-
PDF
- Split View
-
Views
-
Cite
Cite
Suphalerk Lohasammakul, Apram Jyot, Kongkrit Chaiyasate, An approach to achieve tension-free closure and mitigate recurrence in the management of recurrent cervical keloids, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae222, https://doi.org/10.1093/jscr/rjae222
Close - Share Icon Share
Abstract
Keloid is a burdensome condition that negatively affects patient’s quality of life. It is influenced by a spectrum of risk factors, including tension. We propose an approach to address the tension-free closure and optimize surgical outcomes in neck keloid. A retrospective review of neck keloid patients who underwent surgical treatment between 2014 and 2022 was performed. Five patients underwent surgical interventions. Two patients had sufficient and three had insufficient tissue redundancy. The former underwent keloid excision with tension-free closure. The latter underwent keloid excision with full thickness skin graft for tension-free closure. One patient required re-excision with free flap coverage. All patients received postoperative low dose radiation. All patients were satisfied with the results and there were no signs of keloid recurrence during the follow-up period. Tension during closure following keloid excision is a modifiable risk factor. An appropriate algorithm providing tension-free closure can minimize the recurrence.
Introduction
Scar formation is an intrinsic part of the body’s healing mechanism. Prophylactic measures are commonly employed prior to the full maturation of scars to enhance outcomes. Despite this, an abnormal fibro-proliferative response can lead to atypical scar formation such as hypertrophic scars and keloids—both being manifestations of abnormal healing process [1]. Distinguishing between these two can be challenging, although histopathological markers can aid in differentiation; keloids, for instance, are often identified by the presence of alpha-smooth muscle actin (alpha-SMA), although this is not universally observed [2]. Clinically, keloids can be identified by their characteristic growth beyond the original wound boundaries [3–5]. Keloid development is influenced by a spectrum of risk factors, ranging from local aspects like wound location and tension, to systemic factors including skin type, hormonal influences, and genetics [4, 6–9]. This complexity contributes to the treatment challenge, which bifurcates into medical and surgical interventions [10].
Surgical excision, when used as a standalone treatment for keloids, has been shown to result in a recurrence rate exceeding 50%, and the reduction of wound tension through surgical techniques has not been substantiated by data to decrease the likelihood of recurrence [10]. Thus, it is substantiated that optimal outcomes require a combination of surgical and adjunct medical therapies [11, 12]. Neck keloids, in particular, pose a unique challenge due to the inherent tension in this highly mobile area, escalating the risk of recurrence regardless of systemic factors. The complexity of treating extensive neck keloids compounds the difficulty of achieving successful outcomes by limiting reconstructive options and increasing the potential for reconstruction failure compared to smaller, isolated keloids.
This article aims to outline an algorithmic strategy developed by the senior author for the management of cervical keloids, showcased through a series of cases that illustrate a spectrum of minor to extensive presentations.
Methods
We conducted a retrospective review of the medical records of patients with recurrent cervical keloids treated surgically by the senior author between 2011 and 2022. Our study adhered to the ethical principles outlined in the Declaration of Helsinki and received approval from the Corewellhealth institutional review board (approval number 2020-011). All the patients were informed and consented for participating in this study. Informed consent was obtained from all individual patients for whom identifying information and/or photographs.
Patients were stratified based on the size of their keloids and the anticipated size of the defect post excision. The reconstructive approach was aimed at achieving tension-free wound closure. The outcomes of the surgical interventions were assessed by examining the rates of keloid recurrence and evaluating the satisfaction levels of the patients. Prior to surgery, all patients were thoroughly informed about the possibility of additional follow-up surgical procedures.
Results
During the specified study period, five patients received surgical interventions for recurrent neck keloids. The specifics of each patient’s operation are detailed in Table 1. Here, we present three exemplary cases to illustrate the range of approaches taken. Patients were preoperatively assessed to determine the adequacy of tissue availability for tension-free closure. Two patients were considered as having sufficient tissue redundancy. Other three were classified as having insufficient tissue redundancy for tension-free repair. One patient, who had previously experienced recurrence following a full thickness skin graft and postoperative radiation therapy, was successfully treated with a free superficial circumflex iliac artery perforator (SCIP) flap reconstruction to achieve tension-free closure. During the follow-up period, one of patients were administered triamcinolone acetonide injections as a prophylactic measure against recurrence. All the patients reported high levels of satisfaction and there were no signs of keloid recurrence during the follow-up period.
