-
PDF
- Split View
-
Views
-
Cite
Cite
Sylvie Nachtergaele, Laurine Mattart, Christophe Vindevogel, David Francart, Dominique Herman, Lionel Brescia, Gastric tube-preserving pancreaticoduodenectomy for ampullary adenocarcinoma after Lewis-Santy esophagectomy: a case report and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae610, https://doi.org/10.1093/jscr/rjae610
Close - Share Icon Share
Abstract
Pancreaticoduodenectomy after esophagectomy is a challenging procedure given the need to preserve the vascularization of the gastric plasty. We describe a case of a modified Longmire III procedure in a 68-year-old patient who underwent an esophagectomy with gastric conduit reconstruction in 2019 for esophageal adenocarcinoma. Two years later, an adenocarcinoma of the ampulla of Vater was diagnosed, necessitating pancreaticoduodenectomy with preservation of the gastric conduit. The patient presented no postoperative complications. Hepatic recurrence was observed 13 months after surgical resection. At 24 months follow-up, new liver metastases were observed. Preservation of the gastroduodenal and right gastric arteries was achieved, enabling conservation of the gastric plasty. Given the limitations of lymphadenectomy, the indication for this surgery must always be carefully considered. In the context of complex surgery, a complete preoperative workup to precisely determine the vascular anatomy as well as any anatomical variations is essential to establish the best operative strategy.
Introduction
With the improvement of surgical techniques and oncological follow-up, it is common to observe the appearance of a second primary tumor in the same patient.
Approximately 4% of patients develop a second cancer in the upper digestive tract after esophagectomy [1]. In the literature, some rare cases of pancreatic surgery after esophagectomy have been described. Indeed, pancreaticoduodenectomy according to Whipple is a complex and aggressive operation fraught with potential complications. The challenge is all the greater in view of the necessity to preserve the gastric plasty.
Case report
The patient, a 68-year-old male, had routine testing to monitor his esophageal cancer, well-differentiated pT1N0M0 adenocarcinoma.
In 2019, he underwent a Lewis–Santy esophagectomy with gastric tube reconstruction. Given the grade of the tumor, he did not receive adjuvant chemotherapy.
During the follow-up, a scan performed in late 2021 revealed suspected local pancreatic recurrence.
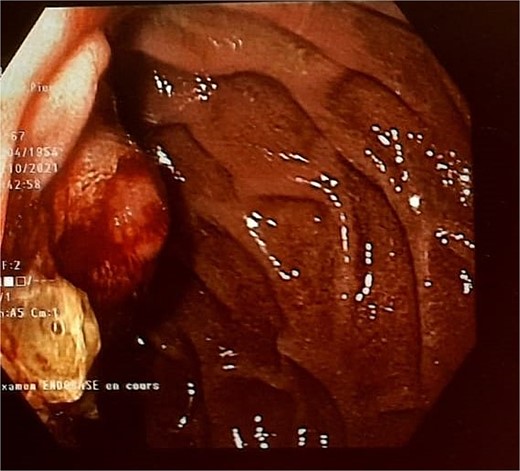
Endoscopic testing revealed a tissue lesion in the papilla (Fig. 1) and biopsies were positive for adenocarcinoma of the ampulla of Vater. An abdominal CT scan revealed dilatation of the Wirsung duct. The right gastroepiploic artery (RGEA), gastroduodenal artery (GDA), and right gastric artery (RGA) were not involved. The work-up for extension—including an MRI, 3-phase CT scan, and PET-CT scan—ruled out any distant lesions. Based on these results and after multidisciplinary discussion, it was decided to perform surgery since the clinical stage was cT2N0M0.
After a bi-subcostal laparotomy, extensive peritoneal exploration was performed and no metastasis was found, allowing the operation to proceed.
After an antegrade cholecystectomy, the common hepatic duct was dissected and transected 1 cm below the bifurcation, above the insertion of the cystic duct. The hepatoduodenal ligament was dissected, the hepatic and precaval nodes were sampled; the perioperative test was negative.
The GDA was isolated on its right anterolateral edge and supra-selective dissection of the intrapancreatic branches was performed. Ligation of the middle colic artery was required to correctly expose the RGEA, which was also preserved (Fig. 2).
