-
PDF
- Split View
-
Views
-
Cite
Cite
Ibtissam I E El Ouali, Soumiya S E El Graini, Omar O E El Aoufir, Soufya S B Belaabed, Amine A B Benkabbou, Laila L A Amrani, Meriem M B Bakkar, Youssef Y O Omor, Oumaima O L Lahnaoui, Sanae S A Amalik, Broncho biliary fistula, a rare complication after hepatectomy: case report of endoscopic and radiological management, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae657, https://doi.org/10.1093/jscr/rjae657
Close - Share Icon Share
Abstract
Bronchobiliary fistula (BBF) is one of the most exceptional complications following hepatic surgery. By integrating evidence-based case studies from existing literature, this review offers critical insights into the efficacy of diverse imaging modalities and therapeutic approaches across a broad spectrum of clinical scenarios. Computed tomography, and magnetic resonance cholangiography or even scintigraphy shows an abnormal tractus between biliary ducts and pulmonary bronchi and minimally invasive techniques using endoscopy are considered the techniques of choice. Surgery should only be considered in complicated cases due to significant morbidity and mortality rate. We report the case of a 46-year-old man with metastatic adenocarcinoma of the rectum involving the liver, treated with metastasectomy, which was complicated by a BBF. The patient underwent radiological external drainage followed by endoscopic placement of biliary endoprosthesis with favorable outcome.
Introduction
Bronchobiliary fistula (BBF) is a rare medical condition that was first described in 1850 by Peacock [1]. It consists of an abnormal communication between the biliary tract and the bronchial tree. Notably, the most reported etiologies arise from biliary tract obstruction, traumatic injury [2], hepatic abscesses, hydatid, or amebic liver infections [2]. The main clinical sign of BBF is a productive cough with yellowish sputum, known as biliptysis.
Case presentation
A 46-year-old male with a history of rectal adenocarcinoma and multiple liver surgeries due to metastases presented a new liver lesion. After a series of treatments, including radiofrequency ablation, radiotherapy, and chemotherapy, the patient underwent another non-anatomic liver resection. Although the immediate postoperative period was uneventful, the patient developed symptoms like fatigue, weight loss, fever, dyspnea, and biliptysis (Fig. 1) about 10 days after discharge. These symptoms suggested the development of a BBF.

Yellowish pigmentation of the patient’s tongue suggestive of biliptysis.
Upon further examination, the patient’s blood tests showed elevated inflammatory markers, and imaging studies revealed atelectasis in the right lower lung lobe, pleural effusion, and a subphrenic collection (Fig. 2). A computed tomography (CT) scan confirmed the presence of an intrahepatic collection communicating with the pleural cavity, indicating a potential BBF (Fig. 3) which was confirmed on magnetic resonance imaging (MRI) (Fig. 4). A drain was inserted under CT guidance (Fig. 5), and an endoscopic retrograde cholangiopancreatography (ERCP) revealed spontaneous bile leakage from the duodenal bulb. A stent was placed to drain the biloma (Fig. 6). Surgical intervention was avoided due to the patient’s liver condition.
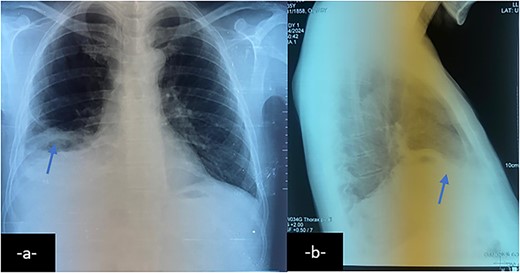
Chest X-ray on postero-anterior (a) and lateral views shows right basal atelectasis of the lung, right pleural effusion and sub phrenic collection with air-fluid level (arrow).
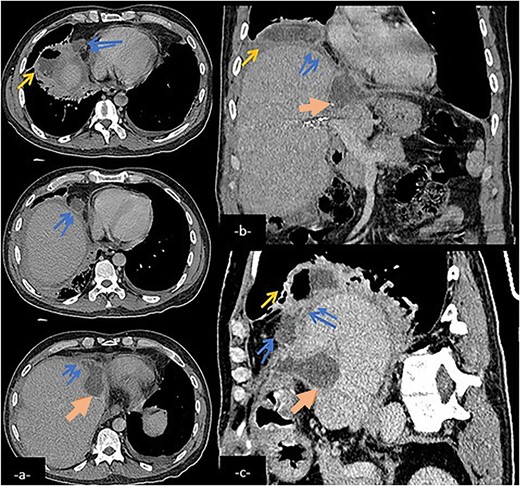
Abdominal CT scan in axial (a), coronal (b), and sagittal (c) reconstruction showing a biliary collection (large arrow) in the left hepatic lobe communicating with a subphenic and pleural collections with possible connexion with lower right airways (arrow) via a fistulary tract (double arrow).
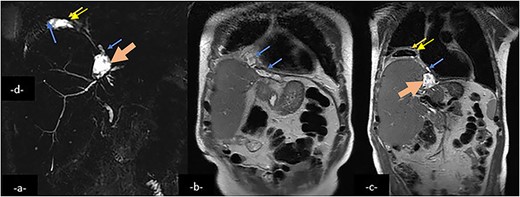
Magnetic resonance cholangio pancreatography (MRCP) in Radial T2 SSFSE sequence and coronal T2 showing a collection (large arrow) in the left hepatic lobe, subphrenic collection (arrow) and right pleural collection (double arrow) containing air and communicating with airways.