| No . | Age . | Sex . | Keloid location . | Previous treatment . | Tissue redundancy . | Procedures . | Follow-up period . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | F | Pre- and postauricular area | Keloid excision 5 times laser steroid injections | Yes | Keloid excision with extensive undermining postoperative radiation | 4 years |
| 2 | 39 | F | Left neck | Keloid excision multiple times + steroid injection | No | Keloid excision with FTSG + postoperative RT | 9 years |
| 3 | 40 | F | Right neck and cheek | Keloid excision + RT Keloid excision + steroid injections | No | Keloid excision + FTSG + postoperative radiation + steroid injection keloid excision + SCIP free flap | 6 months |
| 4 | 42 | F | Left neck | I&D due to infected keloid 2 times | No | Keloid excision + FTSG + postoperative radiation | 6 months |
| 5 | 20 | M | Bilateral neck | Steroid injections | Yes | Keloid excision + postoperative radiation | 6 months |
| No . | Age . | Sex . | Keloid location . | Previous treatment . | Tissue redundancy . | Procedures . | Follow-up period . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | F | Pre- and postauricular area | Keloid excision 5 times laser steroid injections | Yes | Keloid excision with extensive undermining postoperative radiation | 4 years |
| 2 | 39 | F | Left neck | Keloid excision multiple times + steroid injection | No | Keloid excision with FTSG + postoperative RT | 9 years |
| 3 | 40 | F | Right neck and cheek | Keloid excision + RT Keloid excision + steroid injections | No | Keloid excision + FTSG + postoperative radiation + steroid injection keloid excision + SCIP free flap | 6 months |
| 4 | 42 | F | Left neck | I&D due to infected keloid 2 times | No | Keloid excision + FTSG + postoperative radiation | 6 months |
| 5 | 20 | M | Bilateral neck | Steroid injections | Yes | Keloid excision + postoperative radiation | 6 months |
FTSG, full thickness skin graft; SCIP, Superficial Circumflex Iliac Artery Perforator.
| No . | Age . | Sex . | Keloid location . | Previous treatment . | Tissue redundancy . | Procedures . | Follow-up period . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | F | Pre- and postauricular area | Keloid excision 5 times laser steroid injections | Yes | Keloid excision with extensive undermining postoperative radiation | 4 years |
| 2 | 39 | F | Left neck | Keloid excision multiple times + steroid injection | No | Keloid excision with FTSG + postoperative RT | 9 years |
| 3 | 40 | F | Right neck and cheek | Keloid excision + RT Keloid excision + steroid injections | No | Keloid excision + FTSG + postoperative radiation + steroid injection keloid excision + SCIP free flap | 6 months |
| 4 | 42 | F | Left neck | I&D due to infected keloid 2 times | No | Keloid excision + FTSG + postoperative radiation | 6 months |
| 5 | 20 | M | Bilateral neck | Steroid injections | Yes | Keloid excision + postoperative radiation | 6 months |
| No . | Age . | Sex . | Keloid location . | Previous treatment . | Tissue redundancy . | Procedures . | Follow-up period . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | F | Pre- and postauricular area | Keloid excision 5 times laser steroid injections | Yes | Keloid excision with extensive undermining postoperative radiation | 4 years |
| 2 | 39 | F | Left neck | Keloid excision multiple times + steroid injection | No | Keloid excision with FTSG + postoperative RT | 9 years |
| 3 | 40 | F | Right neck and cheek | Keloid excision + RT Keloid excision + steroid injections | No | Keloid excision + FTSG + postoperative radiation + steroid injection keloid excision + SCIP free flap | 6 months |
| 4 | 42 | F | Left neck | I&D due to infected keloid 2 times | No | Keloid excision + FTSG + postoperative radiation | 6 months |
| 5 | 20 | M | Bilateral neck | Steroid injections | Yes | Keloid excision + postoperative radiation | 6 months |
FTSG, full thickness skin graft; SCIP, Superficial Circumflex Iliac Artery Perforator.