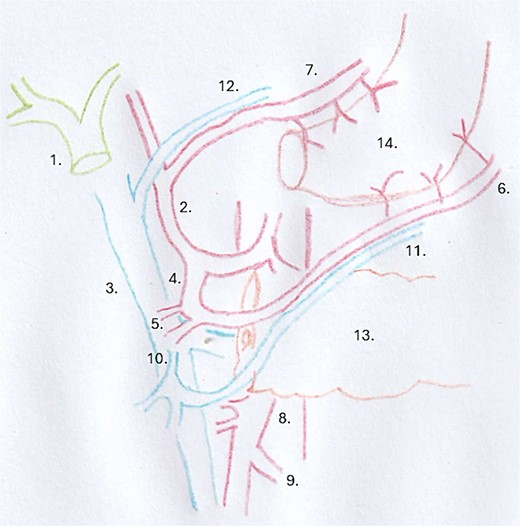
Surgical drawing: 1 = common hepatic duct, 2 = proper hepatic artery, 3 = portal vein, 4 = gastroduodenal artery, 5 = superior pancreaticoduodenal artery, 6 = right gastroepiploic artery, 7 = right gastric artery, 8 = superior mesenteric artery, 9 = middle colic artery, 10 = gastrocolic trunk of Henlé, 11 = right gastroepiploic vein, 12 = right gastric vein, 13 = pancreas, 14 = gastric plasty.
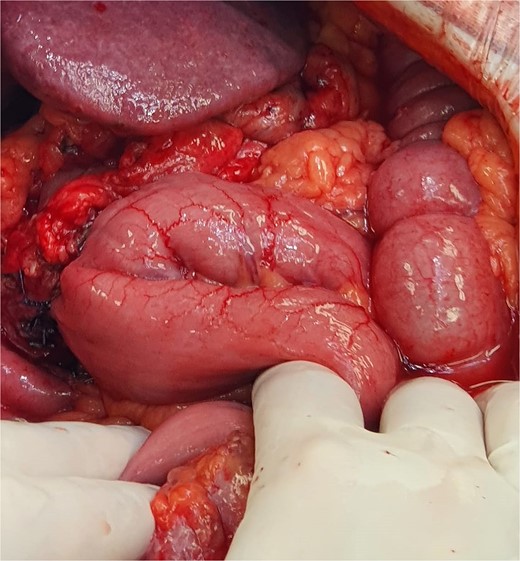
After separating the RGA and GDA from the posterior surface of the duodenal bulb, the bulb was transected 1 cm downstream of the pylorus using an endoGIA stapler, resulting in a pylorus-preserving pancreaticoduodenectomy (Fig. 3). Reconstruction consisted of pancreaticogastric, hepaticojejunal, and transmesocolic gastrojejunal anastomosis (Fig. 4). Throughout the procedure, blood flow through the gastric plasty was sufficient.
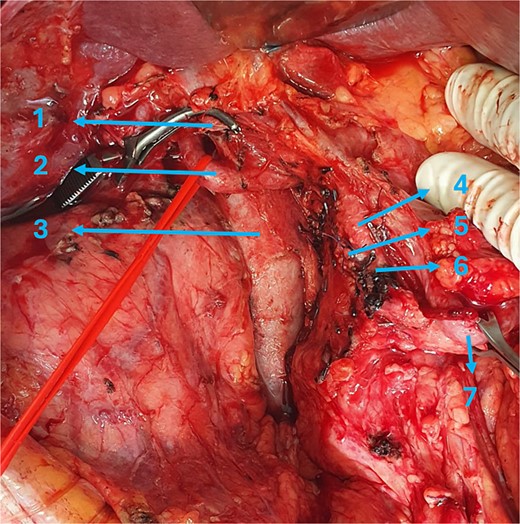
Intraoperative view: 1 = common hepatic duct, 2 = proper hepatic artery, 3 = portal vein, 4 = gastroduodenal artery, 5 = superior pancreaticoduodenal artery, 6 = right gastroepiploic artery, 7 = pyloric section.
