-
PDF
- Split View
-
Views
-
Cite
Cite
Shmokh Alsalamah, Yazeed Jarman, Mohammd Alsanea, Mohammed Asiri, Riyadh Alhedaithy, Bilateral enlarged concha bullosa: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad508, https://doi.org/10.1093/jscr/rjad508
Close - Share Icon Share
Abstract
Concha Bullosa (CB) is a common sinonasal anatomical variant, which commonly extends into the middle turbinate. Generally, patients presenting with CB are asymptomatic and often incidentally diagnosed with a non-contrast computed tomography scan of the paranasal sinuses. In cases of extensive pneumatization, large CB may cause significant signs and symptoms—commonly, headaches, nasal obstruction, and hyposmia. With only a few reported cases of large CB in the literature; we herein, report a rare case of an unusually massive bilateral CB that resulted in complete obstruction of the left nasal cavity and partial obstruction of the right nasal cavity, in addition to a review of relevant literature.
Introduction
Nasal turbinates are important structures arising from the lateral nasal wall into the nasal cavity. There are three turbinates; superior, middle, and inferior. Turbinates play a key role in regulating airflow direction, humidification, warming, as well as filtering inhaled air through the nose [1]. Concha Bullosa (CB) is defined as hypertrophy and pneumatization within the nasal turbinates, often reported in the middle turbinate and less frequently in the superior or inferior turbinate. Variation in the incidence of CB has been reported in the literature, ranging from 14% to 53.6% [2, 3]. In the current paper, we describe a bilateral enlarged CB of the middle turbinate with complete unilateral nasal obstruction in a 22-year-old female, along with a review of current literature.
Case presentation
A 22-year-old female presented to our otolaryngology clinic with 3-year long complaints of bilateral alternating nasal obstruction and congestion more to the right side, associated with a mild to moderate intermittent, throbbing frontal headache and hyposmia. The patient’s quality of life was also affected due to sleep disturbance and mouth breathing. She denied any rhinorrhea, otorrhea, or otalgia. Patient is surgically and medically free. Upon examination, the patient had a severely deviated nasal septum to the right side, and bilateral enlarged turbinates with the left concha reaching to the nasal floor resembling polyp grade 4. For further evaluation, a non-contrast computed tomography (CT) of paranasal sinuses was performed. It revealed a right-sided deviated nasal septum with bilateral CB resulting in significant narrowing of the nasal cavity, with patent ostiomeatal complexes (Fig. 1). The option for surgical intervention was offered and explained to the patient, and the risks and benefits of the procedure were discussed thoroughly. Surgery was proceeded following patient’s approval. Under general anesthesia, the examination of the nose was performed using an endoscope and monitoring system, it showed a large left-sided CB extending through the nasal cavity reaching the nasal floor, right-sided CB reaching to the inferior turbinate, and a severely deviated nasal septum to the right side. Surgery started first with resection of the lateral part of the concha bullosa with the aid of turbinectomy scissor. Lower aspect of the medial part extending to the nasal floor was trimmed. After that, septoplasty was performed. Right CB was identified, the size was prominent reaching the inferior turbinate, it was removed with the same technique addressed earlier. Then bilateral turbinoplasty was performed. The patient tolerated the procedure and made an uneventful postoperative recovery. She was discharged in a stable condition with analgesia and hypertonic nasal saline irrigation. The patient was seen post-operatively and reported no active complaints, the nasal obstruction improved, no more sleep disturbance and headache free. However, the patient was still hyposmic. Endoscopic examination showed patent nasal cavity.
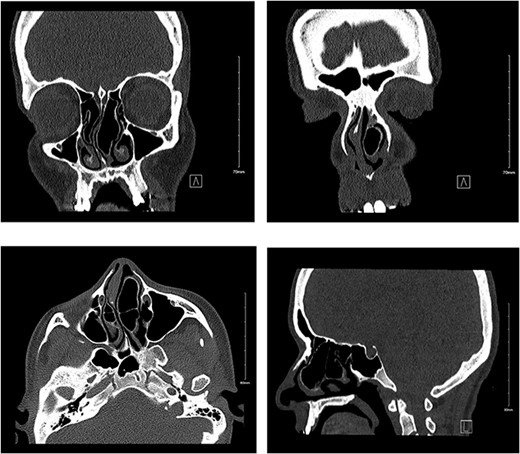
Non-contrast CT showing bilateral pnuematized concha bullosa, more prominent on the left pushing the nasal septum to the right side in coronal (a, b), axial (c), and sagittal (d) views.
