-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Dahman, Lina Abusulayman, Norah Alharbi, Faisal Joueidi, Omer Abdulrahim, Mohammed Al-Omran, Open repair of transverse cervical pseudoaneurysm, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae216, https://doi.org/10.1093/jscr/rjae216
Close - Share Icon Share
Abstract
A 40-year-old woman was referred to the vascular surgery clinic complaining of right shoulder pain and swelling secondary to blunt trauma 4 months ago. Computed tomography angiography showed a partially thrombosed supraclavicular pseudoaneurysm adjacent to the subclavian artery measuring 4.5 × 4 × 3.1 cm. Open repair surgery with resection of the pseudoaneurysm was successfully performed without injury to the capsule. Patient was stable and discharged 2 days later with no complications.
Introduction
Arterial pseudoaneurysms are false anyeurysms caused by arterial wall damage, mostly from iatrogenic or traumatic cause. Cervical and thoracic pseudoaneurysms are most commonly arise as a consequence of arterial or venus access procedures, anastomotic failure, trauma, and infection [1].
Symptoms are nonspecific ranging from massive hemothorax, shock, dysphagia, mild respiratory distress, and hemoptysis in delayed presentations. Subclavian pseudoaneurysms are extremely rare, and more often than not occur post chest trauma [2]. Unlike femoral and aortic psuedoaneuyrsms, the pathogenesis of subclavian artery pseudoaneurysms is less understood and even more so for transverse cervical artery pseudoaneurysms. Patient was informed and written consent was obtained for publication.
Case report
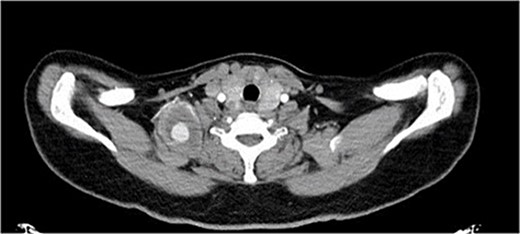
A 40-year-old female, who is a known case of type 1 diabetes mellitus, and hypothyroidism, on insulin and levothyroxine, was referred to our institute 4 months ago following trauma to her right shoulder from a falling drawer: complaining of swelling and pain around the right shoulder, palpable right distal pulses, and no discoloration or skin changes. Computed tomography angiography (CTA) showed partially thrombosed pseudoaneurysm at the right subclavian artery measuring 4.5 × 4 × 3.1 cm, most likely at the level of the costocervical trunk, specifically the highest intercostal artery (Figs 1 and 2). The subclavian artery and its branches were patent.
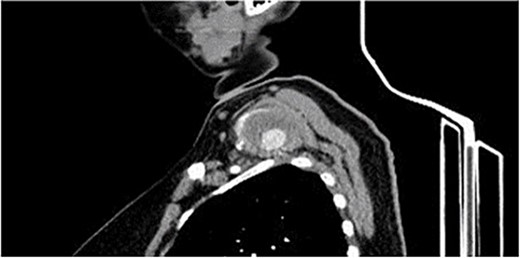
CTA, sagittal view showing the left supraclavicular pseudoaneurysm 4 × 3 cm.
The patient underwent open repair of the pseudoaneurysm. Procedure details: a 2 cm supraclavicular transverse incision was made, the subplatysmal flap was raised and the underlying fat pad was dissected, exposing the scalenus anterior muscle. Pseudoaneurysm was found on the transverse cervical branch of the subclavian, imbedded within the scalenus medius muscle. C-5, C-6, and the long thoracic nerves were identified (Fig. 2). Pseudoaneurysm was mobilized, inflow was controlled by 2–0 silk stitch and clips. The pseudoaneurysm was resected completely (Figs 3 and 4). The patient tolerated the procedure and was discharged without reported complications.
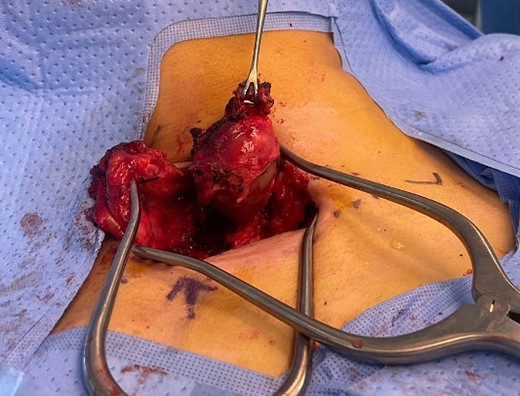
The supraclavicular incision and well-capsulated pseudoaneurysm with scalene muscle fully dissected intraoperatively.

Discussion
The transverse cervical artery also called the cervicodorsal trunk is one branch of the thyrocervical trunk, which arises from the first part of the subclavian artery.
Previously reported cases were pseudoaneurysms formed after temporary venous catheter placement in the internal jugular vein using a blind landmark-guided technique. These cases were initially diagnosed using color doppler ultrasound and confirmed with angiography [3–5]. Two cases were treated with endovascular approach using coil embolization, one case was treated with surgical ligation [3–5]. One case of massive bleeding caused by transverse cervical artery pseudoaneurysm was reported arising 3 weeks after a radical neck dissection and was treated successfully with emobolization therapy [6]. Cases of true aneurysms of the transverse cervical artery are exceedingly rare but have been reported in association with neurofibromatosis and Klippel Trenaunay syndrome, with the former treated by coil emobolisation and the latter by surgical exploration [7, 8].
The treatment for subclavian artery pseudoaneurysms is either by open or endovascular approach. The goal in open surgical repair is to resect the aneurysm while maintaining continuity of blood flow [9]. Exposure of the artery is challenging due to its location and anatomy, as it is adjacent to the clavicle or sternum [10]. Sternotomy aids in the exposure of intrathoracic aneurysms and supra/infra-clavicular incisions can be used in extrathoracic aneurysms. In some cases, clavicular resection is considered [9]. The need for manipulation of peri-clavicular anatomy may injure the brachial plexus and adjacent vessels, contributing to morbidity and mortality with open surgical repair [11]. Other options include endovascular treatment [3, 12], but long-term outcomes of this approach in subclavian artery pseudoaneurysms are limited [13]. Guidelines for treatment of subclavian artery pseudoaneurysms and branch pseudoaneurysms have not been established, but both open and endovascular approachs may be adopted dependent on their location and configuration [9, 13]. Regardless of approach, all anyeursms must be treated irrespective of size. In this case, open surgical resection was chosen due to the pressure effects of the pseudoaneurysm sac in close proximity to the brachial plexus, which would continue to cause symptoms if endovascular intervention was used.
Conclusion
Traumatic transverse cervical artery pseudoaneurysms are exceptionally rare because of their etiology, anatomical location, and time frame, as in our case. Due to the rarity of such cases, the approach to investigations and management is limited to similar cases. CTA was recommended to delineate the exact site of the pseudoaneurysm and outline the vascular anatomy. Because of the size, location, and symptoms of the patient, open repair surgery was the preferred approach for this case.
Conflict of interest statement
None declared.
Funding
None declared.



