-
PDF
- Split View
-
Views
-
Cite
Cite
Dominic Campano, Kaitlin Rush, Caleb Gottlich, Neil Jain, Bryan Bourland, Desirae Mckee, Dorsal lunate dislocation and en bloc proximal row carpectomy: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae043, https://doi.org/10.1093/jscr/rjae043
Close - Share Icon Share
Abstract
An unhelmeted 59-year-old male involved in a motorcycle accident presented with a right dorsal lunate dislocation in the context of a polytrauma evaluation. Soft-tissue attachments were minimal across the carpus, which allowed for an en bloc proximal row carpectomy. Two-year follow-up yielded a satisfactory outcome given the high energy injury mechanism. Proximal row carpectomy is a useful tool which preserves wrist range of motion in the acute trauma setting and is durable, as demonstrated by our patient’s postoperative mobilization using a wheelchair.
Introduction
Lunate and perilunate dislocations are uncommon injuries most frequently associated with high energy trauma. As classically described, Mayfield Stage IV injuries characteristically result in volar lunate dislocations (Table 1) [1]. This report details a case which deviates from normal with a resultant dorsal dislocation, extensive disruption of carpal ligaments, and an ipsilateral distal radius fracture. Given the severity of ligamentous disruption and the need for restoring patient mobilization, proximal row carpectomy (PRC) was performed to preserve wrist range of motion (ROM).
| Stage I | Scapholunate ligament disrupted |
| Stage II | Capitolunate ligament disrupted |
| Stage III | Lunotriquetral ligament disrupted. Entire carpus usually dislocates dorsally. |
| Stage IV | Radiolunate ligament disrupted and palmar lunate dislocation |
| Stage I | Scapholunate ligament disrupted |
| Stage II | Capitolunate ligament disrupted |
| Stage III | Lunotriquetral ligament disrupted. Entire carpus usually dislocates dorsally. |
| Stage IV | Radiolunate ligament disrupted and palmar lunate dislocation |
| Stage I | Scapholunate ligament disrupted |
| Stage II | Capitolunate ligament disrupted |
| Stage III | Lunotriquetral ligament disrupted. Entire carpus usually dislocates dorsally. |
| Stage IV | Radiolunate ligament disrupted and palmar lunate dislocation |
| Stage I | Scapholunate ligament disrupted |
| Stage II | Capitolunate ligament disrupted |
| Stage III | Lunotriquetral ligament disrupted. Entire carpus usually dislocates dorsally. |
| Stage IV | Radiolunate ligament disrupted and palmar lunate dislocation |
Case report
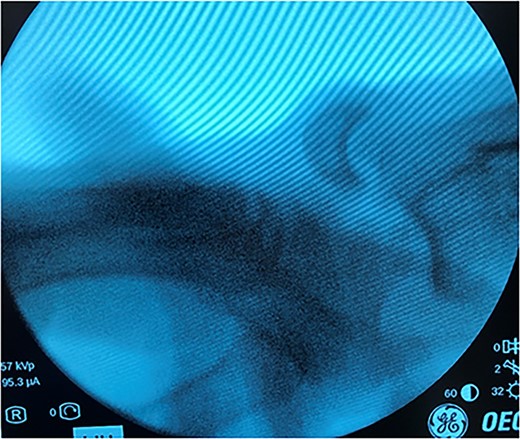
An unhelmeted 59-year-old male presented to the trauma bay at our institution after being involved in a motorcycle accident. This polytraumatized patient had been intubated prior to arrival and evaluation revealed numerous orthopedic injuries, including a right dorsal lunate dislocation (Fig. 1). Other injuries included a left distal femur fracture, left superior and inferior rami fractures, left APC II pelvic ring fracture, left closed tibia/fibula fractures, a Type III open right tibial shaft fracture, a right anterior column acetabulum fracture, and a Type I open right distal radius fracture. Traumatic subarachnoid hemorrhage to the bilateral frontal lobes, a unilateral occipital condyle fracture, a C1 fracture posterior arch fracture, a craniocervical dislocation, and numerous rib fractures were also noted. In addition to splinting all other peripheral injuries, the right distal radius fracture and lunate dislocation were closed reduced using a sugartong splint, with the wrist positioned in slight extension (Fig. 2).
