-
PDF
- Split View
-
Views
-
Cite
Cite
Caroline McBurney, Susan Zhang, Sharon Morris, Nodular fasciitis of the orbit: rapid growth phase post iatrogenic incisional trauma, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae023, https://doi.org/10.1093/jscr/rjae023
Close - Share Icon Share
Abstract
Nodular fasciitis (NF) is a benign, reactive, myofibroblastic proliferative solitary lesion that commonly develops in the subcutaneous or superficial fascia. We present a case of a 35-year-old male with a rapidly enlarging upper eyelid mass postiatrogenic incisional trauma. Subsequent en toto excisional biopsy demonstrated NF. Given the rapid clinical course of this patient and the reactive nature of NF, we hypothesize that the initial incisional trauma likely incited an inflammatory response resulting in rapid proliferation and growth of the lesion. NF accounts for <1% of all orbital lesions, and is often a clinically and pathologically difficult diagnosis to make given its propensity to mimic other benign and malignant conditions. Therefore, we recommend that en toto biopsies of orbital lesions in this anatomical area be performed rather than incisional biopsies.
Introduction
Nodular fasciitis (NF) is a benign, reactive, often self-limiting myofibroblastic proliferative solitary lesion [1]. It commonly develops in the subcutaneous or superficial fascia [1]. Lesions involving the head and neck account for 7%–20% of all NF cases [2]. Typical presentation is a rapidly growing solitary nodule, often measuring between 2 and 3 cm in size [1]. NF can occur in all age groups with no gender predilection, although it is most commonly seen in adults between the ages of 20 to 40 [2]. Given their rapid growth, high cellularity, increased mitotic activity and local infiltrative growth pattern, these benign lesions can often be misdiagnosed as a dermoid cyst or as more sinister pathology such as malignant sarcoma and lead to inappropriate management [1, 3]. Orbital NF is a rare occurrence accounting for <1% of all orbital lesions, adding further complexity to its diagnosis and compressive optic neuropathy is the most concerning sequalae for orbital lesions [4, 5].
Case report
A 33-year-old Caucasian male was reviewed by his general practitioner (GP) for a gradually enlarging mass at the medial aspect of the left upper eyelid. His GP performed an incision and drainage for a suspected infected sebaceous cyst. Seven weeks later, the patient presented to a tertiary hospital emergency department with wound dehiscence, purulent discharge and enlarging palpable mass; and was subsequently referred to ophthalmology.
Apart from the incision and drainage, there was no preceding trauma or any contributory past medical or ocular history. On examination, a 1.3 mm × 8 mm firm, non-erythematous, non-tender, tethered palpable mass over the left medial canthus and upper eyelid was noted. Palpebral aperture of the left eye was reduced to 4 mm, in comparison with 8 mm on the right. Visual acuity was 6/6 in the right eye and 6/12 pinhole to 6/9 in the left eye with normal intraocular pressures bilaterally. Anterior and posterior segments examination of the eyes were unremarkable. He had full range of extraocular eye movements with no proptosis, normal colour vision and full visual fields to confrontation. He had mild neuropraxia in the V1 distribution, and there were no palpable cervical or pre-auricular lymph nodes.
Initial incisional biopsy histopathology showed detached squamous epithelium and underlying subepithelial stroma with areas of inflamed granulation tissue and necrotic debris, with no evidence of dysplasia or invasive malignancy.
Computerised tomography (CT) and magnetic resonance imaging (MRI) were performed to further define the lesion as seen in Figs 1 and 2.

CT of the orbits demonstrated a 21 × 19 mm soft-tissue mass at the medial canthus with mass effect on the adjacent globe and no evidence of infiltration.
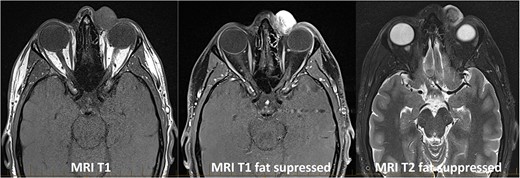
MRI of the orbits demonstrated a 20 × 18 mm well defined rounded mass arising within the medial canthus with no infiltration or bony erosion.
Anterior orbitotomy with complete excision of the mass was performed. Intraoperative findings demonstrated a large solid lesion with local inflammation and bony fixation with no clear capsule. Deep dissection to anterior superior orbit was performed, and the mass was carefully dissected off the surrounding nerves and vessels. Histological findings showed a proliferation of bland spindled, stellate cells arranged in fascicles with a fibrohistiocytic appearance. Occasional mitoses were noted. Immunohistochemistry demonstrated the cells were positive for SMA and calponin. AE 1/3, C-kit, CD34, Sox10, Melan-A, desmin and H-Caldesmon were negative. These morphological features and immunohistochemistry findings were consistent with a diagnosis of NF.
The patient healed well with no significant scar tissue. He had a temporary mild neuropraxia of the supraorbital nerve that settled. A follow up MRI at 12 months showed complete resolution of disease with no recurrence.
Discussion
To the best of our knowledge, this is the first reported case of iatrogenic trauma inciting a rapid growth phase in orbital NF. Prior to the initial incision and drainage, the mass was slowly enlarging over a number of months. Following incision and drainage, there was immediate, rapid growth of the lesion over the course of 7 weeks. This led us to hypothesize that trauma from the procedure likely incited an inflammatory response resulting in rapid proliferation and growth.
The exact aetiology of NF remains unclear. Historically, it was thought to be a reactive proliferative lesion with an association with previous trauma and subsequent inflammation [6]. However, only 10%–15% of cases in the literature are associated with trauma, as such it is unlikely to be the sole causative factor [6]. The recent identification of the recurrent gene rearrangement of ubiquitin-specific protease 6 (USP6) in ~90% of NF cases suggests a clonally proliferative nature [7]. Given the clinical course of our patient, it is possible that the pathogenesis of NF may be both reactive and clonally proliferative. Unfortunately, as testing for USP6 gene fusions is not part of current clinical practice, it is difficult to demonstrate this.
NF has no malignant potential and prognosis is excellent with complete marginal excision widely considered to be curative [8]. Recurrence is generally rare, however, in cases of recurrence some studies have reported the effective use of targeted steroid injections [8]. NF has also been shown to spontaneously regress without treatment [8]. Even in cases of partial excision, spontaneous regression has been reported [8]. It is still not well understood why spontaneous regression or resolution occurs in some cases, while in others proliferation occurs [8]. NF accounts for <1% of all orbital lesions, and it is a clinically and pathologically difficult diagnosis to make given its propensity to mimic more sinister pathology such as malignant sarcoma—of which, incisional biopsy is not advised [8]. Some studies have suggested using fine needle aspiration (FNA) in the diagnosis of NF, however, specific FNA-based diagnosis of NF remains challenging to definitively diagnose as benign, with uncertainty remaining in a significant number of cases [9]. Therefore, it is our recommendation that en toto biopsies of orbital lesions in this anatomical area be performed. This reduces the likelihood of misdiagnosis and inappropriate intervention, as well as reduces the likelihood of inciting a rapid growth phase.
Conclusion
The iatrogenic incisional trauma to our patient may have been an inciting factor leading to the lesion’s rapid growth phase and should be an important consideration for future cases with similar presentations. En toto biopsies of orbital lesions in this anatomical area should be considered rather than incisional biopsies.
Declaration of competing interest
The authors declare they have no conflicts of interest or financial disclosures in relation to this article.
Funding
No funding or grant support.
Informed Patient consent
Consent to publish the case report was obtained from the patient in writing. This report does not contain any personal information that could lead to the identification of the patient.



