-
PDF
- Split View
-
Views
-
Cite
Cite
Maximiliano Tellez-Zarate, Javier Meza-Hernandez, Edgardo Jimenez-Fuentes, Neuroganglioma in the posterior mediastinum: an incidental discovery, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae156, https://doi.org/10.1093/jscr/rjae156
Close - Share Icon Share
Abstract
Ganglioneuroma, a rare benign neuroblastic tumor, typically arises in the posterior mediastinum, but it can be found in the anterior mediastinum and thymus. Predominantly affecting the young, these asymptomatic tumors are often discovered incidentally through imaging. In our reported case, a 44-year-old woman post-hysterectomy with persistent jaundice was diagnosed with a neuroganglioma in the right posterior mediastinum via a computed tomography (CT) scan. Thoracotomy and resection revealed a 10-cm neuroganglioma untangled from mediastinal planes. Post-surgery, chylothorax emerged, which was managed through a 5-day fasting approach. Thoracic neurogangliomas, rare and often asymptomatic, demand meticulous diagnosis, emphasizing imaging and histopathology, with postoperative vigilance for complications.
Introduction
Ganglioneuroma is a benign neuroblastic tumor originating from neural crest cells. These usually occur in the posterior mediastinum, but they can also appear in the anterior mediastinum and thymus rarely [1]. These tumors are extremely rare, and cases have been reported mostly for young patients, which are often incidental findings in imaging studies due to their asymptomatic nature in most instances [2].
We present a rare case of thoracic neuroganglioma in an adult patient.
Case presentation
We present the case of a 44-year-old woman with 4 years post-hysterectomy for uterine fibroids, seeking urgent care for pain in the right lumbar region with nausea, asthenia, and jaundice persisting for a year. No other symptoms reported. She sought evaluation from a private physician, initiating a study protocol, including liver and bile duct ultrasound and laboratory tests.
Laboratory results showed abnormal liver function tests, characterized by elevated ALT and AST levels. The liver and bile duct ultrasound revealed hepatic steatosis and hepatomegaly without significant findings. Subsequently, a viral profile was conducted, yielding a positive result for Hepatitis A virus. Due to the persistence of lumbar pain symptoms, an external thoraco-abdominal computed tomography (CT) scan was performed, reporting a nodule in the posterior mediastinum measuring 8.2 cm, which was considered as an infiltrative and/or metastatic lymph node conglomerate (Fig. 1).
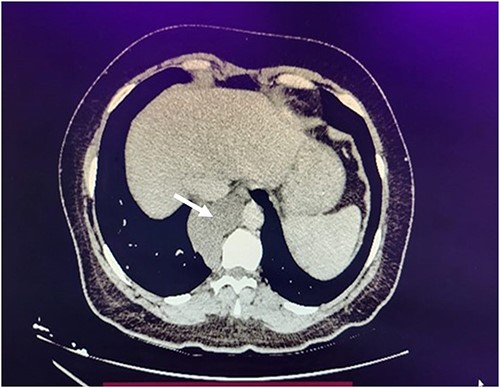
Axial chest computed tomography reveals an 8.2-cm nodule in the posterior mediastinum (white arrow).
She was referred to our unit, where we measured catecholamines. The results were negative, confirming it was not a functional paraganglioma. We then performed an image-guided biopsy, which revealed a lesion suggestive of neuroganglioma upon histopathological examination. This led to the decision to protocolize a right posterolateral thoracotomy and resection of the neuroglioma by the thoracic surgery service.
We made a 15-cm incision in the right posterior scapular region, exposing a neuroganglioma measuring ~10 × 7 centimeters (Fig. 2). Situated in the right paravertebral posterior mediastinum, the tumor adhered to mediastinal planes. Careful dissection was carried out due to significant vascularity in the mediastinal region, involving the ligation of vertebral vessels and precise cold cutting. Progressing toward the diaphragmatic surface, vessels were identified, ligated with silk 0, and cut using cold incisions. Two anthracotic nodules in the right upper and middle lung lobes were discovered, demonstrating carbon pigment accumulation without complications (Fig. 3). A 32 French posterior endopleural tube was carefully inserted, and this was complemented by the placement of a Jackson Pratt drainage system at the site where the tumor was removed.