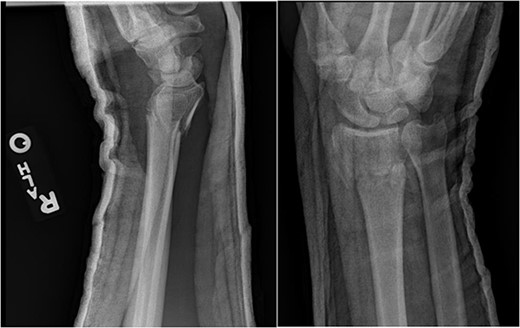
Anteroposterior (AP) and lateral views demonstrating the right distal radius and perilunate dislocation after closed reduction in the trauma bay.
After medical optimization, the patient underwent PRC, open reduction internal fixation (ORIF) of the right distal radius fracture, and carpal tunnel release. A dorsal approach was used, with the third and fourth extensor compartments being released. At this point, extensive disruption of the dorsal wrist capsule and proximal carpal row was observed. The lunate was identified, noted to be devoid of soft tissue attachments, and was able to be excised. Completion of the PRC was achieved by excising the scaphoid and triquetrum from their minimal remaining soft tissue attachments entirely through the dorsal approach (Fig. 3). The lunate fossa of the radius, proximal capitate, and radioscaphocapitate ligament (prerequisite for successful acute PRC) was noted to be intact [2].
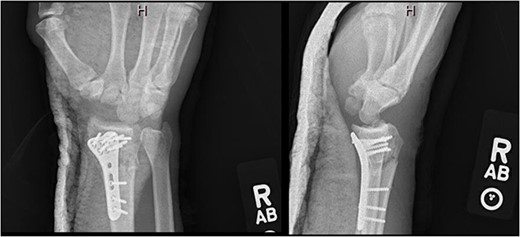
AP and lateral views immediately postop demonstrating right distal radius fixation and PRC.
At 3-month postoperative follow-up, grip strength was 18 lbs on the right and 25 lbs on the left. Pinch strength was 9 lbs on the left and 7 lbs on the right. At 5-month follow-up, the patient was transporting himself using a wheelchair, and his wrist pain was well controlled. At 7-month follow-up, grip strength was improved to 30 lbs on the right and 45 lbs on the left; pinch strength was 3 lbs on the right and 8 lbs on the left. Right wrist motion demonstrated 40° of flexion, 20° of extension, and full unlimited pronosupination. Radiographs demonstrated a healed distal radius fracture with no signs of arthrosis at the new radiocarpal joint (Fig. 4). At 1-year follow-up, the patient continued to progress functionally with no new complaints of pain. At 2-year follow up, the patient’s Disabilities of the Arm, Shoulder, and Hand score was 35.83.
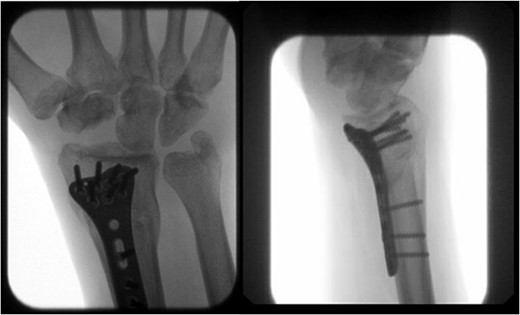
AP and lateral views at 7-month follow-up demonstrating a healed right distal radius fracture without arthrosis at the new radiocarpal joint.
Discussion
Injury pattern
The mechanism of injury in perilunate dislocations is typically forced wrist extension. These dislocations occur in a sequential fashion due to progressive ligamentous disruption and are classified according to the degree of perilunar instability [1]. The Mayfield classification described ligamentous disruption starting radially and progressing ulnarly (Table 1) (Fig. 5) [1]. In Stage IV injuries, the lunate typically dislocates volarly into the carpal tunnel through the space of Poirier. In this report, our patient’s injury deviated from normal with a dorsal dislocation.
