-
PDF
- Split View
-
Views
-
Cite
Cite
Shota Morimoto, Futoshi Morio, Toshiya Tachibana, Tomoya Iseki, Lateral process fracture of the talus in a basketball player treated with arthroscopic reduction-internal fixation: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae220, https://doi.org/10.1093/jscr/rjae220
Close - Share Icon Share
Abstract
An open reduction-internal fixation is generally recommended in Type I lateral process fractures of the talus when the dislocation of the fragment is >2 mm. This report describes a case of a lateral process fracture of the talus in a 24-year-old male basketball player who underwent arthroscopic reduction-internal fixation. The patient complained of pain on the lateral aspect of his left ankle during a cutting motion. Based on physical examination and radiological findings, the patient was diagnosed with a lateral process fracture of the talus and underwent surgical treatment with arthroscopic reduction-internal fixation. At 12 weeks after the surgery, bone union was achieved, and the patient was able to resume playing basketball at his pre-injury level without symptoms, complications, or functional impairment. Lateral process fracture of the talus in a 24-year-old male basketball player was successfully treated with arthroscopic reduction-internal fixation.
Introduction
Lateral process fractures of the talus (LPFT) are relatively rare, accounting for 26% of all talar fractures and 0.4-1% of ankle injuries [1–4]. The fracture also commonly occurs in snowboarders and is known as ‘snowboarder’s fracture’ [5, 6]. LPFTs are generally divided into three types according to the Hawkins’ classification [1], which is useful for selecting of the appropriate form of management [7]. Type I is a simple fracture that extends from the talofibular articular surface down to the posterior talocalcaneal articular surface of the subtalar joint. Type II is the comminuted fracture that involving both the fibular and the posterior calcaneal articular surfaces of the talus and the entire lateral process. Type III is a chip fracture of the anterior and inferior portions of the posterior articular process of the talus. Particularly, in Type I cases with >2 mm of displaced bone fragment, an open reduction-internal fixation is generally recommended [7].
Here, we describe a case of Type I LPFT in a 24-year-old male basketball player who was successfully treated by minimally invasive, arthroscopic reduction-internal fixation.
Case report
A 24-year-old male basketball player presented to our hospital complaining of left lateral ankle pain during a cutting motion. His height, weight, and body mass index were 172 cm, 64.0 kg, and 21.6 kg/m2, respectively, and he had no history of previous medical conditions. On his first visit to our hospital, he could not walk due to pain. Physical examination revealed swelling, ecchymosis, and tenderness at the lateral aspect of his left ankle. The American Orthopedic Foot and Ankle Society (AOFAS) score was 32 out of 100 points. Plain radiographs of the left ankle showed no abnormal findings in the anteroposterior view, but a fracture line was discovered at the base of the lateral process of the talus in the lateral view (Fig. 1). Non-contrast computed tomography (CT) showed a simple fracture line that extending from the talofibular articular surface down to the posterior talocalcaneal articular surface of the subtalar joint. In addition, the bone fragment was displaced >2 mm (Fig. 2). The patient was diagnosed with Type I LPFT and underwent surgical treatment.

Plain radiographs of the left ankle showed no abnormal findings in the anteroposterior (A) view, but a fracture line was discovered at the base of the lateral process of the talus in the lateral (B) view.
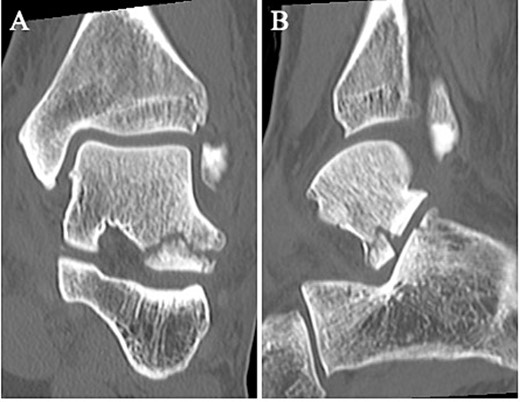
Non-contrast CT showed a simple fracture line that extending from the talofibular articular surface down to the posterior talocalcaneal articular surface of the subtalar joint in the coronal (A) and sagittal (B) views.
The surgery was performed under general anesthesia in the lateral position, with the affected side up. A thigh air tourniquet and a fluoroscopy were used. First, 3 ml of normal saline was injected into the sinus tarsi. A viewing portal was then made above the sinus tarsi, and a working portal was made 2 cm anterior to the viewing portal. A 30° arthroscope with a diameter of 2.7 mm was used to observe the fracture site (Fig. 3A). The synovium, adipose tissue and coagulation clot surrounding the fracture site were removed with a 3.0-mm-diameter motorized shaver, and the bone fragment was reduced using a guidewire sleeve and fixed with a 0.8-mm guidewire (Fig. 3B), the fragment was fixed through the guidewire with a cannulated double-threaded screw (Double Thread Screw Japan Mini, Meira, Nagoya, Japan) (Fig. 3C). After confirming that the bone fragment was fixed in the correct position under a fluoroscopy, the wound was sutured, and so the surgery was concluded (Fig. 4).
