intervention.
The human breast develops from a primary mammary bud, which is paired with solid epithelial masses in the pectoral region at the fourth intercostal spaces, a remnant of mammary crest or ridge [8]. Accessory breasts and nipples have been seen in the milk line which signifies the existence of the mammary crest [9]. However, numerous studies have explored the genesis of ectopic breast tissue in the body away from the milk line, positing theories including sweat gland metaplasia and aberrant migration of primordial breast cells away from the milk line [10], among others.
A notable enlargement of the ectopic breast tissue was documented during the patient’s puberty, a phenomenon corroborated by existing literature attributing such growth to hormonal fluctuations [11]. Behaving like a normal breast, ectopic breasts are prone to the risks of development of infection, and benign or malignant conditions [12].
Spinal dysraphism is an umbrella term for a group of disorders arising from cutaneous, mesodermal, or neural derivatives of the dorsal median region of the embryo [13]. OSD is an imperceptible clinical condition where the abnormal fusion of the posterior vertebral arch occurs with unexposed neural tissues and intact overlying skin [5]; however, it may manifest cutaneous stigmata [6] and clinical features [7] which clue toward underlying spinal lesion. OSD can occur with or without cutaneous and subcutaneous mass, which could be lipomeningocele, meningocele, dermal sinus, ectopic breast, etc. [7]. However, the literature fails to demonstrate a direct association between ectopic breast and OSD. Further research would be paramount in this regard.
Ectopic breasts can be managed either conservatively or surgically depending upon growth, clinical features, and cosmesis [14]. There could be no symptoms at all or patients may present with pain, heaviness, significant growth during puberty, discomfort during menstruation, and cosmesis, which prompts surgical removal in experienced hands [15]. We went for complete surgical removal because there was significant growth, mild pain, heaviness, and cosmetic issues. Literature is lacking in the natural history of the ectopic breast; however, behaving like a normal breast, it would grow like a normal breast and should be kept under observation for any unusual growth, development of infections, and benign or malignant conditions.
Conflict of interest statement
None declared.
Funding
None declared.



