-
PDF
- Split View
-
Views
-
Cite
Cite
Courtney Holinger, Magdalena Sejka, Adam Skidmore, Case report: doing the mesenteric twist, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad221, https://doi.org/10.1093/jscr/rjad221
Close - Share Icon Share
Abstract
A 23 year old female presents with an internal hernia after undergoing a laparoscopic duodenojejunostomy for superior mesenteric artery syndrome. This is an extremely uncommon complication. On review of the literature and this case, it is hypothesized that the internal hernia happened in this case due to the longer than usual distance between the duodenojejunal flexure and the part of jejunum brought up to anastomosis.
INTRODUCTION
Superior mesenteric artery (SMA) is a rare, not yet fully understood condition that causes duodenal obstruction. A multitude of conditions that cause rapid weight loss are thought to result in the loss of the fat pad between the aorta and the SMA. This causes the SMA to apply extrinsic pressure on the duodenum causing obstruction.
The main treatment methods are medical and involved nutrition and reversing the causes of the weight loss. When these methods do not relieve the symptoms, surgery to perform a duodenojejunostomy is the next step to consider [1]. This case study explores how a rare complication of this surgery, an internal hernia, may have occurred.
CASE STUDY
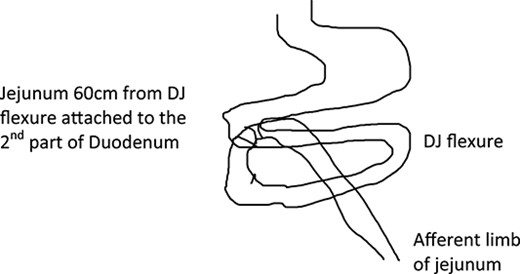
A 23 year old female underwent a laparoscopic duodenojejunostomy for SMA syndrome. The duodenum was accessed infra-colic and the second part of the duodenum was anastomosed to the proximal jejunum 60 cm from the duodenojejunal (DJ) flexure (Fig. 1).
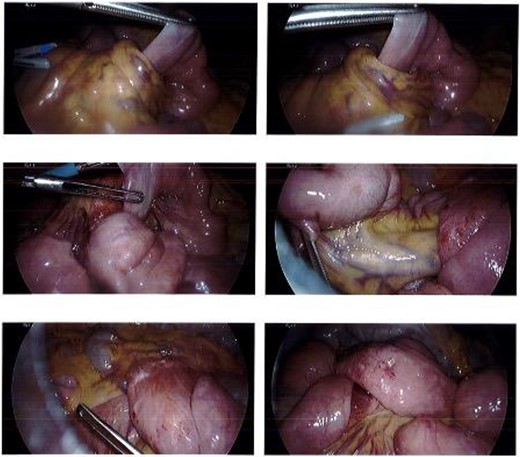
She presented to the surgeon’s rooms with a history of 9 days of postprandial vomiting 9 months later. A computed tomography (CT) showed a volvulus immediately adjacent to the duodenojejunostomy anastomosis causing a small bowel obstruction (Fig. 2).

The patient was taken for a diagnostic laparoscopy and found to have an internal hernia. Small bowel had fallen through a defect between the afferent limb of the jejunum and the third part of the duodenum (Fig. 3). This was reduced, the small bowel was run and found to be viable with no need for resection. The defect was closed with 3.0 V-lock suture.
The patent recovered well from the surgery and discharged Day 9 post operation.
DISCUSSION
SMA syndrome is a rare condition that causes obstruction of the third part of the duodenum due to extrinsic compression from the SMA. The primary cause is thought to be due to loss of the mesenteric fat pad between the SMA and aorta. The adult cohort of patients at risk of SMA syndrome are those who have underwent significant weight loss either deliberately or due to medical or psychological disorders [2]. The first line of treatment is conservative and focuses on enlarging the narrow aorto-mesenteric angle via nutritional optimization, if this fails the main surgical treatment of SMA syndrome is duodenojejunostomy [3].
A duodenojejunostomy involves creating an anastomosis between the duodenum and the jejunum [4]. A review of what literature is available on duodenojejunostomy for SMA syndrome reports that most surgeon’s anastomosis the jejunum 20–30 cm from the DJ flexure [5]. Internal hernias are a very rare complication of a duodenojejunostomy and there is no literature on this phenomenon. This patient’s anastomosis occurred at 60 cm from the DJ flexure, which may have created a bigger defect and therefore made this patient more prone to an internal hernia.
The take away message from this case it to ensure that the anastomosis point of the jejunum is a short enough distance from the DJ flexure that a defect, through which small bowel can fall, is not created and therefore lead to an internal hernia.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