The anatomopathological analysis revealed pT3bN0(0/19) MxV0L0Pn0R0 adenocarcinoma of the ampulla of Vater. The patient experienced no perioperative complications and was discharged on postoperative Day 12 under good conditions.
Adjuvant chemotherapy was recommended by multidisciplinary agreement but was refused by the patient. The patient experienced recurrence at 13 months with the appearance of two hepatic metastases on segments III and VII. Palliative chemotherapy was recommended at the expert center where the patient was initially treated. The patient finally underwent surgical resection of both lesions. In January 2024, 2 years after the pylorus-preserving pancreaticoduodenectomy, further hepatic recurrence was observed in the left liver.
Discussion
This article describes a complex surgical procedure in a patient with two cancers, esophageal adenocarcinoma treated with esophagectomy and, 2 years later, adenocarcinoma of the ampulla of Vater treated by gastric tube-preserving pancreaticoduodenectomy. Consequently, the patient underwent two major surgical procedures, known for their high morbidity rates. Modern surgical techniques and appropriate perioperative care have broadened the indications for these types of surgery while reducing complication rates [2].
The prognosis for periampullary cancers is poor and the only definitive treatment is complete resection [3]. Pancreaticoduodenectomy involves lymph-node removal of the GDA and RGA, vessels vascularizing the gastric tube after Lewis–Santy esophagectomy. In this context, we decided to preserve those arteries in this patient, in order to maintain the previous reconstruction. However, preserving the GDA might increase the risk of disease recurrence because the efficiency of lymph node dissection along the GDA may be compromised [3].
This operation might also prevent massive bleeding from the GDA stump in the event of pancreatic fistula. A third theoretical reason for choosing this technique is to prevent delayed gastric emptying as a result of preserving pyloric vascularization [2].
Nonetheless, the indication for this surgery is still very limited. In a Pubmed literature search, 15 cases of post- esophagectomy pancreaticoduodenectomy were identified after 2010 (Table 1).
| Author . | Year . | Age . | Sex . | Diagnosis . | Interval (m) . | Surgery . | Preservation . | Complications . | Recurrence & follow-up (m) . |
|---|---|---|---|---|---|---|---|---|---|
| Ando [4] | 2010 | 67 | M | Adenocarcinoma of the ampulla of Vater | 60 | PPPD | RGEA, RGEV, & GDA | None | No 36 |
| Yada [5] | 2010 | 77 | M | Duodenal adenocarcinoma | 204 | PD | GDA & RGEV | None | No 18 |
| Addeo [6] | 2011 | 73 | M | Pancreatic metastasis of renal cell carcinoma | 72 | PPPD | RGEA & RGEV | Pancreatic fistula | No 1 |
| Fragulidis [7] | 2011 | 50 | M | Pancreatic head adenocarcinoma | 156 | PPPD | RGEA & GDA | None | Yes (8) 14 |
| Inoue [8] | 2014 | 72 | M | Pancreatic head adenocarcinoma | 120 | PD | Reconstr GDA to RGEA & RGEV to LRV | None | No 6 |
| Okimoto [2] | 2014 | 70 | M | IPMN | 120 | PPPD | RGEA, RGEV, & GDA | Pancreatic fistula | No 2 |
| Nandy [9] | 2014 | 70 | M | Pancreatic head adenocarcinoma | 36 | PD | Data not available | None | Yes (2) 4 |