Case 1: management of facelift scar keloids
A 70-year-old female patient was afflicted with keloids that had developed over her bilateral facelift scars from a surgery performed 20 years prior. The resulting scars were not only esthetically unpleasing but also painful and progressively enlarging, leading to five subsequent re-excisions. Unfortunately, each attempt was followed by recurrence at various intervals. In between these surgical interventions, the patient endured multiple sessions of laser therapy and steroid injections, all of which failed to yield improvement. The keloids caused significant discomfort, manifesting as pain and pruritus, which severely disrupted her daily activities.
Given the persistence of keloids despite conventional treatments [10], we opted for a combined approach of surgical excision followed by postoperative radiotherapy, a modality selected to minimize the likelihood of recurrence. To ensure the success of the primary closure, we employed strategies for scar minimization, chiefly aiming for tension-free suturing [13].
The procedure involved extensive undermining of the facial skin flaps towards the nasolabial, submental, and submandibular areas, enabling a relaxed repositioning of the cheek flap over the postauricular incision. To avoid possible facial nerve damage in a patient with a history of facelift surgery, sub-superficial musculoaponeurotic system (sub-SMAS) dissection was deliberately avoided [14]. The skin was approximated using atraumatic techniques to ensure everted wound edges and precise alignment. Subsequently, the patient underwent low-dose postoperative radiotherapy administered over 3 days (total dose of 12 Gy), which is advocated for reducing keloid recurrence rates [11, 15].
The patient’s post-treatment recovery was unremarkable, with no reported complications. The wound healing progressed smoothly, and the patient experienced complete resolution of pain and pruritis. Moreover, there was no sign of keloid recurrence at the 4-year follow-up. Figure 1 showcases the comparative documentation of her pre- and post-operative outcomes.
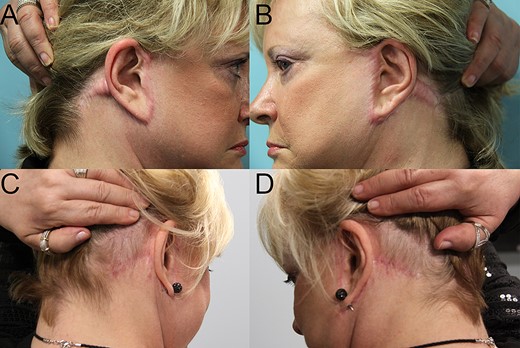
Bilateral cervical and preauricular keloids. Pre- (A and B) and post-operative 4 years (C and D) pictures after keloid excision, reconstruction with redo facelift, and postoperative radiotherapy.
Case 2: submandibular keloid management with postoperative challenges
A 50-year-old female with a chronic history of keloid formation in the left submandibular region presented to our emergency department in 2012 due to an infection of the keloid. Her medical record revealed a pattern of recurrent infections and multiple failed interventions, including surgical excisions and steroid injections. After initial management with antibiotics, we scheduled her for further surgical evaluation.
In a subsequent visit, she underwent surgical resection of a sizable keloid scar, measuring 20 by 8 cm. The defect was reconstructed using a full-thickness skin graft (FTSG) harvested from her left lower abdomen [16, 17]. To mitigate the risk of keloid recurrence, immediate postoperative radiation therapy was administered starting on the day of the operation and continuing for three consecutive days [11]. Despite experiencing some epidermolysis likely related to the radiation, the graft showed a 100% take to the wound bed.
Five months post operation, we noted hypertrophic scarring along the wound margins. This complication was managed effectively with serial injections of kenalog, resulting in a satisfactory response. The patient experienced no pain or pruritus post-treatment until the 9-year follow-up. Figure 2 illustrates her pre- and post-operative states, including the discoloration noted in the grafted skin.
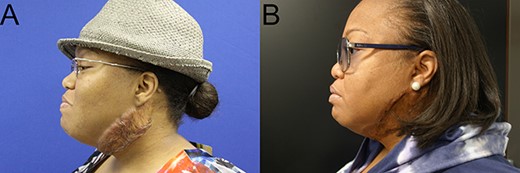
Cervical keloids. Pre- (A) and post-operative 9 years (B) pictures after keloid excision, reconstruction with FTSG, and postoperative radiotherapy.
Case 3: comprehensive management of recalcitrant mandibular keloid
A 43-year-old female presented with a history of a recurrent keloid on her right mandibular area. Initially treated with keloid excision and postoperative radiotherapy at another facility years prior, her keloids unfortunately reappeared within a few months. Subsequent treatments, including further keloid excision with primary closure and steroid injections were to no avail. The keloids recurred, presenting with increased itching and pain.