![Right volar wrist demonstrating the pattern of progressive perilunate instability described by Mayfield et al. [1].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2024/2/10.1093_jscr_rjae043/1/m_rjae043f5.jpeg?Expires=1770173277&Signature=gsIv4SMUw-jnF4SF1~XyhIB3QVhRJVkb0AhqMeE7x~UJKWRJVyK52LipO60ljyBRq665M1fY2cY0waWkZbym9O1k7TC6TAG6SOrlI6C9DP8DlBJtnjmPRVMBFAv7-XMxqQKupG1lJRxxnv4lG4EsEsi-iwo6AHCcDFzPoprrzNxhogyh-CDnvC6p5vn758stuzJLCjWdj1Y-c8uvwX-WeGaPhUfvWBsxcFGdne3cYM7Lv5zJL5G6tYvALliyouBj08KUQajp0KL4B4XtU2~2EfFMvsQwYXvMtc19aBDJw4Mj6nYgalSkXTw~htG9HKr3iHaA5A23vmwBKIuIvVWxKw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Right volar wrist demonstrating the pattern of progressive perilunate instability described by Mayfield et al. [1].
Imaging
Radiographic imaging in volar dislocations may show a break in Gilula’s arc or a “piece of pie” sign due to the dorsal force causing palmar rotation on posteroanterior views [3]. Lateral views may demonstrate a “spilled teacup sign” or scapholunate angle >70° [3]. The case presented in this study was an obvious fracture and uncharacteristic dorsal dislocation. The Johnson classification would describe this as a lesser arc injury, as the surrounding ligaments of the lunate were involved with no fracture of other carpal bones [4].
Treatments
Treatment of volar lunate dislocations with closed reduction and percutaneous K-wire fixation has shown acceptable functional outcomes [5, 6]. Recent literature has also explored ligament reconstruction as an alternative [7].
Treatment options for dorsal lunate dislocations have not been broadly described. Neavin et al. reported a dorsal lunate dislocation with an ipsilateral radial styloid fracture, which was treated with ORIF and pinning [8]. This resulted in a sclerotic appearing lunate with partial avascular necrosis on magnetic resonance imaging (MRI), but yielded a good functional result. The authors hypothesized that preexisting arthritis of the scaphotrapeziotrapezoid and radiocarpal joints as well as an attenuated scapholunate ligament predisposed the patient to a dorsal dislocation [8]. Bilos et al. reported a dorsal lunate dislocation, which was pinned in place [9]. This resulted in radiographic sclerosis but no collapse of the lunate at 1 year [9]. Grip strength was similar to the unaffected side at final follow-up [9].
Arthrodesis rather than PRC or ORIF may be considered in chronic cases or cases with extensive lunate facet or capitate chondral injuries. Other treatments include attempting salvage—pinning the radiolunate joint to prevent ulnocarpal translation [10].
In this case, severe ligamentous disruption and the need for restoring patient mobilization favored using PRC. Over the course of 2 years, our patient demonstrated progressive improvement in function, and no signs of arthrosis at the new radiocarpal joint.
Outcomes
Previously reported acute perilunate dislocations treated with PRC had equal functional outcomes when compared to ORIF [11]. PRC resulted in good functional outcomes with failures typically occurring in younger patients under age 35 [12, 13]. Herzberg et al. reported poor outcomes in patients treated late (>45 days postinjury) and found that the incidence of posttraumatic arthritis was high (56%) among their 115 perilunate injuries [14]. Other studies have validated a decreased, but satisfactory ROM after PRC [15].
Wall et al. described long-term outcomes following PRC >10 years postoperatively [16]. Patient satisfaction was mostly favorable, with a 12% rate of conversion to radiocarpal arthrodesis at 10-year follow-up [16]. Younger age appeared to be associated with failure and conversion to fusion [16]. For this reason, it was concluded that the optimal candidates for successful PRC are aged 35–40 [16]. Our 59-year-old patient was older than this age range, but at 2 years postoperatively, demonstrated satisfactory functional progression.
Conclusion
In this report, severe ligamentous disruption and the need for restoring patient mobilization favored using PRC for treating a dorsal lunate dislocation. This was durable postoperatively, as the patient’s extensive lower extremity injuries led to heavy reliance on using the wrist for wheelchair mobilization. PRC proved to be an acceptable treatment choice which provided an option for early wrist function and ROM. Typical treatments requiring prolonged wrist immobilization may not be feasible in the polytraumatized or paralyzed patient with increased demands on upper extremity function to provide mobilization. These findings support the use of PRC for preservation of wrist ROM.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding
This research received no funds, grants, or other support from agencies in the public, commercial, or not-for-profit sectors.