| Okochi [10] | 2015 | 70 | M | Pancreatic head adenocarcinoma | 60 | PD | Reconstr RGEA from MCA | None | No 8 |
| Orii [3] | 2019 | 79 | M | Pancreatic head adenocarcinoma | 60 | PPPD | RGEA, RGEV, & RGA | None | No 63 |
| Izumi [11] | 2019 | 78 | M | Pancreatic head adenocarcinoma | 84 | PD | RGEA, RGEV, & RGA | None | No 5 |
| Minagawa [12] | 2020 | 76 | M | Pancreatic head adenocarcinoma | 96 | PD | Reconstr RGEA from MCA | Gastro-jejuno stomy leak | No 15 |
| Appelbaum [13] | 2020 | 65 | M | Pancreatic head adenocarcinoma | 12 | PPPD | RGEA & RGEV | Pancreatic fistula | No 8 |
| Honig [1] | 2020 | 72 | M | Pancreatic head adenocarcinoma | 132 | PPPD | RGEA & RGEV | Duodeno-jejuno stomy leak | No 3 |
| Biesma [14] | 2021 | 77 | M | Bile duct carcinoma | 142 | PD | RGA | Gastro-jejuno stomy leak | No 24 |
| Watanabe [15] | 2022 | 78 | F | Pancreatic head adenocarcinoma | 396 | PD | Reconstr RGEA from GDA | Gastro paresis | Data not available |
| Our case | 2022 | 68 | M | Adenocarcinoma of the ampulla of Vater | 33 | PPPD | RGEA & GDA | None | Yes (13) 24 |
| Author . | Year . | Age . | Sex . | Diagnosis . | Interval (m) . | Surgery . | Preservation . | Complications . | Recurrence & follow-up (m) . |
|---|---|---|---|---|---|---|---|---|---|
| Ando [4] | 2010 | 67 | M | Adenocarcinoma of the ampulla of Vater | 60 | PPPD | RGEA, RGEV, & GDA | None | No 36 |
| Yada [5] | 2010 | 77 | M | Duodenal adenocarcinoma | 204 | PD | GDA & RGEV | None | No 18 |
| Addeo [6] | 2011 | 73 | M | Pancreatic metastasis of renal cell carcinoma | 72 | PPPD | RGEA & RGEV | Pancreatic fistula | No 1 |
| Fragulidis [7] | 2011 | 50 | M | Pancreatic head adenocarcinoma | 156 | PPPD | RGEA & GDA | None | Yes (8) 14 |
| Inoue [8] | 2014 | 72 | M | Pancreatic head adenocarcinoma | 120 | PD | Reconstr GDA to RGEA & RGEV to LRV | None | No 6 |
| Okimoto [2] | 2014 | 70 | M | IPMN | 120 | PPPD | RGEA, RGEV, & GDA | Pancreatic fistula | No 2 |
| Nandy [9] | 2014 | 70 | M | Pancreatic head adenocarcinoma | 36 | PD | Data not available | None | Yes (2) 4 |
| Okochi [10] | 2015 | 70 | M | Pancreatic head adenocarcinoma | 60 | PD | Reconstr RGEA from MCA | None | No 8 |
| Orii [3] | 2019 | 79 | M | Pancreatic head adenocarcinoma | 60 | PPPD | RGEA, RGEV, & RGA | None | No 63 |
| Izumi [11] | 2019 | 78 | M | Pancreatic head adenocarcinoma | 84 | PD | RGEA, RGEV, & RGA | None | No 5 |
| Minagawa [12] | 2020 | 76 | M | Pancreatic head adenocarcinoma | 96 | PD | Reconstr RGEA from MCA | Gastro-jejuno stomy leak | No 15 |
| Appelbaum [13] | 2020 | 65 | M | Pancreatic head adenocarcinoma | 12 | PPPD | RGEA & RGEV | Pancreatic fistula | No 8 |
| Honig [1] | 2020 | 72 | M | Pancreatic head adenocarcinoma | 132 | PPPD | RGEA & RGEV | Duodeno-jejuno stomy leak | No 3 |
| Biesma [14] | 2021 | 77 | M | Bile duct carcinoma | 142 | PD | RGA | Gastro-jejuno stomy leak | No 24 |
| Watanabe [15] | 2022 | 78 | F | Pancreatic head adenocarcinoma | 396 | PD | Reconstr RGEA from GDA | Gastro paresis | Data not available |
| Our case | 2022 | 68 | M | Adenocarcinoma of the ampulla of Vater | 33 | PPPD | RGEA & GDA | None | Yes (13) 24 |
PD = pancreaticoduodenectomy, PPPD = pylorus-preserving pancreaticoduodenectomy, IPMN = intraduct papillary mucinous neoplasm, RGEA = right gastroepiploic artery, RGEV = right gastroepiploic vein, GDA = gastroduodenal artery, LRV = left renal vein, MCA = middle colic artery, RGA = right gastric artery, M = male, F = female, m = months
