-
PDF
- Split View
-
Views
-
Cite
Cite
William Sergi, Stefano D’Ugo, Annarita Libia, Norma Depalma, Tiziana Marchese, Stefano Garritano, Stefania Vadrucci, Elisa Stasi, Ivan Botrugno, Farshad Manoochehri, Marcello Spampinato, William Sergi, Symptomatic acinar cell cystadenoma of the pancreas, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad360, https://doi.org/10.1093/jscr/rjad360
Close - Share Icon Share
Abstract
Acinar cystic transformation (ACT), also known as ‘acinar cell cystadenoma’, is an uncommon cystic neoplasm of pancreas with unknown malignant potential. This case regards a woman with symptomatic pancreatic head ACT, revealed with pathological exam of specimen after pancreaticoduodenectomy. A 57-years-old patient presented mild hyperbilirubinemia and recurrent cholangitis; she underwent to ERCP, EUS and MRI, and these exams revealed a large cyst of the pancreatic head that caused biliary compression. The discussion of the case by the multidisciplinary group indicated surgical resection. Pancreatic ACT is so rare, and its preoperative diagnosis is difficult. The symptoms of the patients and the features of the cyst are the criteria to choose a surgical resection.
INTRODUCTION
Acinar cystic transformation (ACT) of the pancreas is a benign lesion, particularly rare to be diagnosed. It was first described as an incidental autopsy finding in a case report from 2002 and defined ‘acinar cystadenoma’. Since then, several case reports have been published discussing possible etiologies of this previously unrecognized neoplasm [2].
Literature reported a total of about 75 patients with ACT of the pancreas; because of the poor number of reported cases, epidemiology and pathogenesis of this neoplasm are still unclear. Last evidence suggest that it could be a nonneoplastic dilation of the acinar and ductal epithelium [3], so the 2019 5th edition of the WHO classification reclassifies it as a nonneoplastic cystic lesion [4].
This rare type of pancreatic cystic lesion represents a diagnostic challenge, being a benign lesion in differential diagnosis with other pancreatic cysts harboring malignant potential, such as intraductal papillary mucinous neoplasm (IPMN) or mucinous cystic neoplasm. It is important to establish a correct diagnosis, considering that clinical management and follow-up are different among the various cystic lesions. We herein report a case of symptomatic ACT treated with surgical resection.
CASE PRESENTATION
A 57-year-old female patient presented to our department with mild direct hyperbilirubinemia and recurrent episodes of cholangitis. On her past medical history, she had hypertension and previous laparoscopic cholecystectomy. Before admission, she underwent an US scan first, with evidence of small stones in the common bile duct. She was hence booked for an elective ERCP. The exam showed, besides the stones, a stenosis of the distal bile duct, which was likely compressed from a cystic lesion of pancreatic head: endoscopist proceeded with the remotion of the stones and the placement of a plastic stent in the common bile duct.
Measurement of the oncomarkers showed a CA 19.9 value of 343 U/ml (normal < 40). Following the ERCP, the patient was submitted to further investigations with MRI and EUS. The MRI with cholangiographic sequences revealed a cystic cluster, with maximum diameter of 3 cm in the pancreatic head, responsible for the biliary compression (Fig. 1).
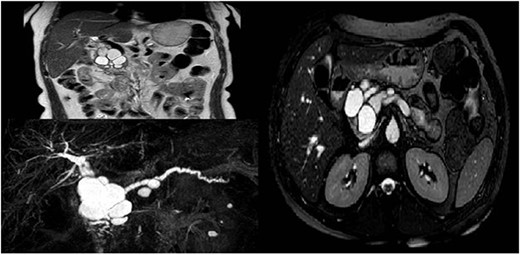
Radiological features of a large complex cyst of the pancreatic head.
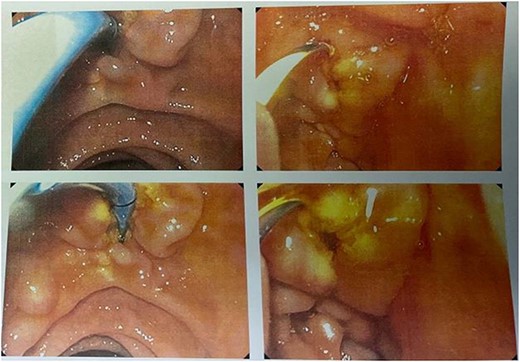
The subsequent EUS confirmed the presence of an IPMN-like lesion, although it was not possible to detect a connection with the pancreatic duct, because of the size of the cyst. There was no evidence of worrisome features or solid lesions (Fig. 2).
The multidisciplinary meeting decides to offer surgery because of the patient’s symptoms and the possibility of a cystic lesion with associated malignant transformation. The patient underwent a pylorus-preserving pancreaticoduodenectomy with locoregional lymphadenectomy. On surgical examination, the lesion appeared a large nonhomogeneous bulging in the head of the pancreas, without involvement of adjacent organs or evidence of peritoneal nodules. Postoperative course was free of adverse events and the patient come back home 10 days later.
PATHOLOGY
Gross examination of the resected specimen revealed numerous cysts ranging from 2 to 25 mm in diameter with a thin translucent wall diffusely distributed throughout the pancreatic head, containing clear white serous fluid and not communicating with ductal pancreatic system; on cyst wall, solid areas or papillary excrescences are not present.
