-
PDF
- Split View
-
Views
-
Cite
Cite
Faez Ebrahim Nashawi, Ahmad Alkheder, Hamza Omar Shasho, Lava Abdullah, Adham bader aldeen Mohsen, An unusual route of odontogenic infection from the mandible to the orbit through the facial spaces, resulting in blindness: a rare case report, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad457, https://doi.org/10.1093/jscr/rjad457
Close - Share Icon Share
Abstract
Orbital infection is a rare complication of odontogenic infections, mostly originating from maxillary teeth. In our case, we present one of the unusual routes by which an odontogenic infection of a lower molar tooth has spread into the orbit. A 67-year-old uncontrolled diabetic patient was referred to our hospital with a complaint of a swollen right masseteric region and orbital infection following a dental procedure on the right mandibular third molar. Computed tomography scan and magnetic resonance imaging showed multiple abscesses localized in the masseteric and infratemporal spaces, extending into the orbital cavity through bony erosion in the lateral orbital with no sinus involvement. Improper treatment and poorly controlled diabetes resulted in the extensive spread of the infection. Clinical and radiological reevaluation has played a major role in the management of our case by elucidating the route of infection and localizing abscess foci accurately.
INTRODUCTION
Most cases of orbital infection are complications of paranasal sinusitis. A small percentage of cases are caused by infections of the middle ear, eyelids, tonsils, intracranial areas or odontogenic structures, either directly by the spread through local tissue planes or via the lymphatic and vascular systems [1]. Odontogenic orbital infections usually originate from maxillary teeth, either through maxillary sinusitis or, rarely, by direct invasion of the facial spaces. The spread of an odontogenic infection to orbital space can result in serious morbidity, such as visual loss, cavernous sinus thrombosis and death [2]. This case report serves as an example of how improper assessment of an infection’s route of spread could lead to delayed treatment and catastrophic results.
CASE PRESENTATION
A 67-year old patient was admitted to our Hospital with a complaint of swelling and pain in the right masticatory space, trismus and right eye proptosis with for the past month and a half . He had a history of poorly controlled type 2 diabetes mellitus for 20 years, arterial hypertension and coronary artery bypass graft surgery, all of which necessitated the use of glipizide, metformin, aspirin, carvedilol, atorvastatin and ramipril medications.
The patient reported undergoing a dental procedure due to a right-sided mandibular tooth infection. Two days later, the right masticatory space began to swell. A local doctor prescribed intramuscular Ceftriaxone 1-g injections twice a day for 20 days with no improvement. During a month, the swelling expanded to the right buccal, temporal and circumorbital spaces, and then exophthalmos in the right eye began to develop.
The patient was referred to the emergency room of a hospital in Damascus. The oral and maxillofacial team requested a panoramic dental X-ray (Fig. 1b). The patient was given Ceftriaxone, Carbapenem and Amikacin according to the outcome of the bacterial culture and antibiotic sensitivity test, which revealed Enterobacter. The pus was obtained by needle aspiration of the buccal space. To drain the abscess, an oral cavity’s right buccal and right temporal incisions were made, and a corrugated drain was inserted in both incisions. Despite treatment within a week, the swelling got worse and the right eye’s visual acuity started to deteriorate.
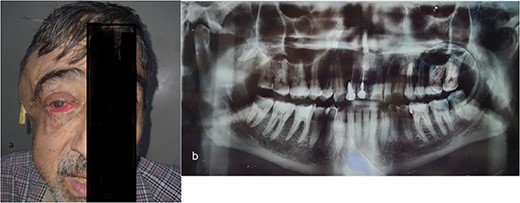
(a) The right masticatory, buccal and temporal regions are markedly swollen, and a drain has been inserted into the abscess cavity in temporal region. There is obvious pus oozing from the right eye, and the right eyelid and cornea both exhibit redness and edema. (b) Panoramic radiograph revealed periapical abscess, lateral large deep caries with pulp involvement in the third right mandibular molar tooth.
The patient was transferred to our hospital. The outside hospital had observed him after his initial procedure for a week before he came to our hospital.
At admission, 1 month and 1 week after initial symptom onset, the patient’s overall health was poor, with arterial hypotension, fatigue and fever. During the ophthalmic exam, the right eye showed exophthalmos, a purulent discharge from the lateral canthus, a visual acuity of 0/10 with only light perception, an upper corneal density with lateral thinning and herniation of the iris, with the contents of the uvea protruding through a corneal ulcer and upper eyelid ptosis (Fig. 1a).
The patient’s head and neck were imaged using magnetic resonance imaging (MRI) and computed tomography scan, which revealed the presence of abscess collections in the submasseteric space, pterygomandibular space, deep temporal space and infratemporal abscess spreading to the orbital cavity through a bony defect in the lateral orbital wall, all of which were not addressed during the first procedure (Figs 2 and 3).
