-
PDF
- Split View
-
Views
-
Cite
Cite
Rebecca Jess, Virginia Summerour, Andrew Garnham, Michael Lewis Wall, Nina Al-Saadi, Kiran Randhawa, Successful treatment of a large profunda femoris artery aneurysm and associated pseudoaneurysm using endovascular stenting, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae221, https://doi.org/10.1093/jscr/rjae221
Close - Share Icon Share
Abstract
Profunda femoris artery aneurysms are a rare form of peripheral arterial aneurysm. In this report, we present the case of an 83-year-old lady who was found to have a 65 mm aneurysm arising from the proximal left profunda femoris artery and associated pseudoaneurysm. Successful treatment was achieved using an endovascular approach in which two stents were deployed.
Introduction
Profunda femoris artery aneurysms (PFAAs) account for 0.5% of all peripheral aneurysms [1, 2]. These aneurysms are thought to be rare due to the deep anatomical location of the artery, allowing for protection by the muscular tunnel of the adductor magnus [2–4]. Most reported PFAAs have been due to atherosclerotic wall degeneration amongst the elderly population; they have also been associated with connective tissue disease and multiple synchronous or asynchronous aneurysms [5, 6]. These aneurysms are often asymptomatic, however may present with a pulsatile groin swelling or symptoms of aneurysmal rupture [4]. PFAAs may also cause symptoms of local venous and nerve compression, leading to distal venous congestion and thigh pain [5]. We present a case report of a true PFA aneurysm and associated pseudoaneurysm and an endovascular approach for treatment.
Case report
An 83-year-old lady with a background of hypertension, peripheral vascular disease, previous stroke, gastro-oesophageal reflux disease, and poor mobility was referred by her General Practitioner to the Vascular clinic with a 1-month history of left groin swelling. She was previously known to the Vascular team due to bilateral superficial femoral (SFA) and popliteal artery aneurysms, as well as a left profunda femoris artery (PFA) aneurysm, however treatment had not been offered due to frailty and therefore surveillance was not arranged. Examination found a pulsatile, non-tender 50 mm × 50 mm left groin swelling.
CT angiogram of the lower limbs showed her previously known aneurysms, as well as a 65 mm aneurysm arising from the proximal left PFA (Fig. 1), with an associated 36 mm pseudoaneurysm likely representing a contained rupture.
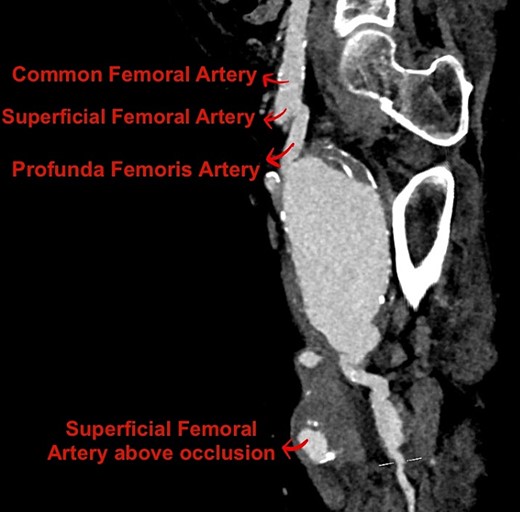
Reconstructed sagittal view of the CT angiogram lower limb showing the PFAA.
Due to the patient’s comorbidities, poor mobility, and a score of 6 on the Rockwood Frailty Scale, a decision to exclusively treat the PFAA endovascularly was taken, as the distal SFA was occluded [7].
Conventional angiogram of the left PFA was performed under local anaesthetic. Ultrasound guided puncture of the left common femoral artery was performed and two 10 mm × 150 mm Viabahn stents were placed via an 8 French sheath. Aneurysm exclusion was achieved as seen in Fig. 2 and flow is seen in the distal PFA. Stent patency was further confirmed post procedure using an Ultrasound Doppler.
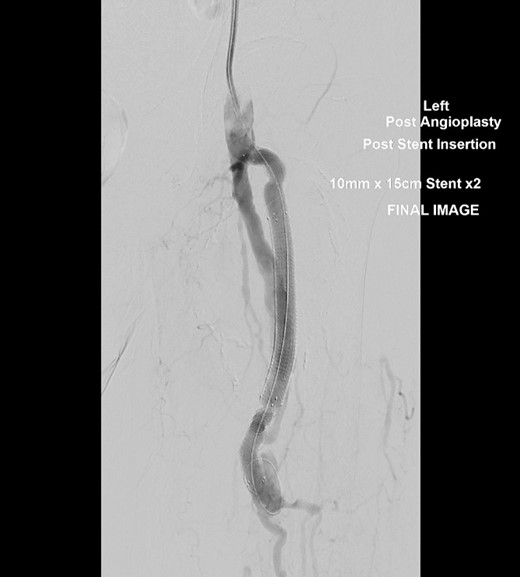
Conventional angiogram of the left PFA showing exclusion of the aneurysm and flow into the distal PFA after deployment of a second 10 mm × 150 mm Viabahn stent.
The patient recovered well and was discharged home with no changes to her medications (including 75 mg Aspirin OD and 10 mg Amlodipine OD). Due to her age, history of reflux, as well as her poor mobility and risk of falls, a single antiplatelet agent was preferred. She has attended for 6-monthly Ultrasound duplex follow-up scans to assess stent patency and monitor the other aneurysms. At 6 months, duplex showed that the left PFA stent is widely patent, and the residual aneurysm sac size is stable, with no endoleak or flow into the pseudoaneurysm.
Discussion
True PFAAs are thought to be rare due to their deep anatomical location allowing for protection [2–4]. However, this patient had risk factors including multiple aneurysms and hypertension that likely played a role in the development of her large PFAA. These aneurysms generally go undetected until they become symptomatic or rupture, but as PFAAs have a high rupture rate of 20%, they require surveillance, or intervention depending on size [5, 8]. The risk of rupture for asymptomatic aneurysms <20 mm is low, however they should be monitored annually via ultrasound duplex [1, 5]. For those that require intervention, several techniques have previously been described, with open surgery remaining the most common procedure [8]. Open surgical repair techniques have included ligation or resection with vascular reconstruction, whereas endovascular techniques have included covered stent graft implantation and coil embolization [8, 9].
For this patient, open surgical approaches were considered including bypass and ligation of the vessel, however this would have required extensive dissection to achieve distal control. Given the size of the PFAA, as well as the patient’s functional status, an endovascular approach under local anaesthetic was preferred. Two stents were deployed during the procedure, which excluded the aneurysm and sealed the pseudoaneurysm. The most recent scan shows patency of the stent, however, there are limited data on the long-term stent patency [9].
Conflict of interest statement
None declared.
Funding
None declared.