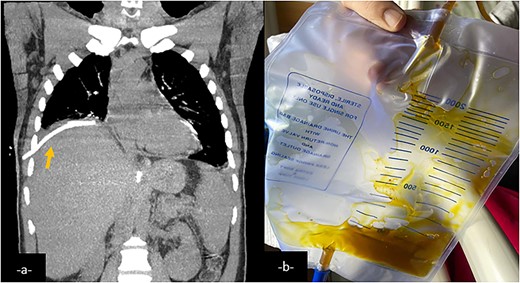
Coronal CT-scan reconstruction after an external drainage of the right pulmonary collection showing a decrease in size of it (a). External drainage finds a brownish fluid consistent with bile (b).
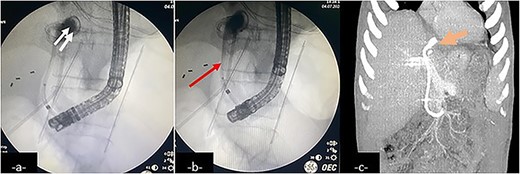
An endoscopic retrograde cholangiopancreatography (ERCP) showing contrast leakage from left-sided bile duct (a, double arrow) with duodenal fistula communicating with the biloma, drained by an inserted stent (b, arrow). Follow-up coronal CT-scan reconstruction after ERCP shows the internal drainage (c, large arrow).
The patient has been followed up for 6 months post-stent insertion and has remained symptom-free until today. Also, the pneumonia was treated with effective antibiotics, and no respiratory symptoms have been reported since.
Discussion
BBF is a rare condition predominantly observed in endemic regions as a complication of hydatid or amoebic disease.
A recent systematic review identified tumors as the most frequent cause (32.3%) of BBF formation [3], followed by bile duct obstruction (30.8%) [4]. Other etiologies include trauma [5] or iatrogenic injury [6], and congenital malformations [7]. The precise pathogenesis of BBF remains incompletely understood; however, elevated pressure within the biliary tree and local inflammation are recognized as major contributing factors. In the present case, an intrahepatic abscess induced adhesion formation between the diaphragm and the lung, which was considered the underlying cause of the BBF.
Procedures such as hepatic transplantation [6], trans arterial chemo-embolization, and radiofrequency ablation of primary hepatic tumors [8, 9] may also be associated with the development of BBF. Spontaneous BBF cases have also been reported.
Clinical manifestations of BBF include persistent cough, fever, mild jaundice, and often a history of liver pathology. The hallmark sign of BBF, biliptysis, is characterized by the expectoration of bitter-tasting or green-tinged sputum.
In most cases, imaging tests are necessary to confirm the diagnosis of BBF and to elucidate the anatomical situation prior to surgical intervention. The key imaging techniques for assessing BBF include ERCP, CT, and magnetic resonance cholangiography (MRC).
Chest X-ray may reveal dense opacities in the right lower lobe.
CT is the most frequently utilized imaging method to properly evaluate the upper abdomen and chest. It often reveal a subphrenic fluid collection, indicative of a biloma, right-sided pleural effusion, lacerations of the liver dome, diaphragm disruption, or dilated bile ducts in the presence of biliary obstruction [10]. However, the fistula itself is rarely visualized on CT.
MRI, including MRC, offers the advantage of multiplanar imaging capabilities and can effectively demonstrate distal biliary obstruction. However, it has limitations in visualizing nondistended ducts, which is often the case with BBF [11].
At ERCP, typical findings of BBF include the leakage of contrast material into the right-sided subphrenic compartment and right lower hemithorax. Bronchoscopy seldom reveals the fistula and is not essential for diagnosis or treatment. Percutaneous transhepatic cholangiography or ERCP have traditionally been performed to delineate the biliary anatomy before re-exploration and ductal repair [11].
Furthermore, biliary scintigraphy using hepatic iminodiacetic acid can demonstrate the migration of tracer activity from the liver to the chest cavity [11].
Complete drainage of the pleural, subdiaphragmatic, and perihepatic spaces is the first step in managing BBF. Eliminating any sources of inflammation and irritation, and reducing the pressure gradient responsible of ongoing bile drainage from the biliary tree to the bronchus is essential to ensure the closure of the fistula [12].
BBF due to benign causes, patients with a short life expectancy or those unable to tolerate open surgery are usually treated conservatively.
The successful resolution of symptom with the adjunctive use of octreotide in managing some cases of BBF has also been supported by reports [13].
Advanced techniques, such as histoacryl embolization under bronchoscopic guidance in the case reported by Honrubia Lopez et al. [14], has helped sealing the leakeage, improving the patient’s condition.
On the other hand, direct open repair remains the definitively curative treatment in more aggressive backgrounds of BBF like tumors, trauma, mechanical obstruction or in case of failure of prior conservative therapy [15].
It requires usually thoracotomy, relieving obstruction, fistulous tract resection. Fluid collection drainage and closure of the diaphragm defect adjunctive to viable tissue interposition between the lung and the diaphragmatic defect.
Multimodal treatments may be necessary for patients who underwent previous biliary reconstruction and that may include adjunctive percutaneous and surgical procedures.
Conclusion
This case highlights the complexity of BBF, a condition with varied causes and presentations. Non-surgical treatments are increasingly advocated as the initial approach. However, due to the diverse underlying conditions of patients with BBF, personalized and collaborative care approaches remain essential.
Acknowledgements
I, Ibtissam El Ouali, would like to express my gratitude to my professors and all the colleagues who participated in the completion of this work.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.