Discussion
CB is a common sinonasal anatomical variant which is especially seen in the middle turbinate[2, 3]. Although the etiology of CB is still being investigated and ambiguous, various theories exist concerning the factors associated with their development. The ‘ex vacua’ theory is a possible mechanism which is associated with air flow patterns of the nasal passage. According to this theory, air flow decreases on one side of a preexisting septal deviation while it increases on the opposite side. Thus, conchal aeration on the opposite side of the deviation also increases[4]. Moreover, several studies reported a strong association between unilateral or dominant CB and contralateral nasal septal deviation[4, 5]. As in the case of our patient, a giant left CB and right septal deviation was seen together possibly due to reduced airflow in the deviated side and increased airflow in the opposite side.
According to a study conducted by Bolger et al., there are three possible types of CB; Lamellar concha, which can be defined by vertical lamellar pneumatization, bulbous type which is characterized by pneumatization of inferior segment. Third type is the extensive type defined as pneumatization of both components [6]. Nasr El-Din et al., conducted a study that included 488 Saudi patients with CB, which was prevalent in both males and females among the Saudi population, which was 55.4% and 55.7%, respectively. The prevalence of bilateral CB is 55.5%, which is more frequent as compared to the unilateral CB cases. The most frequent type observed is extensive CB (44.0%), as seen in our patient [7].
Patients with CB are typically asymptomatic and diagnosed incidentally upon imaging. It can, however, cause symptoms in cases of large CB where extensive pneumatization is noted, more significantly if it was bilateral CB. The most frequent presenting features of CB in these cases are sinus-related symptoms such as headaches secondary to mucosal contact [8, 9]. Nasal congestion, rhinorrhea, anosmia, facial pressure, and snoring are some symptoms seen as a result of blockage of sinuses [8]. Additionally, physical examination findings frequently show an intranasal mass or septal deviation. In conjunction with CT findings that may show bone remodeling and extranasal involvement, which may lead the physician to suspect a more sinister pathology[10].
Two similar cases to ours were described in the literature. The first case presented with headaches and right sided nasal obstruction. CT scan results have shown an enlarged air-filled middle turbinate with septal deviation and was managed by functional endoscopic sinus surgery (FESS) in which the lateral laminae were removed followed by septoplasty and conchoplasty[11]. The second similar case was reported by Perić A, et al. A case about a 32- year-old female presented with mild frontal headaches and right septal deviation. This patient underwent FESS in which a lateral laminectomy was performed followed by septoplasty [3]. However, both cases did not show the rare bilateral anatomical variation reported in our case.
Surgical approach is the definitive treatment of symptomatic CB. Several surgical approaches were described in literature in the management of CB such as turbinoplasty, partial/ total resection, crushing, and medial/ lateral laminectomy. Lateral excision of the middle turbinate is the most common technique in treating CB[12]. In a randomized controlled trial, lateral laminectomy and crushing had no negative effects on olfaction [13].
There are complications that can arise from CB if left untreated. CB possesses a mucociliary transport system, and upon obstruction, a mucocele can form and potentially become infected to develop into a mucopyocele[9]. Additionally, there were other associations that have been reported such as fungus balls and hemangiomas [14, 15].
Conclusion
Bilateral giant CB is a rare anatomical variation discovered on non-contrast CT. Nasal obstruction and headache are the most frequently reported symptoms. The gold standard treatment for giant CB is a surgical intervention, via an endoscopic technique. The outcome of surgery for this condition is excellent with rare recurrence.
Disclosures
Authors have no conflict of interests, and the work was not supported or funded by any drug company. This article (or any part of its contents) was not presented in any conference and was not published in any journal.