In view of her repeated recurrences post-treatment, we approached her condition with a more aggressive strategy. We performed another keloid excision and covered the defect with a full-thickness skin graft measuring 8 by 9 cm, followed by a comprehensive postoperative radiotherapy regimen, delivering a total dose of 20 Gy. Additionally, she received multiple sessions of steroid injections in an effort to prevent recurrence. Despite these efforts, the keloid returned after 4 years, now even larger at 10 by 11 cm. Given the patient’s history of keloid persistence, particularly in a region prone to movement, we recommended free tissue transfer as a definitive reconstructive option to achieve tension-free wound closure. She underwent keloid excision followed by reconstruction with a SCIP flap. Considering her previous two rounds of radiotherapy, we opted not to administer postoperative radiotherapy to avoid the risks of radiation overexposure.
The postoperative recovery was smooth, and the patient experienced a significant improvement in quality of life, reporting no pain or itching. At her last follow-up, at 6-month post-surgery, there was no evidence of keloid recurrence. Figure 3 showcases her transformative journey from preoperative presentation to postoperative healing.

Recalcitrant cervical keloids. Pre- (A) and postoperative 4 years (B) pictures after keloid excision, reconstruction with FTSG. Postoperative 6 months (C) pictures after second keloid excision, reconstruction with SCIP free flap.
Discussion
Keloids are pathological overgrowths of scar tissue that relentlessly expand beyond the original wound boundary, often without any tendency to regress. This abnormal healing process not only detracts from esthetic appearance but can also result in functional limitations and psychological distress, cumulatively diminishing the quality of life. Recognized as a condition with multifaceted etiology [4, 6–9], we acknowledge that wound tension is a key modifiable risk factor. Our algorithm, depicted in Fig. 4, prioritizes strategies to achieve tension-free closure for neck keloids, with successful outcomes in the cases reported herein.
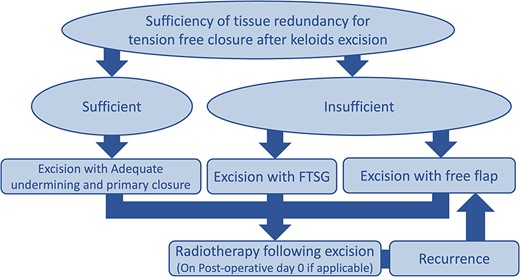
In cases where there is sufficient tissue redundancy, we advocate for subcutaneous undermining followed by primary closure. This approach generally yields tension-free wound closure and has been associated with satisfactory outcomes (as elaborated in Case 1).
Conversely, for keloids lacking sufficient adjacent tissue to allow primary closure, tissue transfer becomes necessary. FTSG is often the first line of consideration due to its simplicity and the brevity of operative time required. It is also favored over split thickness skin grafts because it typically results in less contraction and better cosmetic outcomes [18–20], which is particularly advantageous in the neck area where mobility can induce long-term tension. However, the monotherapy of keloid treatment has a notorious reputation for high recurrence rates [11]. This is evidenced by our patients’ previous unsuccessful treatments, which separately included keloid excision, laser therapy, and steroid injections. Since these standard treatments failed to prevent recurrence [10], we elected to incorporate postoperative radiotherapy to enhance our surgical approach and reduce recurrence rates [11, 15]. It should be noted, though, that skin grafts tend to be less resistant to radiotherapy [21], potentially leading to complications such as epidermolysis and graft discoloration issues that are less apparent in darker skin individuals (discussed further in Case 2). Another viable option is free tissue transfer. Although it is a more complex and time-intensive procedure, there is growing evidence of its efficacy for reconstruction post-keloid excision, albeit from limited case studies [22–24]. Notably, free flaps are more resilient to radiotherapy, which can be safely administered even within the first 24 h post operation [24].
Author contributions
Suphalerk Lohasammakul (Formal analysis, Methodology, Writing—original draft), Apram Joyt (Conceptualization, Writing—review & editing), and Kongkrit Chaiyasate (Conceptualization, Supervision, Writing—review & editing)
Conflict of interest statement
The authors have no conflicts of interest or products that are used in this manuscript.
Funding
The authors have no financial disclosures to declare.