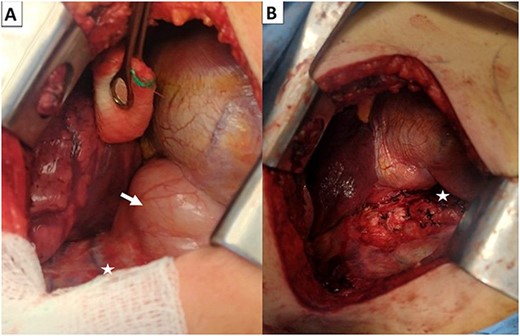
Right posterior thoracotomy before extracting the neuroganglioma (arrow) (A) and after extracting the neuroganglioma (B).
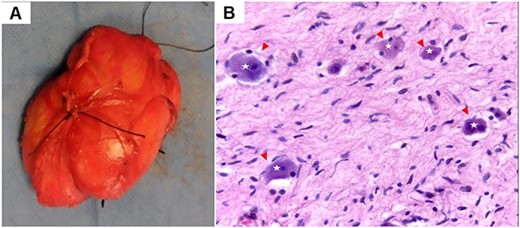
6.1 × 3.8 × 9.0-cm neuroganglioma extracted from the patient; (A) hematoxylin and eosin-stained slide at 4× and 40× magnification of the neuroganglioma; large ovoid cells with basophilic cytoplasm (star), surrounded by Schwannian stroma; (arrowhead) (B).
As a postoperative complication, the patient developed chylothorax, which was managed with fasting and parenteral nutrition for 5 days, achieving satisfactory resolution. The chest tube was removed, and a follow-up appointment was scheduled in the outpatient clinic.
Discussion
Few cases of thoracic neuroganglioma have been reported in the literature, which are often detected incidentally and become asymptomatic. The reported age median ranges from the first to the fifth decade of life [3, 4].
Symptoms manifest in 17.1%–73.4%, with prevalent issues like pain, swelling, gastrointestinal problems, neurological symptoms, hypertension, skin lesions, or bleeding, which are unrelated to tumor size. Symptoms exhibit variation based on the neuroganglioma’s location [4].
Imaging studies delineate neurogangliomas on tomography as either homogeneously or slightly heterogeneously hypodense lesions with calcifications, potentially leading to confusion with other pathologies [2]. Given the interpretive intricacies, there is a preference for completing the diagnosis through image-guided biopsy, boasting a 90% sensitivity for thoracic pathology [5].
The definitive treatment for thoracic neurogangliomas involves surgical extraction, with thoracotomy deemed as the optimal approach, allowing timely intervention in case of operative complications [6]. Postoperative monitoring is crucial, given that complications, although occurring in <3%, may be severe—such as pulmonary edema or Harlequin syndrome resulting from sympathetic trunk injury [7, 8].
Conclusion
Thoracic ganglioneuromas are uncommon, necessitating consideration and inclusion in the differential diagnosis when appropriate. Relying on imaging studies and histopathology is crucial for an accurate diagnosis. Similarly, during surgery, meticulous care of the structures surrounding the neuroganglioma is essential to minimize complications.
Acknowledgements
To all surgical team at General Hospital ‘Dr Manuel Gea Gonzalez’.
Author contributions
Maximiliano Téllez-Zárate, MD, wrote the paper and contributed to the analysis. Javier Meza-Hernández, MD, wrote the paper and contributed to the data. Edgardo Jiménez-Fuentes, MD, critically revised the manuscript.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
All relevant data supporting the findings of this case report are included directly within the manuscript. No external access is required, as all pertinent data are presented integrally in the body of this document.



