-
PDF
- Split View
-
Views
-
Cite
Cite
David Z Allen, Emily M Cao, Gabriela Cruz, Joshua J Kain, Use of an open partial laryngectomy technique for a massive laryngeal leiomyosarcoma in a 40-year-old man with functional preservation postoperatively, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad370, https://doi.org/10.1093/jscr/rjad370
Close - Share Icon Share
Abstract
Laryngeal cancers are one of the most common head and neck malignancies and can lead to significant morbidity and mortality. Although they most commonly originate from squamous cell carcinoma, there are multiple different pathologies that can arise. We present a patient with an atypical presentation of a glottic mass for which final pathology revealed a leiomyosarcoma (LMS). We report the first case in the English literature of a large bulky LMS that was removed entirely through a partial vertical laryngectomy and pharyngectomy, with maintained swallow and speech function postoperatively.
INTRODUCTION
Leiomyosarcomas (LMS) are a rare cause of glottic cancer, making up <1% of all laryngeal neoplasms [1–4]. A LMS is made up of either smooth muscle or aberrant undifferentiated mesenchymal tissue and often presents in a nearly identical manner as laryngeal squamous cell carcinoma [1–4]. Symptoms are typically nonspecific and non-unique to its diagnosis including dysphagia, dyspnea, progressive hoarseness and infrequently stridor or choking sensation [1–4]. Furthermore, initial biopsies can mistake this cancer for a spindle cell carcinoma, making the definitive diagnosis dependent on immunohistochemical analysis with the adjunctive use of electron microscopy. Broad population risk factors have been difficult to characterize, and there is a paucity of research into head and neck LMS. Treatment commonly entails an aggressive surgical approach, frequently by a total laryngectomy with adjunctive radiotherapy for bulky tumors and long-term follow-up. However, this approach leaves the patient with life-long debilitation in swallow and speech function even with proper rehabilitation. Open partial laryngectomy surgery (OPL) has a long and successful history in head and neck surgical oncology dating back to as early as 1947 [5]. However, with the subsequent adoption and expansion in the use of transoral laser microsurgery and later transoral robotic surgery for laryngeal and hypopharyngeal pathologies, these open operative techniques have become scarce to non-existent in modern head and neck training. We present the first patient in the English literature with a bulky LMS successfully excised with a partial vertical laryngectomy to highlight the utility of OPL in the modern era of head and neck surgery.
CASE REPORT
A 40-year-old male with a hypopharyngeal mass was referred to a tertiary head and neck surgical oncology practice after a computerized tomography (CT) scan showed a large 6.5 cm heterogeneously enhancing mass involving the right larynx and hypopharynx, as well as the right thyroid cartilage with local mass effect without separate regional adenopathy (Fig. 1).
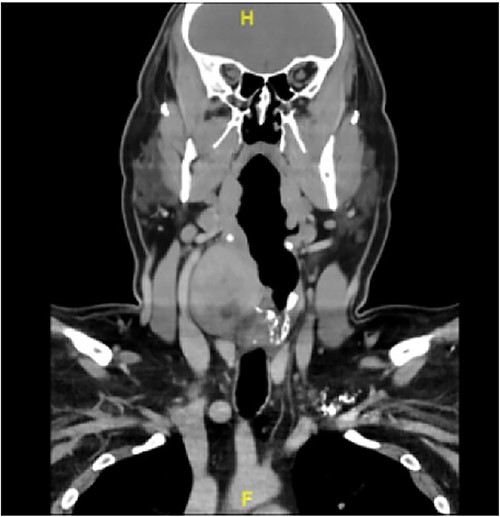
CT scan illustrating the large 6.5 cm mass involving the right larynx and hypopharynx.