| Author . | Year . | Age . | Sex . | Diagnosis . | Interval (m) . | Surgery . | Preservation . | Complications . | Recurrence & follow-up (m) . |
|---|---|---|---|---|---|---|---|---|---|
| Ando [4] | 2010 | 67 | M | Adenocarcinoma of the ampulla of Vater | 60 | PPPD | RGEA, RGEV, & GDA | None | No 36 |
| Yada [5] | 2010 | 77 | M | Duodenal adenocarcinoma | 204 | PD | GDA & RGEV | None | No 18 |
| Addeo [6] | 2011 | 73 | M | Pancreatic metastasis of renal cell carcinoma | 72 | PPPD | RGEA & RGEV | Pancreatic fistula | No 1 |
| Fragulidis [7] | 2011 | 50 | M | Pancreatic head adenocarcinoma | 156 | PPPD | RGEA & GDA | None | Yes (8) 14 |
| Inoue [8] | 2014 | 72 | M | Pancreatic head adenocarcinoma | 120 | PD | Reconstr GDA to RGEA & RGEV to LRV | None | No 6 |
| Okimoto [2] | 2014 | 70 | M | IPMN | 120 | PPPD | RGEA, RGEV, & GDA | Pancreatic fistula | No 2 |
| Nandy [9] | 2014 | 70 | M | Pancreatic head adenocarcinoma | 36 | PD | Data not available | None | Yes (2) 4 |
| Okochi [10] | 2015 | 70 | M | Pancreatic head adenocarcinoma | 60 | PD | Reconstr RGEA from MCA | None | No 8 |
| Orii [3] | 2019 | 79 | M | Pancreatic head adenocarcinoma | 60 | PPPD | RGEA, RGEV, & RGA | None | No 63 |
| Izumi [11] | 2019 | 78 | M | Pancreatic head adenocarcinoma | 84 | PD | RGEA, RGEV, & RGA | None | No 5 |
| Minagawa [12] | 2020 | 76 | M | Pancreatic head adenocarcinoma | 96 | PD | Reconstr RGEA from MCA | Gastro-jejuno stomy leak | No 15 |
| Appelbaum [13] | 2020 | 65 | M | Pancreatic head adenocarcinoma | 12 | PPPD | RGEA & RGEV | Pancreatic fistula | No 8 |
| Honig [1] | 2020 | 72 | M | Pancreatic head adenocarcinoma | 132 | PPPD | RGEA & RGEV | Duodeno-jejuno stomy leak | No 3 |
| Biesma [14] | 2021 | 77 | M | Bile duct carcinoma | 142 | PD | RGA | Gastro-jejuno stomy leak | No 24 |
| Watanabe [15] | 2022 | 78 | F | Pancreatic head adenocarcinoma | 396 | PD | Reconstr RGEA from GDA | Gastro paresis | Data not available |
| Our case | 2022 | 68 | M | Adenocarcinoma of the ampulla of Vater | 33 | PPPD | RGEA & GDA | None | Yes (13) 24 |
| Author . | Year . | Age . | Sex . | Diagnosis . | Interval (m) . | Surgery . | Preservation . | Complications . | Recurrence & follow-up (m) . |
|---|---|---|---|---|---|---|---|---|---|
| Ando [4] | 2010 | 67 | M | Adenocarcinoma of the ampulla of Vater | 60 | PPPD | RGEA, RGEV, & GDA | None | No 36 |
| Yada [5] | 2010 | 77 | M | Duodenal adenocarcinoma | 204 | PD | GDA & RGEV | None | No 18 |
| Addeo [6] | 2011 | 73 | M | Pancreatic metastasis of renal cell carcinoma | 72 | PPPD | RGEA & RGEV | Pancreatic fistula | No 1 |
| Fragulidis [7] | 2011 | 50 | M | Pancreatic head adenocarcinoma | 156 | PPPD | RGEA & GDA | None | Yes (8) 14 |
| Inoue [8] | 2014 | 72 | M | Pancreatic head adenocarcinoma | 120 | PD | Reconstr GDA to RGEA & RGEV to LRV | None | No 6 |
| Okimoto [2] | 2014 | 70 | M | IPMN | 120 | PPPD | RGEA, RGEV, & GDA | Pancreatic fistula | No 2 |
| Nandy [9] | 2014 | 70 | M | Pancreatic head adenocarcinoma | 36 | PD | Data not available | None | Yes (2) 4 |
| Okochi [10] | 2015 | 70 | M | Pancreatic head adenocarcinoma | 60 | PD | Reconstr RGEA from MCA | None | No 8 |
