-
PDF
- Split View
-
Views
-
Cite
Cite
Maris Niibek, Andrei Uksov, Liver transplantation for polycystic liver disease: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad507, https://doi.org/10.1093/jscr/rjad507
Close - Share Icon Share
Abstract
A 57-year-old man complained about abdominal distension and pain, constant feeling of early satiety. He was diagnosed with polycystic kidneys at the age of 24 and liver cysts discovered at the age of 38. The CT scan revealed 33 x 21 x 27 cm polycystic liver with cysts up to 7 cm in diameter. In 2009–2019 the patient was repeatedly punctured for liver cysts. Considering the continued enlargement of the liver and the worsening of complaints, the patient was put on the waiting list for a liver transplant in the spring of 2019. The patient went through liver transplantation on 11th of July 2022, the liver measures were 53 x 37 x 39 x 16 cm and weight 14,75 kg. The postoperative course was uneventful. Liver transplantation can be very effective treatment method that significantly improves the quality of life in PLD patients.
Introduction
Polycystic liver disease (PLD) is a rare hereditary disease that can occur as an isolated disease or be accompanied by autosomal dominant polycystic kidney disease (ADPKD) or autosomal recessive polycystic kidney disease (ARPKD) [1]. In isolated PLD, germline mutations occur in the PRKCSH and SEC63 genes, which are expressed on hepatocytes and cholangiocytes. These genes are in charge of making the proteins sec-63 and hepatocystin, which are responsible for fluid transportation and epithelial cell growth [2]. In ADPKD, gene mutations occur in 80% of cases in PKD1 and up to 10% of cases in PKD2 genes [3]. These genes are responsible for making polycystin and mutations of these genes leads to dysregulation of fluid secretion and abnormal cell growth [4].
The enlargement of the liver and pressure on the surrounding organs can cause shortness of breath, early fullness, abdominal enlargement, malnutrition, gastroesophageal reflux disease and back pain [1]. The obstruction of the venous drainage of the liver can cause portal hypertension, ascites, splenomegaly, bleeding from esophageal varices, jaundice and/or encephalopathy [4]. The diagnosis of PLD is made with imaging studies, the synthetic function of the liver is usually preserved in PLD [5, 6].
Treatment is indicated for patients who have symptoms caused by hepatomegaly or develop cyst complications such as cyst rupture, infection, bleeding or hepatic venous outflow obstruction [1].
Medical therapy consists somatostatin analogues, which inhibit the secretion of cyst fluid and hyperplasia of the bile duct cells, therefore inhibiting the growth of hepatic cysts [7]. Mammalian target of rapamycin inhibitors [8], ursodeoxycholic acid [9] and vasopressin-2 receptor antagonists [10] have shown delay on the growth of hepatic cysts in ADPKD patients.
Cyst aspiration and sclerotherapy is indicated for patients with a single giant cyst with rate of cyst volume and symptom remission 72–100% [11]. Transcatheter arterial embolization is used to embolize the branches of the arteries that supply blood to the cysts [1].
Surgical therapy consists cyst fenestration and hepatic resection. The extent of resection depends on the size and distribution of the cysts, hepatectomy can be used in patients with at least one liver segment that is not affected by the cysts. Liver transplantation is preserved for patients with severe symptoms and malnutrition, untreated complications and previously failed alternative interventions [1].
Case report
A 57-year-old male patient was diagnosed with polycystic kidneys at the age of 24 and liver cysts discovered at the age of 38. The patient’s mother was also diagnosed with polycystic kidneys and she has undergone a kidney transplantion.
Since 2009, the patient was complaining about abdominal distension, abdominal pain and constant feeling of early satiety. A CT scan showed cysts with a diameter of up to 7 cm all over the liver, the kidneys also had numerous cysts of different sizes. In the blood analysis AST, ALT, ALP and bilirubin were normal, there was a slight increase in GGT 128 U/L. Renal function was normal. A genetic analysis showed disease-related heterozygous missense mutation in the PKD1 gene.
Because of the complaints, the patient has been repeatedly punctured for liver cysts. In 2013, as a result of a car accident, the patient developed a rupture of a the right lobe liver cyst. A total laparotomy was performed due to intraperitoneal hemorrhage, which was later complicated by the development of an incisional hernia. Hernioplasty was performed in 2014 with an intra-abdominal mesh.
Over the years, the patient continued to experience an increase in abdominal girth. In the CT examination of 2017, the liver size was increased compared to the previous CT: the dimensions of the liver was 33 x 21 x 27 cm (Fig. 1). Considering the continued enlargement of the liver and worsening of symptoms, the patient was put on the waiting list for a liver transplant in the spring of 2019. Due to the lack of intensive care places during the COVID pandemic, he was temporarily off waiting list. Because of the worsening abdominal pain and malnutrition, markedly decreased exercise tolerance, the patient was again placed on the active waiting list for a liver transplant in May 2022.
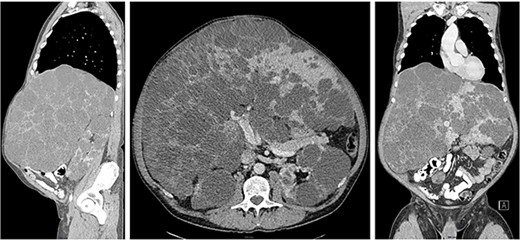
Computed tomography showed extremely enlarged liver with the dimensions of 33 x 21 x 27 cm.
Liver transplantation was performed on 11th of July 2022: massive hepatomegaly (Fig. 2) and extensive adhesions due to previous laparotomy and inicisional hernia repair made the release of the recipient’s liver very difficult. The duration of the operation was 413 minutes, the anhepatic time was 73 minutes, and the cold ischemia of the donor liver was 517 minutes. In the final histology, the liver measures were 53 x 37 x 39 x 16 cm and weight 14,75 kg (Fig. 3). Histologically, it was an adult polycystic kidney disease with liver involvement (polycystic liver disease), there were no signs of malignancy.

Massive hepatomegaly and previous operations made mobilization of the liver very difficult.

The final pathology revealed the liver measures 53 x 37 x 39 x 16 cm and weight 14,75 kg.
The postoperative course was uneventful and the patient was discharged home on the 29th postoperative day. The liver function has been good after transplantation. The patient developed incisional hernia, due to which incisional hernia repiar with intra-abdominal mesh was performed on March 2023.
Discussion
The treatment of PLD primarily depends on the patient’s symptoms and is mainly divided into three categories: drug therapy, percutaneous therapy and surgical therapy [1]. In case of liver cirrhosis, the liver is usually small and therefore easily manipulated during surgery. However, in the case of extremely large polycystic liver, it’s very difficult to mobilize the liver and get access to the liver hilum. If the liver normally weighs up to 2 kg, the average polycystic liver weights about 6,7 kg [12]. In this case, the liver weighed 14,75 kg. Extreme care must be taken when mobilizing the liver and visualizing the structures, as there is a high risk of injuring compressed and dislocated blood vessels, especially the inferior vena cava (IVC). Since the polycystic liver is very large, the classic approach with the excision of the recipient IVC instead of the piggyback technique should be preferred [13]. This case vividly demonstrates how liver transplantation is a very effective treatment method that significantly improves the quality of life in PLD patients.
Conflict of interest statement
We declare that there is no conflict of interests.
Funding
We declare that no funding was received in support of this work.