This patient’s presenting symptoms were a non-tender, palpable enlarging right-sided neck mass, sleep-disordered breathing and minimal regurgitation when eating without any solid or liquid dysphagia. In the office, a flexible laryngoscopy showed a right-sided lateral hypopharyngeal mass with leftward laryngeal deviation and rotation that was entirely submucosal. The clinical boundaries included the ipsilateral supraglottic soft tissues, the thyroid cartilage ala, the lateral arytenoid and the entirety of the right piriform sinus, which was submucosally obliterated by the mass. There was also diminished mobility of the right vocal fold, predominantly affecting lateral excursion. An ultrasound-guided core-needle biopsy of the mass was performed in-office, and the pathology showed an atypical spindle cell proliferation in sclerotic stroma with smooth muscle differentiation, without clear malignant features. Subsequently, an operative direct laryngoscopy with endoscopic tissues sampling of the right hypopharyngeal submucosal mass was performed. This pathology too returned indeterminate as a spindle cell neoplasm with smooth muscle differentiation despite extensive immunohistochemical studies and analysis.
The decision was then made to pursue definitive surgical management. The patient underwent an awake fiberoptic intubation, direct laryngoscopy, open partial right vertical laryngectomy, open right lateral pharyngectomy, right neck dissection levels II–IV and tracheostomy with preservation of the ipsilateral recurrent laryngeal nerve. Importantly, the intrinsic laryngeal musculature stimulated robustly to 1.0 mA intraoperative electric stimulation after tumor resection showing intact conduction. The ipsilateral right posterior cricoarytenoid muscle fibers were sacrificed with the medial aspect of the tumor. He was able to achieve primary tension-free mucosal closure of the oncologic lateral pharyngotomy defect with no leak by postoperative water-soluble esophagram on postoperative day 7. He was phonating with intelligible speech by cannula finger occlusion and was decannulated from tracheostomy placement on postoperative day 7. He achieved an oral diet by postoperative day 14 and advanced to a solid diet by 4 weeks without the need for non-oral supplementation. By 6 weeks postoperative, he was tolerating a complete solid and liquid diet without restrictions and was phonating with fully intelligible speech, both personally and professionally. Three-month post-treatment imaging showed no evidence of recurrence, and flexible laryngoscopic examination shows full and complete right vocal fold adduction with complete glottic closure with partial limitation in lateral excursion.
Final pathology revealed a moderately differentiated LMS (grade 2/3) with clear surgical margins and without lymphovascular invasion or perineural invasion (Figs 2 and 3). None of the 32 lymph nodes collected were positive for malignancy. With a grade 2 histology, he was recommended postoperative dosed radiation (60 Gy in 30 fractions) for enhanced durable locoregional control.
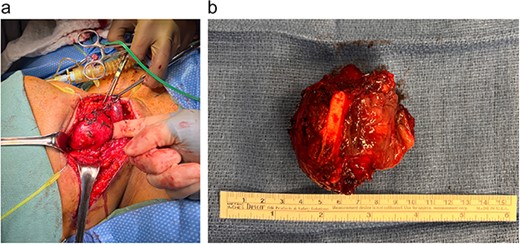
Gross images of the LMS in the operating room (a) and post-excision with clear illustration of the involvement of the thyroid cartilage (b).
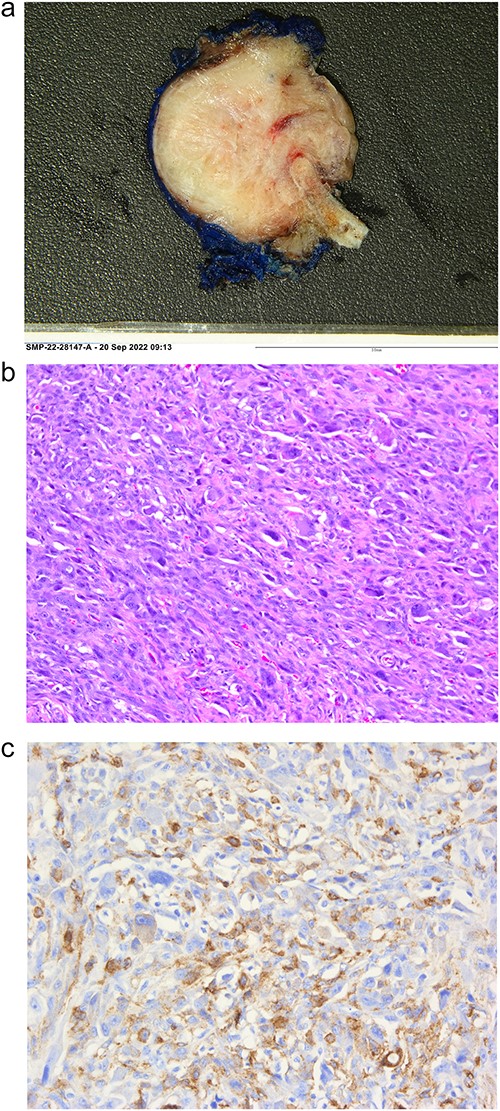
Histopathological analysis of the LMS including the gross image (a), hematoxylin and eosin staining (b), alpha smooth muscle actin immunohistochemical staining (c).