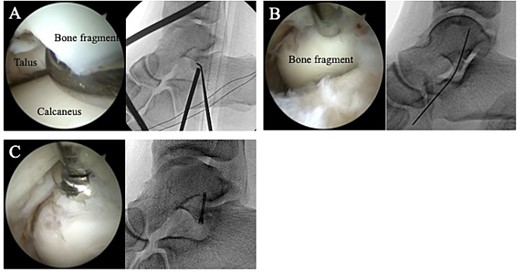
(A) A 30° arthroscope with a diameter of 2.7 mm was used to observe the fracture site. (B) The bone fragment was reduced using a guidewire sleeve and fixed with a 0.8-mm guidewire. (C) The fragment was fixed through the guidewire with a cannulated double-threaded screw.

Postoperative plain radiographs showed that the bone fragment was fixed in the correct position in the anteroposterior (A) and lateral (B) views.
Postoperatively, a non-weightbearing short leg splint was postoperatively applied for 2 weeks. Active and passive range of motion exercises of the ankle were permitted at 2 weeks postoperatively. Partial-weightbearing was allowed at 4 weeks postoperatively, and full-weightbearing at 6 weeks postoperatively. The patient was allowed to jog 8 weeks after surgery. After confirming that bone union was obtained on non-contrast CT (Fig. 5) and tenderness on the lateral side of the ankle had resolved, the patient was allowed to return to his original sport at 12 weeks postoperatively. Two years after surgery, the patient remained a competitive basketball player with no symptoms. Additionally, the AOFAS score had improved to 100 points.
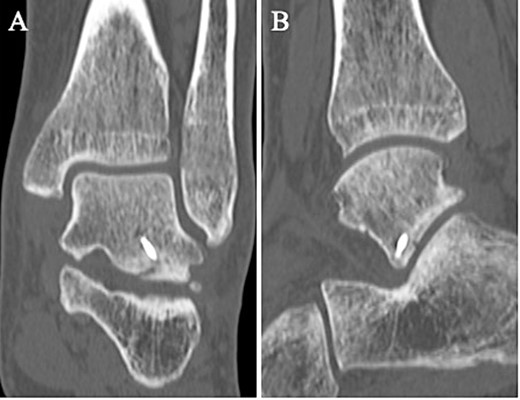
A non-contrast CT taken at 12 weeks postoperatively showed bone union in the coronal (A) and sagittal (B) views.
Discussion
Treatments for LPFT generally divide between conservative and surgical treatment [7, 8]. The choice of treatment is determined by the type of fracture, the size of the bone fragments, and the degree of bone fragment displacement [7–9]. In the case of non-displaced fractures, good results have been reported with conservative treatment such as cast immobilization and non-weightbearing regardless of the fracture type [7, 9]. On the other hand, surgical treatment is applied for displaced fractures, severe comminuted fractures, and instances of nonunion [7–9]. Surgical treatment for LPFT typically includes open reduction-internal fixation and bone fragment excision [7]. Especially in Type I fractures, where the dislocation of the bone fragment is >2 mm, open reduction-internal fixation is recommended [7]. There have been several recent reports of open reduction-internal fixation for Type I fractures with satisfactory results have been reported [10–12]. However, an open approach carries a higher risk of complications such as infection, skin necrosis, nerve damage, and talar necrosis [13]. In addition, the open approach makes it difficult to observe the intraarticular surface and may complicate the precision required to anatomically reduce the bone fragment [13]. To our knowledges, there is only one case report of LPFT treated with arthroscopic reduction-internal fixation. Funasaki et al. [9] successfully treated a patient with Type I LPFT using arthroscopic reduction-internal fixation. Additionally, this report has demonstrated that arthroscopic surgery can provide precise anatomical reduction and allows for an early return to pre-injury daily and sporting activities.
In this case, surgical treatment was indicated because the fracture was Type I and the bone fragment was also displaced >2 mm. Because of the high risk of complications associated with the traditional open procedure and the difficulty of directly observing the fracture site, the surgery was performed under arthroscopy. As a result, at 12 weeks postoperatively, the patient was able to return to his original sport at his pre-injury level without symptoms, complications, or functional impairment.
In conclusion, we reported a case of LPFT in a 24-year-old male basketball player who was successfully treated with arthroscopic reduction-internal fixation. This surgical technique may be a useful option for the treatment of Type I LPFT with bone fragment displacement of more than 2 mm.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Funding
None declared.
Data availability
Not applicable.



