-
PDF
- Split View
-
Views
-
Cite
Cite
Mansour M Aldhilan, Abdullah H Alshahrani, Ismail H Almogbil, Heterotopic ossification postsuperficial medial collateral ligament pie-crusting: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae305, https://doi.org/10.1093/jscr/rjae305
Close - Share Icon Share
Abstract
Anterior cruciate ligament and meniscus tears are common among sports injuries. There are different techniques for addressing anterior cruciate ligament and meniscus tears, with distinct indications, advantages, and disadvantages. We present the case of a 23-year-old male who underwent right anterior cruciate ligament reconstruction and posterior horn medial meniscus repair using an all-inside technique via superficial medial collateral ligament (sMCL) pie-crusting. Clinical examination and radiological investigations a few months later identified calcifications on the medial side of the right knee. We diagnosed the patient with heterotopic ossification post-sMCL pie-crusting; no apparent causal factors were present. To our knowledge, there have been no documented instances of heterotopic ossification following sMCL pie-crusting. In conclusion, heterotopic ossification may occur after sMCL pie-crusting; further studies are needed on this subject.
Introduction
The anterior cruciate ligament (ACL) is a significant component of the knee joint [1]. It consists of two major bundles: anteromedial and posterolateral [2]. It is the major hindrance to anterior tibial translation, with some contribution to rotational stability [3]. ACL tears are the most common ruptured ligaments in the knee among sports-related injuries, with an annual rate exceeding 80 000 cases in the United States [4]. Acute ACL tears are often accompanied by injuries, including the medial and lateral meniscus tears, as well as posterolateral corner injuries. Chronic ACL tears may lead to a higher incidence of medial meniscus tears, possibly due to chronic instability [5]. Different techniques have been employed for ACL reconstruction using diverse graft options, such as patellar tendon, hamstring tendons, autografts, and allografts, each with their own advantages and disadvantages [6]. Meniscus tears are common knee sports injuries requiring surgery due to mechanical symptoms or pain. Multiple surgical procedures for meniscus tears have been described in the literature, including open surgical repair, arthroscopic-assisted inside-out, outside-in, and all-inside procedures [7]. Combining meniscus repair with ACL reconstruction is crucial, as it enhances stability and increases the success rate of meniscus healing by up to 92% [8]. Superficial MCL (sMCL) pie-crusting is commonly used in posterior horn medial meniscus (PHMM) repair to widen joint space, allow complete access to the posterior-medial knee compartment, and reduce the risk of iatrogenic cartilage injuries. Theoretically, sMCL pie-crusting may cause residual knee instability, pain, or saphenous neurovascular injury. Nevertheless, most clinical studies did not report such complications [9]. Heterotopic ossification (HO) is defined as the formation of bone within extra-skeletal structures [10]. As far as we know, no cases have been reported in the literature about HO post-sMCL pie-crusting. This case report has been reported in accordance with the Surgical Case Report guidelines [11].
Case report
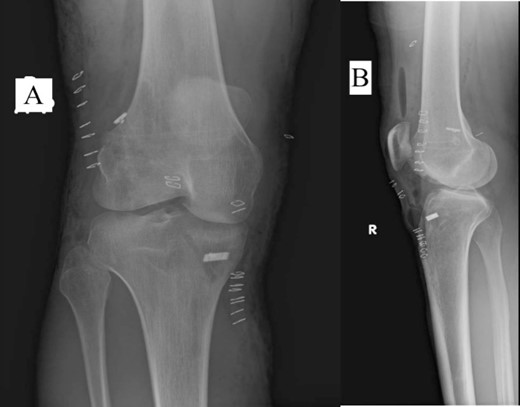
A 23-year-old male veterinarian presented to our out-patient department postright ACL reconstruction with hamstring autograft, PHMM tear by all-inside repair via sMCL pie-crusting technique, and lateral extra-articular tenodesis (modified Lemaire) in June 2023. A preoperative plain radiograph of the right knee revealed no evidence of HO (Fig. 1). No evidence of heterotopic ossification was detected in the right knee on plain radiographs taken 2 weeks postsurgery. (Fig. 2). Five months postsurgery, plain radiographs revealed new bone formation at the medial femoral condyle, precisely where the sMCL femoral origin was located (Fig. 3). The patient was asymptomatic and continued with rehabilitation. Seven months after the surgery, the patient started to complain of pain and clicking sensations when the right knee was flexed beyond an angle of 130°. Magnetic resonance imaging revealed consolidation of the newly formed bone, leading to a diagnosis of HO post-sMCL pie-crusting (Fig. 4). Nine months following surgery, the patient began to feel a bony mass on the medial side of the right knee. A plain radiograph and computed tomography (CT) scan revealed the complete formation of a bone island (Fig. 5). The past surgical history of this patient revealed that he had undergone left knee ACL reconstruction with hamstring autograft in December 2021, which failed and was complicated by a PHMM tear. The patient had presented to our facility for a revision. A revision ACL reconstruction was done using a bone-tendon-bone (BTB) autograft and PHMM tear all-inside repair via the sMCL pie-crusting technique in February 2022. A 2-year follow-up of the left knee, including physical examination and 3D-CT scans (Fig. 6), revealed no symptoms or signs of HO, although the same technique of sMCL pie-crusting was employed. Our patient suffered no head trauma during treatment. Past medical, drug, allergy, family, social histories, and reviews of systems were irrelevant to our case.
