-
PDF
- Split View
-
Views
-
Cite
Cite
Shingo Kunioka, Takuya Watanabe, Hiroki Mochizuki, Takako Nakaya, Yumiko Hori, Eri Miyoshi, Nobuaki Konishi, Ayaka Arizono, Nana Kitahata, Tasuku Hada, Masaya Shimojima, Yasumasa Tsukamoto, Osamu Seguchi, Hiroyuki Kamiya, Kohei Tonai, Naoki Tadokoro, Satoshi Kainuma, Satsuki Fukushima, Tomoyuki Fujita, Norihide Fukushima, Efficacy of catheter cleaning methods using intravenous indwelling catheter, 10% silver nitrate solution and a monofilament nylon thread for deeply progressed superficial driveline infections: case series, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad443, https://doi.org/10.1093/jscr/rjad443
Close - Share Icon Share
Abstract
Driveline infection (DLI) is treated by local irrigation via driveline exit site (DLES) and surgical debridement is considered in patients with deep DLI. We describe three cases of deeply progressed superficial DLI that were considered to require surgical debridement but could be treated with a unique catheter cleaning method using intravenous indwelling catheter, a cotton swab with 10% silver nitrate solution and a monofilament nylon thread. Case 1 was a 60-y-old man with ischemic cardiomyopathy with left ventricular assist device implantation 2 y before. Daily bedside debridement with 10% silver nitrate solution was performed via the DLES. Case 2 was a 43-y-old man with ischemic cardiomyopathy who had recurrent DLI with methicillin-resistant Staphylococcus aureus, and case 3 was a 49-y-old woman with hypertrophic cardiomyopathy, who also showed improvement in their DLI with Pseudomonas aeruginosa. These cleaning methods may be useful for the deeply progressed superficial DLI.
INTRODUCTION
Implantable left ventricular assist devices (LVADs) play a critical role in the management of patients with advanced heart failure (HF) [1]. Driveline infection (DLI) is the most common LVAD-specific infection [2–5]. Superficial DLI is treated by local irrigation via driveline exit site (DLES). In contrast, surgical debridement or relocation of DLES is selected in patients with deep DLI. At what depth of superficial DLI can be safely treated with irrigation via DLES remains unclear [4–7].
Herein, we describe three cases of deeply progressed superficial DLI that were considered to require surgical debridement but could be treated with a unique catheter cleaning method using intravenous indwelling catheter, a cotton swab with 10% silver nitrate solution and a monofilament nylon thread.
CASE SERIES
Figure 1 illustrates the concept of the catheter cleaning method via the DLES used in this case series. First, the intravenous indwelling catheter is deeply inserted via the DLES to clean the space around driveline. Then, a cotton swab with 10% silver nitrate solution is used to eliminate infected and contaminated tissues. As adequate removal of the infected tissue is crucial, daily elimination of infected tissue using this procedure is generally continued for 1 week. If the depth of infection space around the driveline is deep and continuous drainage is inadequate, monofilament nylon threads are inserted for continuous drainage of exudate via capillary action. Figure 2 shows how the depth of DLI is assessed and how this procedure is performed in practice. Figure 2a reveals the finding of gallium-67 single-photon emission computed tomography (67Ga SPECT), with a high signal, suggesting that the inflammatory area is inside the DLES. Figure 2a, c present findings of superficial echography examination where hypoechoic areas indicate a space around the driveline; this is the suspected infected area. This procedure is deemed feasible as long as the infected space was within reach of the cotton swab and intravenous catheter from DLES. Figure 2d, e show a cleaning method using an intravenous catheter via the DLES. Similarly, a cotton swab with 10% silver nitrate solution is inserted via the DLES to eliminate infected and contaminated tissues. Monofilament nylon threads are inserted for continuous drainage (Fig. 2f–h).
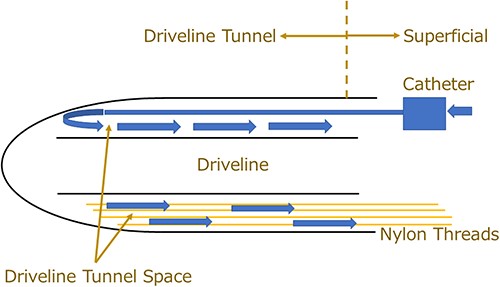
Management concepts and schema of the catheter method via the DLES. A deeply progressed superficial DLI is defined as an infection that has extended from the superficial region of the exit site to the deeper portion but has not reached the pump pocket. An intravenous indwelling catheter can flush the driveline tunnel space from the far end of the space. Notably, excessive injection pressure should be avoided when injecting the cleaning solution into the driveline tunnel space to prevent contaminated fluid from entering the deep part of the space. A cotton swab with 10% silver nitrate solution is used to eliminate infected and contaminated tissues or to enlarge the confined space. Nylon threads help with the continuous drainage, utilizing a capillary action despite the narrow space.
