-
PDF
- Split View
-
Views
-
Cite
Cite
Waleed Albishi, Abdulrahman Alaseem, Sarah Aljasser, Faten Almohideb, Mamdouh Almalki, Ahmed F AlFaleh, Intraosseous extension of supraspinatus calcific tendonitis in a young patient with severe shoulder pain: a rare case report, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad354, https://doi.org/10.1093/jscr/rjad354
Close - Share Icon Share
Abstract
Calcific tendinopathy is one of the causes of shoulder pain and limited range of motion when it affects the rotator cuff tendons. Complications of such a condition are rare and include intraosseous and intramuscular migration. Calcific tendonitis can be classified as acute, subacute or chronic based on the onset of symptoms. The incidence of calcific tendonitis affects females more than males, with the median age of onset being between 40 and 60 years old. Diagnostic modalities include radiographs and computed tomography (CT); however, these are suboptimal when compared to the sensitivity of magnetic resonance imaging. Ninety percent of these cases are treated non-surgically. We present a rare case of a young female patient with right shoulder pain and limited range of motion secondary to the intraosseous migration of calcific tendonitis. The patient’s symptoms were resolved after a CT-guided percutaneous bone biopsy of the lesion. Clinical correlation with the aid of imaging and histopathology is a multimodal approach to help diagnose and treat such conditions.
INTRODUCTION
Calcific tendinitis, also known as hydroxyapatite deposition disease, accounts for 7% of the shoulder pain associated with rotator cuff tendons [1, 2]. Rotator cuff tendonitis can lead to muscle and/or bone migration of calcific deposits and it results in bone marrow inflammation [1]. The incidence of calcific tendonitis affects females more than males, with the median age of onset being between 40 and 60 years old [3]. In our case, the patient was 29-year old at the onset, which would be considered unusual for this condition.
The risk factors for calcific tendonitis include endocrine diseases, such as thyroid disease and diabetes mellitus, alcohol consumption, history of trauma or surgical intervention to the shoulder [3]. Calcific tendonitis is classified based on the onset of symptoms into acute, subacute and chronic types [4].
Patients may be asymptomatic or may present with symptoms of shoulder pain and/or restricted range of motion, depending on the size of the particles [5]. Diagnostic modalities include radiographs and computed tomography (CT); however, they are suboptimal compared to the sensitivity of magnetic resonance imaging (MRI) [6]. Ultrasound (US)-guided aspiration and/or irrigation can be used for diagnostic and therapeutic purposes [6]. In regard to management, treatment options range from nonsurgical management—such as anti-inflammatory medications, physical therapy modalities that focuses on reducing the pain and improving range of motion—to surgical management, such as open or arthroscopic surgeries [3]. Ninety percent of these cases are treated non-surgically and include rest with an arm sling, anti-inflammatory medication (both non-steroidal and steroid oral medication) and intra-articular injection. Cold and heat packs, range of motion exercises as nonoperative management and diathermy, short-wave and radiation therapy can also be used [4].
CASE REPORT
A healthy 29-year-old female patient reported having chronic right shoulder pain for 10 years, which became progressively worse over the course of the 2 weeks prior to her visit in the clinic. The nature of the pain is generalized and continuous. The patient also reported night pain and weight loss over the previous 3 weeks. The pain was aggravated by motion and was relieved by nonsteroidal anti-inflammatory drugs. She reported having no recent or previous trauma to the shoulder. Upon examining the patient, she was using an arm sling for pain relief and her right shoulder was painful to touch with no underlying swelling, redness, hotness or masses. Active and passive ranges of motion were limited due to pain.
Radiographs showed calcification around the region of insertion of the supraspinatus tendon on the humeral head. No fracture lines or surrounding soft tissue swelling were noted. Radiographs of the right shoulder are shown in Fig. 1.
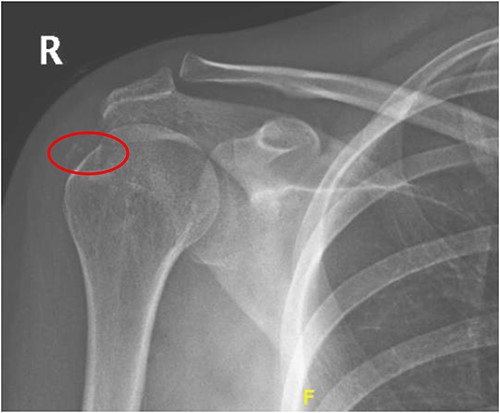
Radiograph of right shoulder showing calcification around the insertion of supraspinatus tendon.
An MRI of the right shoulder showed calcifications over the supraspinatus tendon with an intraosseous lesion mimicking an aggressive or benign skeletal neoplasm (see Figs 2 and 3).
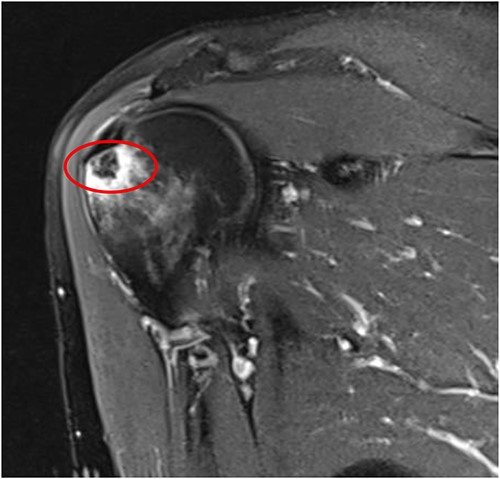
Coronal T2 image of right shoulder showing hypointense lesion; note: the red circle indicates the intraosseous extension of calcified deposits originating from calcified supraspinatus tendon, with surrounding marrow edema.