DISCUSSION
Laryngeal carcinomas make up around one-third of all head and neck cancers each year and are a significant reason for morbidity and mortality, with a 5-year survival rate of around 60% based on Surveillance, Epidemiology, and End Results 2009–15 results [6]. LMS, which are soft-tissue tumors arising from smooth muscle fibers or undifferentiated mesenchymal cells, appear to be most prevalent in areas of smooth muscle such as the uterus, retroperitoneum and gastrointestinal system [7]. Only 3% of cases arise in the head and neck region, with most documented cases involving the oral cavity [8]. The first case of laryngeal leiomyosarcoma found in medical literature was reported by Jackson et al. in 1923 and since then, to the best of our knowledge, <60 total cases in the English literature have been published [9].
The etiological factors for head and neck sarcomas remain ill-defined. Patients with a history of radiation exposure, surgery and immunosuppression status linked to Epstein–Barr virus are thought to be predisposed, and certain hereditary conditions including von Recklinghausen’s disease, Werner syndrome, Turcot syndrome, tuberous sclerosis, along with various other syndromes are believed to carry higher incidence of sarcomas in general. A significant percentage of reported cases have indicated a male-gender predilection with a ratio of 4:1 [10].
Commonly reported symptoms are nonspecific but include dysphagia, dyspnea and progressive hoarseness and possibly stridor or respiratory distress that necessitated a surgical airway [2, 8]. Furthermore, the definitive diagnosis of this pathology is difficult, as its clinical presentation is indistinguishable with that of carcinomas. This renders immunohistochemical assessment with the adjunctive use of electron microscopy for ultrastructural examination central to its accurate diagnosis [2]. In fact, for this patient, an office-based ultrasound-guided core-needle biopsy and an operative direct laryngoscopy with biopsy did not elicit a definitive histopathological diagnosis, despite abundant tissue for analysis.
Histologically, LMS are characterized by bundles and fascicles of spindle cell proliferation, along with cigar-shaped nuclei, eosinophilic cytoplasm and prominent nucleoli [11]. Varying levels of pleomorphism and increased mitotic rates can be observed in some forms of LMS. Immunohistochemical analysis is used to differentiate a LMS from other spindle cell tumors, such as spindle cell carcinoma, melanoma and rhabdomyosarcoma.
In most reported cases of bulky LMS of the larynx, a total laryngectomy was chosen for complete removal of the disease, resulting in the patient being stomal dependent and experiencing difficulties with both swallowing and speech, leading to a lower quality of life [3, 12]. This case is novel by being the first reported patient in the English language literature to have a bulky LMS removed entirely through a partial vertical laryngectomy and partial pharyngectomy, while preserving the neural integrity and intrinsic muscle targets of the recurrent laryngeal nerve. Furthermore, our patient regained normal speech and swallowing function allowing him to return to a near-baseline level of function after major oncologic head and neck surgery.
CONCLUSION
Herein, we present the first patient with a bulky laryngeal LMS that was completely excised through a partial vertical laryngectomy and partial pharyngectomy, maintaining complete phonation and swallowing function.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
All data underlying the results are available as part of the article and no additional source data are required.