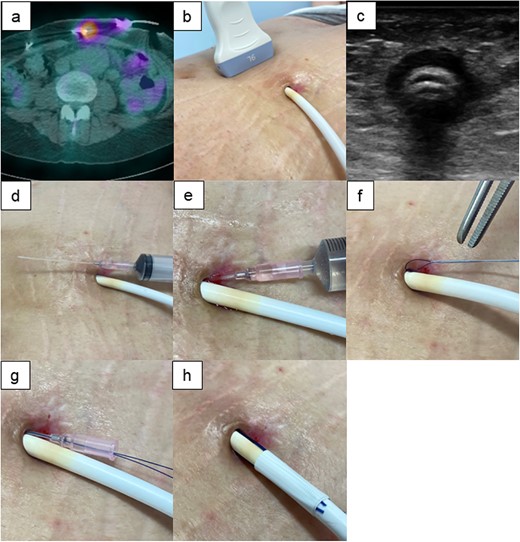
Evaluation of the depth of DLI. (a) Gallium-67 single-photon emission computed tomography (67Ga SPECT) shows the extent of high signalization from the DLES. (b,c) Body surface echography findings show hypoechoic area around the driveline, suggesting effusion of poorly organized inflammatory fluid from the DLES. (d–f) Cleaning of the driveline tunnel using an intravenous indwelling catheter. The catheter is about 5-cm long; it can be cleaned if the length of the infective driveline tunnel is within reach of the cotton swab and intravenous catheter from DLES. (g, h) The intravenous indwelling catheter may be also useful when the nylon threads are inserted into the driveline tunnel space. A catheter and nylon threads are inserted in the driveline tunnel space. Then, the catheter is removed while leaving the nylon threads. SPECT: single-photon emission computed tomography.
Case 1
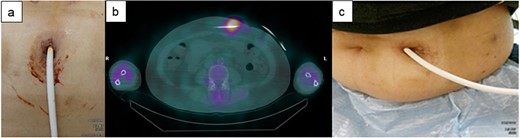
A 60-y-old man with ischemic cardiomyopathy underwent LVAD implantation (HeartMate II™, Abbott Co., Abbott Park, IL, USA) 2 y before being admitted to our hospital because of pain and skin redness above the umbilicus. He had no skin induration and tenderness at the DLES; however, redness, local increase in temperature, and skin induration and tenderness were noted above the umbilicus (Fig. 3a). As the inflammatory area was far from the DLES, surgical debridement and associated relocation of the exit site were considered. 67Ga SPECT showed a high signal up to 5 cm inside the DLES (Fig. 3b). The empirical antibiotics were administered intravenously after collection of cultures of exit site and drained fluid. First, the catheter cleaning method via the DLES was executed, daily bedside debridement with 10% silver nitrate solution was performed via the DLES to eliminate the contaminated tissue for about 1 week. In this patient, the DLES and spot with redness were distant, and it was suspected that the infected granulation tissue affected the discharge of the exuded solution. Therefore, monofilament nylon threads were inserted for continuous drainage (Fig. 3a). Simultaneously, daily irrigation using an intravenous indwelling catheter was continued with a 1000-ml saline solution for about 1.5 months (Fig. 2e). Although repeated culture of drained fluid did not detect the definitive pathogenic bacterium, intravenous antibiotics were used for about 6 weeks but were then switched to oral antibiotics. The spot with redness healed, and the patient was discharged from the hospital 2 months after admission (Fig. 3c). This patient was readmitted for a similar DLI 4 months later and was treated with the same catheter method for about 3 weeks. Then, DLI did not reoccur until 1.5 y later.
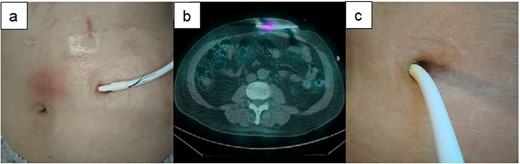
The clinical course of development of the DLI in Case 1. (a) There was some distance between the DLES and the spot with redness and induration. (b) 67Ga SPECT shows high signalization within reach of the cotton swab and intravenous catheter from DLES. (c) The spot with redness and induration healed after treatment with this catheter method.
Case 2
A 43-y-old man with ischemic cardiomyopathy underwent LVAD implantation (HeartMate II™, Abbott Co., Abbott Park, IL, USA) and was readmitted to our hospital because of DLI 3.5 y after this implantation. The DLES had erythema and induration with purulent discharge (Fig. 4a). Culture of the DLES had previously shown the presence of methicillin-resistant Staphylococcus aureus (MRSA). The patient was admitted to our hospital for surgical relocation of the DLES for deep DLI. However, as 67Ga SPECT showed an inflammation area localized 5 cm around the DLES (Fig. 4b), the catheter cleaning method was firstly selected prior to a surgical approach. Appropriate intravenous antibiotic therapy was administered for about 6 weeks, and debridement and cleaning of the infected area via the DLES were performed daily for about 2 months. The catheter cleaning method via the DLES was effective for his DLI; the local increase in temperature gradually improved, and exudation decreased (Fig. 4c). The patient was discharged on day 66 after hospitalization. Oral antibiotic therapy was continued after discharge and was completed after approximately 3 months. DLI has not reoccurred in the 6 months after discharge.
