-
PDF
- Split View
-
Views
-
Cite
Cite
Shota Morimoto, Tomoya Iseki, Toshiya Tachibana, Hiroyuki Futani, Bacillus Calmette–Guérin osteomyelitis of the fifth metatarsal bone in a Japanese infant: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad362, https://doi.org/10.1093/jscr/rjad362
Close - Share Icon Share
Abstract
Bacillus Calmette–Guérin osteomyelitis is a rare complication following Bacillus Calmette–Guérin vaccination. Here, we describe a rare case of Bacillus Calmette–Guérin osteomyelitis of the fifth metatarsal in a 21-month-old Japanese infant. A 21-month-old Japanese female infant presented with a swollen mass on the dorsolateral aspect of the left foot. Based on physical examination, radiological and histopathologic findings and laboratory results, a diagnosis of Bacillus Calmette–Guérin osteomyelitis of the fifth metatarsal bone was made, and an oral anti-tuberculosis treatment was initiated. However, the mass recurred 10 months after the start of the anti-tuberculosis treatment, so additional surgical debridement was performed. Six months after surgery, clinical findings and plain radiograph images revealed complete improvement of the affected area, and anti-tuberculosis treatment was stopped. Bacillus Calmette–Guérin osteomyelitis of the fifth metatarsal in a 21-month-old Japanese infant was successfully treated with oral anti-tuberculosis therapy and surgical debridement.
INTRODUCTION
Tuberculosis (TB) is an airborne infectious disease caused by Mycobacterium tuberculosis, which affects ~10 million people worldwide and kills 1–3 million people annually [1, 2]. The Bacillus Calmette–Guérin (BCG) vaccine, discovered by Calmette and Guérin and now widely used to prevent the onset of TB, is derived from live attenuated Mycobacterium bovis [3]. In particular, since TB morbidity and mortality are higher in children under 5 years of age, and so >90% of newborns receive the BCG vaccine to prevent active TB [2, 4].
Complications associated with the BCG vaccine are relatively rare, accounting for 3.3% of cases after BCG vaccination [5]. The most common complication is subcutaneous abscess, followed by local purulent lymphadenopathy [6]. Osteomyelitis is a rare complication, with a reported prevalence of ~0.01 to 1.1 per million cases [7–9]. Previous reports have shown that BCG osteomyelitis occurs most frequently in the epiphysis or metaphysis of long tubular bones a few months to years after vaccination [10, 11]. However, there are no reports of BCG osteomyelitis having developed in the fifth metatarsal.
This report describes a rare case of BCG osteomyelitis of the fifth metatarsal bone in a 21-month-old Japanese infant. Written informed consent was obtained from the patient’s family for the publication of this report.
CASE REPORT
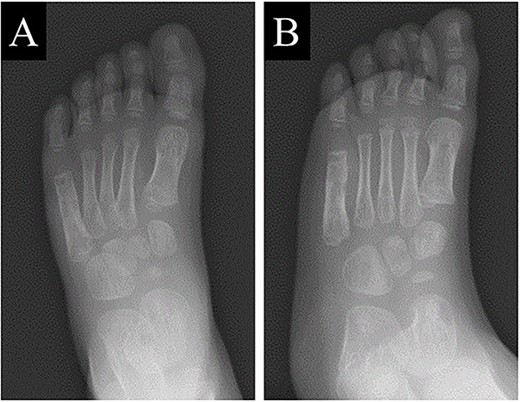