| Orii [3] | 2019 | 79 | M | Pancreatic head adenocarcinoma | 60 | PPPD | RGEA, RGEV, & RGA | None | No 63 |
| Izumi [11] | 2019 | 78 | M | Pancreatic head adenocarcinoma | 84 | PD | RGEA, RGEV, & RGA | None | No 5 |
| Minagawa [12] | 2020 | 76 | M | Pancreatic head adenocarcinoma | 96 | PD | Reconstr RGEA from MCA | Gastro-jejuno stomy leak | No 15 |
| Appelbaum [13] | 2020 | 65 | M | Pancreatic head adenocarcinoma | 12 | PPPD | RGEA & RGEV | Pancreatic fistula | No 8 |
| Honig [1] | 2020 | 72 | M | Pancreatic head adenocarcinoma | 132 | PPPD | RGEA & RGEV | Duodeno-jejuno stomy leak | No 3 |
| Biesma [14] | 2021 | 77 | M | Bile duct carcinoma | 142 | PD | RGA | Gastro-jejuno stomy leak | No 24 |
| Watanabe [15] | 2022 | 78 | F | Pancreatic head adenocarcinoma | 396 | PD | Reconstr RGEA from GDA | Gastro paresis | Data not available |
| Our case | 2022 | 68 | M | Adenocarcinoma of the ampulla of Vater | 33 | PPPD | RGEA & GDA | None | Yes (13) 24 |
PD = pancreaticoduodenectomy, PPPD = pylorus-preserving pancreaticoduodenectomy, IPMN = intraduct papillary mucinous neoplasm, RGEA = right gastroepiploic artery, RGEV = right gastroepiploic vein, GDA = gastroduodenal artery, LRV = left renal vein, MCA = middle colic artery, RGA = right gastric artery, M = male, F = female, m = months
If the GDA could not be preserved, vascular reconstruction was carried out. Okochi and his team performed vascular reconstruction by anastomising the RGEA stump with the right branch of the right middle colic artery due to local invasion [10]. The article by Minagawa et al. documents using the left branch of the middle colic artery to reconstruct the RGEA [12]. Inoue et al. performed microvascular reconstruction with anastomosis of the GDA to the RGEA and drainage from the right gastroepiploic vein into the left renal vein [8].
Most of the clinical cases found on PubMed did not present the prognosis and had fairly short follow-up. However, the study carried out by Orii et al. showed a recurrence-free survival period of >5 years [3]. Our study reached a follow-up of 24 months.
Two studies described recurrence at 2 [9] and 8 [7] months. All three studies involved patients with pancreatic adenocarcinoma. Only one of the case reports found in the Pubmed search involved adenocarcinoma of the ampulla of Vater [4]. In the case of our patient, who underwent pylorus-preserving pancreaticoduodenectomy and meticulous dissection limited by preserving the gastric tube, without adjuvant chemotherapy, recurrence was observed after 13 months, which is encouraging.
Conclusion
This case report highlights the relevance of a centralized, multidisciplinary approach to the management and follow-up of cancers with poor prognoses.
In the context of highly invasive surgery, a complete preoperative workup to precisely determine the vascular anatomy is essential to establish the best surgical strategy, which must be performed in a high-volume center.
Given the limited lymph node dissection associated with the preservation of the gastric plasty, the indication of pancreaticoduodenectomy after esophagectomy must always be carefully considered. Although difficult and risky, this surgery increases patient survival by offering an oncologically acceptable solution.
Conflict of interest statement
None declared.
Funding
None declared.