The clinical course of recurrence of the DLI in Case 2. (a) The DLES had erythema and induration. (b) 67Ga SPECT showed an inflammation area localized to 5 cm around the DLES. (c) Purulent discharge was decreased, and the space around the driveline was reduced.
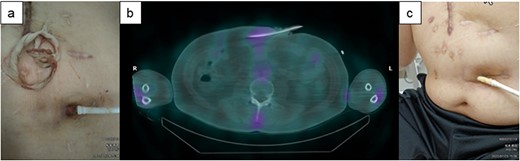
Case 3
A 49-y-old woman with hypertrophic cardiomyopathy underwent LVAD implantation (HeartMate II™, Abbott Co., Abbott Park, IL, USA) and was readmitted to our institution for DLI 4.5 y after this implantation. Skin induration, tenderness along the driveline tunnel, and bleeding and purulent discharge from the driveline tunnel space were found; furthermore, the culture from driveline drainage showed Pseudomonas aeruginosa (Fig. 5a). Although surgical relocation of the DLES was considered, 67Ga SPECT showed a high signal up to 5 cm inside the DLES (Fig. 5b), and the range of cutaneous infection was limited to 5 cm from the site. Therefore, the catheter cleaning method paired with intravenous antibiotics was selected. Consequently, the exuded solution became clear, and the amount gradually decreased. The patient’s DLI gradually improved (Fig. 5c), and she was discharged from our hospital on day 57 after hospitalization.
The clinical course of development of the DLI in Case 3. (a) Skin induration and tenderness along the driveline tunnel and bleeding and purulent discharge from the driveline tunnel space were found. (b) 67Ga SPECT suggested a high signal up to 5 cm inside the DLES. (c) The exuded solution became clear, and the amount gradually decreased. The patient’s DLI gradually improved.
DISCUSSION
Management of DLI that develop at deep within the DLES remains challenging. In general, healing of wound infections requires adequate cleaning and debridement of contaminated tissue to reduce the localized bacterial infection. Our case series suggests that the catheter cleaning method via the DLES using silver nitrate solution and nylon thread drainage was effective for the debridement of infected tissue, even for deeper superficial DLI which may be indicated for surgical debridement. Evaluation of the extent of the infected area using SPECT or superficial echography plays a key role in patient selection for this therapeutic strategy.
Although the importance of debridement and drainage of infected wounds is widely recognized, how these procedures are performed in patients with deeply progressed DLI remains controversial. When DLIs reach deeper, inflammatory exudates and abscesses are observed adjacent to the driveline [5], for which continuous drainage is essential. As reported in the field of plastic surgery, a 10% silver nitrate solution may be an effective tool for the debridement of infected granulation tissue; this is already used in plastic surgery owing to its low invasiveness and availability [8]. Furthermore, nylon thread drainage can drain the collected fluid, is easy to use, has no adhesiveness and is easy to remove [9]. Because the DL tunnel space is narrow and limited, these threads are useful for securing continuous drainage during DLI management.
Surgical treatment, including relocation of the DLES, is an effective treatment procedure; however, its efficacy and procedures have not been properly established in patients with deeply progressed superficial DLI despite its high invasiveness [5, 6]. Furthermore, relocation of the DLES following surgical debridement shortens the tissue barrier that can prevent the extension of the infection area, which may result in a shorter time to pump exchange in event of DLI recurrence. Moreover, patients need to learn a different wound self-care dressing procedure tailored to relocated DLES. This catheter cleaning method allows for the treatment of deeper superficial DLI without replacement of the DLES.
Whether this cleaning method is effective for all of DLI patients, even if the range of infection is narrow from the DLES, remains unclear. Future prospective randomized controlled studies are required to evaluate the usefulness of this procedure for DLI. Careful selection of patients indicated for this procedure is crucial.
In conclusion, a catheter cleaning method via DLES using an intravenous indwelling catheter, a cotton swab with 10% silver nitrate solution, and 2–0 monofilament nylon threads may be an effective therapeutic option for the deeper superficial DLI.
INSTITUTIONAL REVIEW BOARD
This case report was approved by the local ethics committee in National Cerebral and Cardiovascular Center. Appropriate informed consent was obtained from those patients (National Cerebral and Cardiovascular Center IRB number M30-026).
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
T.W. was supported by a Japan Heart Foundation Research Grant, MEXT/JSPS KAKENHI Grant-in-Aid for Young Scientists (B) 15K21697, 19K09256 and 23K07519.
DATA AVAILABILITY
The deidentified participant data will not be shared.