A 21-month-old Japanese female infant presented with a swollen mass on the dorsolateral aspect of the left foot. Her parents noticed the mass and brought the patient to our hospital. The patient had no past medical histories or complications prior to the occurrence. In addition, she received the BCG vaccine at the age of 4 months in Japan. At first visit to our hospital, physical examination revealed the ~3 × 3 cm mass was located on the dorsolateral aspect of the left foot and was hard accompanied by local heat (Fig. 1). Plain radiographs of the left foot showed a lytic lesion without periosteal reaction in the fifth metatarsal bone (Fig. 2). Magnetic resonance imaging (MRI) showed an isointense lesion on T1-weighted images and a hyperintense lesion on T2-weighted images around and within fifth metatarsal (Fig. 3). Gallium scintigraphy revealed intense uptake in the patient’s left foot (Fig. 4). In addition, laboratory examination was within normal. Based on medical history, clinical and imaging findings, we considered the possibility of neoplasia or osteomyelitis and performed an open debridement and biopsy of the lesion to make a diagnosis. The lesion was yellow and consisted of weak, adipose-like tissue that surrounded and continued into the inferior of the fifth metatarsal bone (Fig. 5). The lesion inside and outside the bone was resected as much as possible. Histopathologic examination of the lesion showed granulomatous inflammation including anaplastic giant cells, Langerhans-type giant cells and caseous necrosis (Fig. 6). Based on these results, TB or BCG osteomyelitis was considered as a diagnosis. The tuberculin test was positive, but the QuantiFERON TB test was negative. In addition, samples analyzed using polymerase chain reaction did not identify M. tuberculosis, but did identify the BCG Tokyo-172 strain. Per these findings, the patient was diagnosed with BCG osteomyelitis of the fifth metatarsal and oral treatment with anti-TB medicine including isoniazid (100 mg/day) and rifampicin (150 mg/day) was started. Clinical findings included reduction in swelling of the mass and gradual remodeling of the lytic lesion of the fifth metatarsal on plain radiographs (Fig. 7). However, 10 months after starting the anti-TB treatment, the mass recurred, and MRI revealed a residual high-intensity lesion around and inside the fifth metatarsal on T2-weighted fat-suppressed images (Fig. 8). It was determined that the lesion was difficult to control with anti-TB treatment alone, so an open debridement for the lesion was performed again. Histopathologic examination of the lesion revealed an epithelioid granuloma with necrosis. Therefore, the anti-TB treatment was continued. Six months after the second surgery, clinical and radiographic image findings showed complete improvement (Fig. 9). As a result, anti-TB treatment was ended. At the time of writing this report, 8 years after starting anti-TB treatment, there has been no recurrence.

The mass, ~3 × 3 cm, was located on the dorsolateral aspect of the left foot and was hard accompanied by local heat.
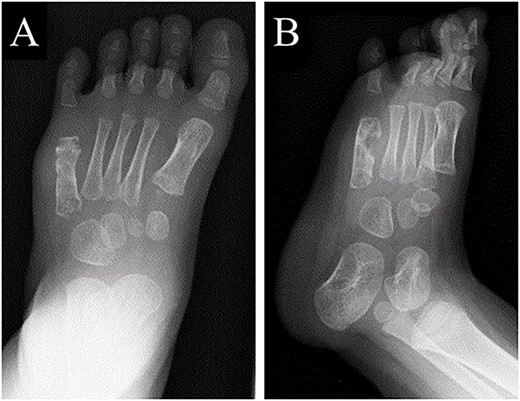
Plain radiographs of the left foot showing a lytic lesion without periosteal reaction in the fifth metatarsal bone in (A) anteroposterior and (B) oblique views.
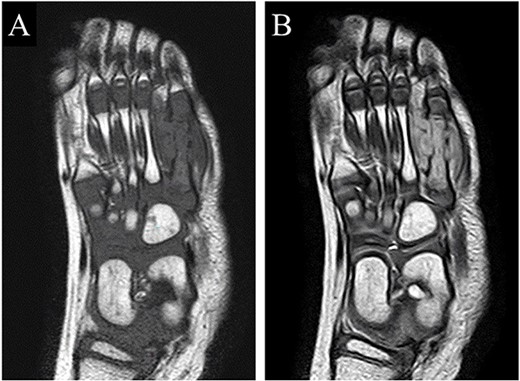
MRI showed an isointense lesion on T1-weighted images and a hyperintense lesion on T2-weighted images around and within the fifth metatarsal.
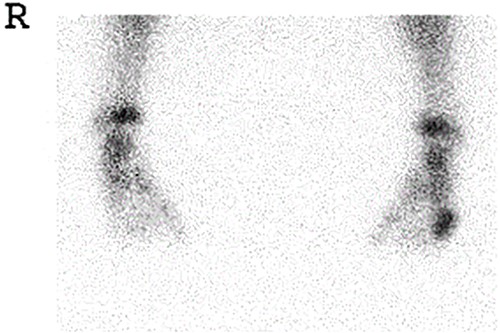
Gallium scintigraphy revealed intense uptake in the patient’s left foot.