On microscopic examination, the pancreatic parenchyma appeared atrophic and replaced by a loose fibrous tissue that was poorly collagenized. The most evident aspect was represented by the presence of numerous cysts of variable sizes and lined by epithelial cells without atypia. Ductal epithelium was admixed with the acinar cells and focal mucinous, clear or squamoid cell change was also observed. The cysts contained eosinophilic amorphous material and acidophilic concretions. They were generally connected to small clusters of acinar cells forming acini, which opened into the cyst lumen (Fig. 3).
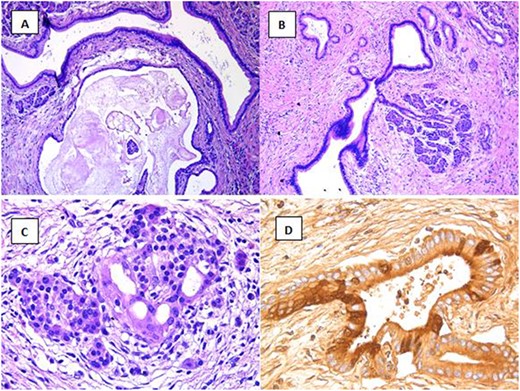
Multiple cists of variable sizes containing amorphous material (A, H&E ×10) and connected to acini (B, H&E ×10); Islet of Langerhans with microcystic dilation (C, H&E ×20); positive immunohistochemical stain for trypsin (D).
There was a crescens of lesions from initial aspects of cystic transformation of the acini to the formation of multiple cysts of various sizes with almost total disappearance of the normal acini. The islets of Langerhans were loose and also showed microcystic dilations.
We can frequently observe chronic inflammatory perineural, peri- and intra-insular infiltrates; ovarian type stroma, necrosis or infiltrative growth is absent and background pancreas typically lacks pancreatic intraepithelial neoplasia. All these features were reminiscent of obstructive pancreatic changes, although a clear cause of this type was not evident.
Immunohistochemical stains for Trypsin, chymotrypsin, lipase, CKAE1–AE3, CK7, CK8 and CK18 were diffusely positive. CK19 stained intervening patches of the ductal epithelium of the lining of the cysts. Alpha amylase, synaptophysin and chromogranin A were all negative. In the differential diagnosis, cystic variant of acinar cell carcinoma (acinar cell cystadenocarcinoma), IPMN, mucinous cystic neoplasm and serous cystadenoma have been into account. Overall, microscopic findings were consistent with ACT.
DISCUSSION
ACT of the pancreas is an extremely rare benign lesion that was first described by Albores–Savaedra [2] and termed ‘acinar cystadenoma’. Differently from neoplasms originating from pancreatic ducts, alterations in KRAS, GNAS, RNF43, TP53, CDKN2A and SMAD4 have not been reported in these lesions, and in general, no genetic alterations indicative of a neoplastic pathogenesis have been found. For these reasons, the 2019 WHO classification of digestive tumors reclassified ACT as a nonneoplastic cystic lesion [4]. ACT mainly affects females, is usually detected incidentally, but when it is large, can be symptomatic, as in our case. The most common location of ACT is the head of the pancreas and less frequently the entire pancreas or the tail. CT and MRI findings are nonspecific, but the presence of multiple cysts and absence of connection with the pancreatic ducts are supportive for diagnosis. In the differential diagnosis, the neoplastic cystic tumors, including mucinous cystic neoplasms, serous cystic neoplasms and IPMN, should be considered [4]. Histologically, the lesion consists of cysts predominantly lined by patches of acinar and ductal bland epithelium. Interestingly, in our patient, the cystic transformation also affects the islets. To our knowledge, this aspect has never been described. The entity presents a challenging diagnosis for the clinician and is often first established after surgery by microscopic examination of the resected specimen. A correct diagnosis is important as clinical management and follow-up depend on it.
CONCLUSION
ACT of the pancreas is a rare and newly recognized benign pancreatic cystic neoplasm with unknown malignant potential. A preoperative diagnosis of ACT is difficult to establish, even after multiple and invasive investigations. The indication for surgery should be based on the patient’s symptoms, considering that no malignant transformation has ever been reported so far. However, difficulties to differentiate ACT from potentially malignant cysts can lead to surgical resection, in order to obtain a pathological diagnosis.
AUTHORS’ CONTRIBUTIONS
William Sergi: design of work and manuscript writing. Stefano D’Ugo: co-author. Stefania Vadrucci: review of literature and author of discussion. Farshad Manoochehri, Stefano Garritano, Tiziana Marchese, Ivan Botrugno, Annarita Libia, Norma Depalma: data collection. Marcello Spampinato: supervisor.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal on request.
ETHICAL APPROVAL
In our institute, the approval of the ethics committee for the retrospective analysis of a clinical case report is not required.
GUARANTOR
Spampinato Marcello.
REGISTRATION OF RESEARCH STUDIES
The submitted case report is not a research study.
PROVENANCE AND PEER REVIEW
Not commissioned, externally peer-reviewed.
Footnotes
†The paper has been written in line with the SCARE criteria [1]. Consent to the processing of data for scientific purposes is requested and signed at the time of admission and kept in the medical record; the authors confirm that the patient’s parents have signed consent to the publication of the data.