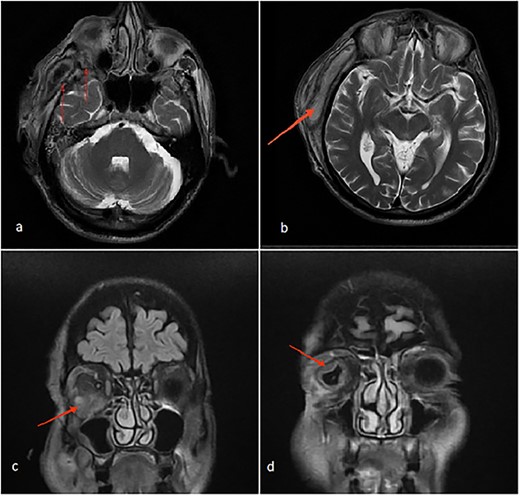
(a) Axial MRI of the head: a dumbbell-shaped lesion (red arrows) representing an infratemporal abscess invading the orbital cavity through the bony erosion of the lateral orbital wall. (b) Abscess localization in the deep temporal space (red arrows). (c, d) Coronal MRI of the head and neck shows an orbital abscess (red arrows) and endopthalmitis (red arrows).
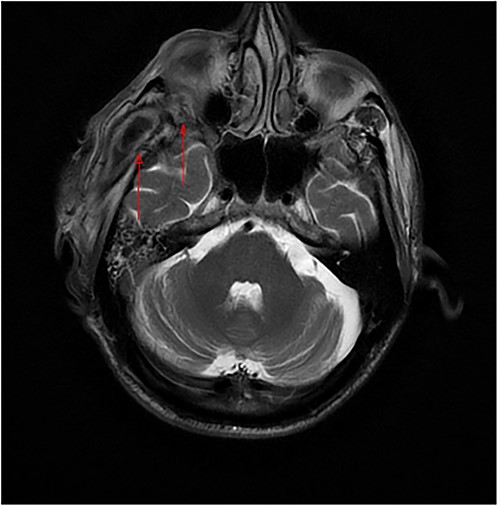
Axial MRI of the head, a dumbbell-shaped lesion (red arrows) representing an infratemporal abscess invading the orbital cavity through the bony erosion of the lateral orbital wall.
After admission, the patient received intravenous (IV) levofloxacin based on culture and sensitivity, and the ENT team performed a second surgical procedure to manage the undrained abscesses. Because to the patient’s unresponsive endophthalmitis, the ophthalmology team decided to drain the orbital abscess and perform evisceration. An implant was inserted into the evisceration cavity. The evisceration was performed out simultaneously with the second surgical procedure in ophthalmology. Surgery and antibiotic treatment were started immediately admission. The symptoms began to improve after 48 h, and within a week, the swelling and purulent oozing stopped, and the drains were removed. The edema was greatly lessened 2 weeks after admission, the CRP was steadily declining, and the patient was discharged.
DISCUSSION
The dual effects of diabetes mellitus and poor dental hygiene, both of which are underestimated issues in Arab regions, have been the reason for the aggressive course of our case [3].
Most cases of odontogenic orbital complications arise from upper jaw tooth infections [4]. What is unique about our case is the unusual route by which the infection spread into the orbit. In our case, the hypothesized path of spread started from the lower third molar infection to both the submasseteric and pterygomandibular spaces and then passed into the infratemporal fossa, where a focus of abscess was loculated, making its way into the orbit through a bony defect in the lateral orbital wall, forming an interesting dumbbell-shape appearance on MRI (Fig. 2a).
The need for a multidisciplinary approach should be emphasized in such cases, including the input of ENT, ophthalmology, internal medicine, radiology and microbiology.
We believe that one major reason for our patient’s symptomatology persistence was the insufficient surgical drainage, as demonstrated by MRI imaging, that revealed multiple abscess foci that were not addressed during the first surgery, which emphasizes the importance of clinical reassessment, repetition and expansion of imaging modalities when dealing with cases recalcitrant to conventional means of treatment.
MRI imaging has a superior role in the assessment of soft tissues, and that was clearly shown in our case as the MRI study helped track the route of infection [5]. The abscesses took place deep in the infratemporal fossa without obvious or specific clinical symptoms. Thus, imaging was the only way to detect the collections. In addition, persistence of inflammation-related clinical and lab markers (i.e. fever, malaise, and elevated ESR) suggests that the collections have probably been present all along the course but have not been managed.
CONCLUSION
Orbital complications of odontogenic infections, especially those of the lower jaw, are rare but may be serious and have severe consequences with delayed treatment, especially in immunocompromised patients. We stress the need for a multidisciplinary approach to treat such cases and the need for clinical and radiological reevaluation in cases refractory to treatment.
ACKNOWLEDGEMENTS
Dr Mohammad Kattaa, a resident in oral and maxillofacial surgery, is acknowledged for providing us with all the needed dental details and interpreting the dental panoramic radiograph.
We also acknowledge Dr Mohammad Jbawi and Dr. Obayda Rasheed Rabah, who work in the radiology department of Al-Mowasat University Hospital, for their assistance in reading and interpreting all of the radiological imaging.
GUARANTOR
Lava Abdullah.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The datasets used or analyzed in this study are available from the corresponding author on reasonable request.