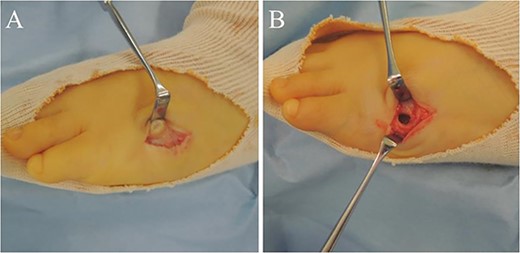
(A) The lesion was yellow and consisted of weak, adipose-like tissue that surrounded and continued into the inferior of the fifth metatarsal bone; (B) The lesion inside and outside the bone was resected as much as possible.
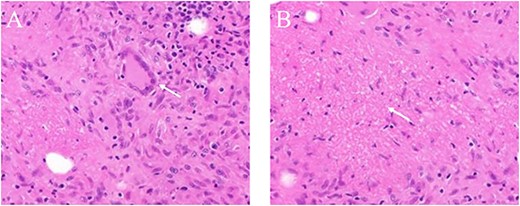
The histopathologic examination of the lesion showed granulomatous inflammation including anaplastic giant cells; (A) Langerhans-type giant cells (white arrow) and (B) Caseous necrosis (white arrow).
Plain radiographs of the left foot showed the lytic lesion of the fifth metatarsal was remodeled gradually in (A) anteroposterior and (B) oblique views.

MRI revealed that a high-intensity lesion remained around and inside the fifth metatarsal on T2-weighted fat-suppressed images.
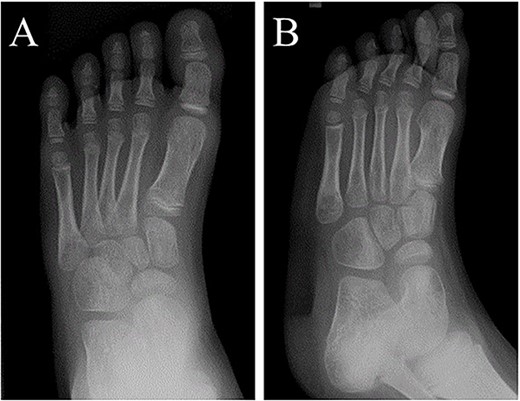
At 6 months after the second surgery, image findings on plain radiographs completely improved on (A) anteroposterior and (B) oblique views.
DISCUSSION
Japan is a moderately endemic country for TB with a TB notification rate of 13.3 per 100 000 people in 2017 [12]. Therefore, in Japan, it is recommended to administer the BCG vaccine (particularly for the BCG Tokyo-172 strain) to infants aged 5 to 8 months due to its high efficiency in preventing the development of TB and low complication rate [13].
BCG osteomyelitis is a rare complication that often occurs a few months to years after BCG vaccination [14]. The incidence rate of BCG osteomyelitis is reported to be 1.1 per million cases in Europe, but 0.01 per million cases in Japan [7–9]. Yamamoto et al. [15] reported that a variety of factors are associated with this difference in incidence, including route of administration, vaccine strain, dosage, timing of vaccination, patient’s immune status and surveillance strategy. Osteomyelitis is also reported to t occur more frequently in the epiphysis or metaphysis of long, tubular bones, and sometimes in flat bones such as the vertebrae and sternum [10, 11].
Although there is no clear consensus on the treatment of BCG osteomyelitis, oral anti-TB treatment alone or in combination with surgical debridement is generally recommended [10]. A two-drug or three-drug regimen (isoniazid plus rifampicin with or without pyrazinamide) is commonly used as oral anti-TB treatment [14]. Although the optimal duration of anti-TB treatment has not yet been established, it has been reported that most cases of BCG osteomyelitis are cured within 6 months to 1 year [14]. No clear indication for surgical debridement has been determined [14].
In conclusion, a rare case of fifth metatarsal BCG osteomyelitis of the fifth metatarsal bone in a 21-month-old Japanese infant was successfully treated with combination oral anti-TB therapy and surgical debridement.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
FUNDING
No funding.
DATA AVAILABILITY
Not applicable.