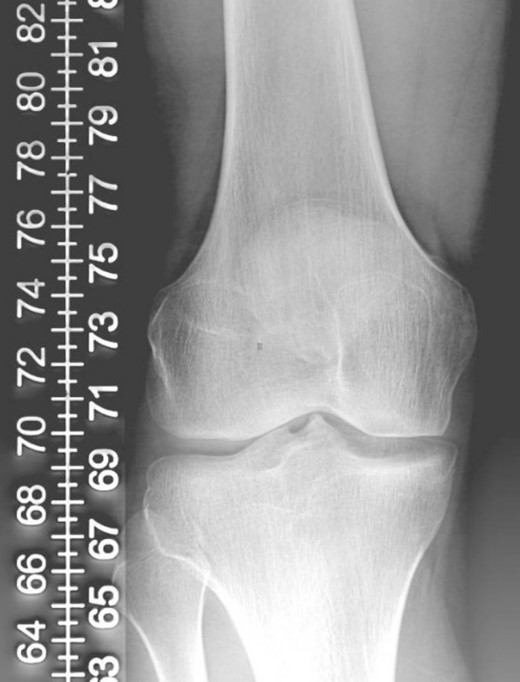
Plain radiograph of right knee AP (A) and lateral (B) 2 weeks postoperative showing no HO.

Plain radiograph of right knee AP (A) and lateral (B) 5 months postoperative showing initial HO.
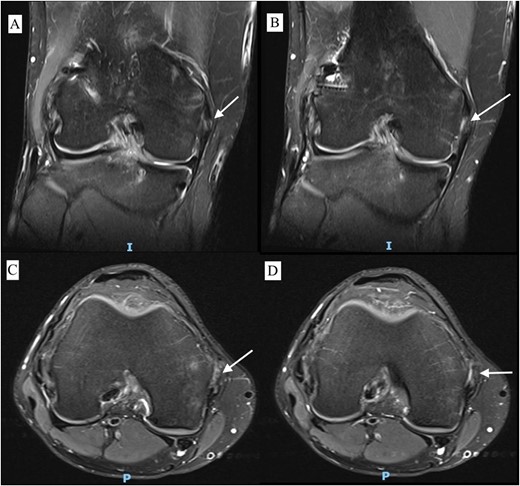
MRI T2 weighted image of right knee with different sections of coronal view (A, B) and axial view (C, D) 7 months postoperative showing HO.
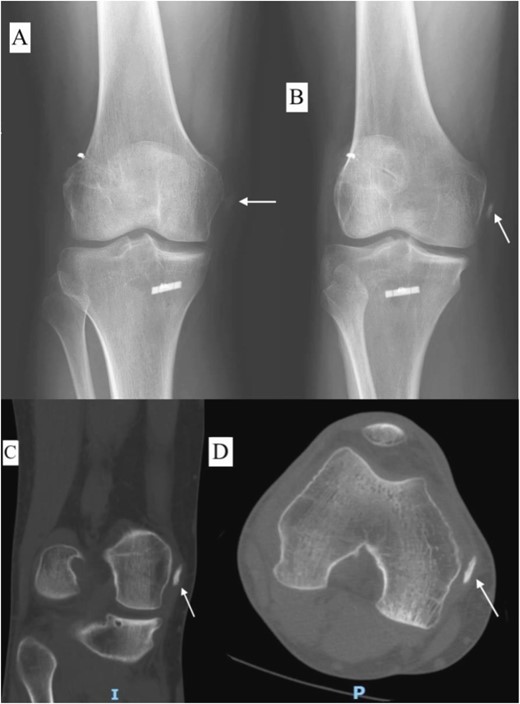
Plain radiograph of right knee AP (A), internal rotation AP (B), CT scan coronal view (C), and axial view (D) 9 months postoperative showing fully mature HO.

Discussion
To our knowledge, this is the first case to report the occurrence of HO post-sMCL pie-crusting. HO is a new bone formation within the soft tissue and has been documented in the literature as a rare complication of ACL reconstruction using a BTB autograft [12]. HO is known as a complication of different conditions, including central nervous system damage or trauma, musculoskeletal trauma, burns, and certain genetic diseases [13]. Our patient lacked identifiable causative factors for HO, and it is unclear why he developed it in the right knee, while there was no HO in the left knee, although the same technique of sMCL pie-crusting was used. During arthroscopic PHMM tear repair, sMCL pie-crusting is commonly used to widen joint space, facilitate the repair, and avoid chondral injuries [14, 15]. In our technique of sMCL pie-crusting, we initially mark the medial epicondyle, and an 18-gauge needle is used to puncture the skin 1.5-cm posterior and slightly distal to this point. The needle is repetitively inserted and withdrawn from the anterior to posterior aspect of the sMCL while applying gentle valgus stress and flexing the knee 20°–30°. An arthroscopic camera was used in the medial compartment to confirm the appropriate opening of joint space.
There are some limitations in our study. As it involves a single case without a known reason, we cannot attribute the cause of HO to pie-crusting. Although we used radiological investigations and clinical examinations, neither histological nor laboratory investigations were used for the diagnosis of HO. We recommend further consideration of this complication, including its implications, outcomes, causes, and preventive measures. Further level 1 and 2 studies are needed on such a topic. In conclusion, sMCL pie-crusting is a very helpful technique in medial meniscus repairs; however, it is accompanied by some risks. HO may occur after sMCL pie-crusting, and more studies are warranted on this topic.
Conflict of interest statement
None declared.
Funding
None declared.
Consent
Written and verbal consent were obtained from the patient for publication of this case, clinical findings, and related images. Written consent is available to the Editor-In-Chief upon request.