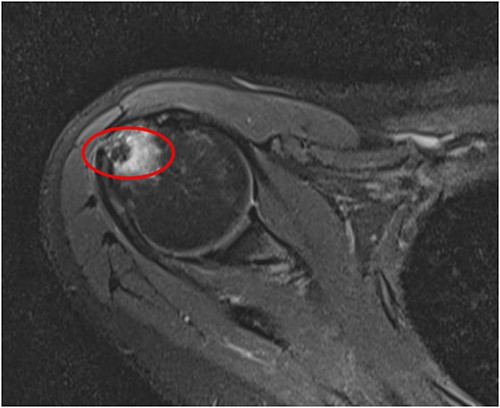
Axial T2 image of right shoulder showing hypointense lesion; note: the red circle indicates the intraosseous extension of calcified deposits originating from calcified supraspinatus tendon, with surrounding marrow edema.
After consulting the musculoskeletal radiologist, the patient underwent computerized tomography (CT)-guided percutaneous bone biopsy. The benefits and risks were explained to the patient, and informed consent was obtained prior to the procedure.
Under local anesthesia, we used aseptic technique and CT guidance with a 11-gage coaxial bone biopsy needle to obtain two samples from the right proximal humerus head bony lesion through lateral approach. All specimens were sent for histopathology analysis with formalin. The patient tolerated the procedure well with no immediate post-procedure complications. The biopsy size was 1.5 cm by 1.0 cm by 0.3 cm and showed bone tissue with fibrosis, chronic inflammation and calcifications. It was negative for carcinoma.
After the biopsy, the patient's symptoms significantly resolved, including the alleviation of pain and the regaining of full range of motion. The patient resumed normal activities of daily living without complaint.
DISCUSSION
The prevalence of calcific tendonitis is estimated to be 3%, with the peak age at onset being between 40 and 60 years old with a female predominant picture [6]. The pathogenesis of this condition has not been completely established. The most-described theory in the literature, however, attributes it to a cell-mediated response. Tendon cells undergo fibrocartilaginous metaplasia when intratendinous oxygen level drops, a process which ultimately leads to calcium formation within the tendons [5].
In the late 1980s, Uhthoff et al. described the process of calcific tendonitis and how it occurs in three stages. The first stage is pre-calcific, in which there is fibrocartilaginous metaplasia of the tenocytes. The second stage is the calcific stage, in which it subdivides into formative phase, resting phase and resorptive phase. The formative phase is characterized by the formation of calcific deposits. The resting phase lacks inflammation or vascular infiltration, and the resorptive phase is characterized by resorptive phagocytosis and vascular infiltration. The third stage is the post-calcific stage, which is characterized by remodeling of the tendon via granulation tissue and fibroblasts. Each stage of this process has distinct features on imaging which correlate with a patient’s symptoms [5, 7]. Our patient had 10 years of mild symptoms and a sudden peak of pain that lasted 2 weeks prior to her clinic visit.
Complications and unusual sequelae of calcific tendonitis have been described in the literature—particularly cases of intraosseous and intramuscular migration of calcific deposits [8]. The migration of calcium hydroxyapatite crystals to the surrounding musculature occurs through tendons and most commonly through the supraspinatus and infraspinatus tendons. However, intraosseous migration of crystals is believed to happen through enzymatic action and subsequent bony involvement in the form of cortical erosion, subcortical migration or intramedullary dissemination [9].
Different imaging modalities can be used in augmentation to reach a diagnosis. Radiographs, CT and MRI technology are all used to identify specific radiological characteristics of the calcium deposits and locations. MRI technology has the ability to show surrounding soft tissue in detail. MRI scans show calcifications as low-signal intensity masses on all sequences, while the surrounding inflamed tissue flares with high-intensity signals [6]. US can help identify calcific plaque morphology and can be used for therapeutic purposes with US-guided aspiration or irrigation of calcific deposits. Image-guided interventional procedures have been shown to be less invasive and highly effective in the treatment of such cases [10, 11].
The osteolytic appearance detected in the MRI mimics a tumor-like lesion and, according to Porcellini et al., there is a correlation between the size of calcification deposits and intraosseous involvement. The size of calcification deposits are larger when there is intraosseous involvement [12]. Usually, the calcified tendonitis is self-limiting and responds well to conservative management [13]. In our case, the patient responded well and had resolution of all symptoms after the biopsy was done. The main possible reason for this is that the biopsy indirectly decompressed the subacromial area, which relieved the inflammation and provided extra space in the area. Although one study showed that intraosseous lesions generally respond to arthroscopic debridement, and it is the preferred treatment choice [13], we found that taking multiple biopsy specimens using a large-gage coaxial bone biopsy needle can help treat the patient’s condition without the need for surgery. This opens the door to the use of less-invasive therapeutic approaches when treating this rare shoulder pathology.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grants from funding agencies in the public, commercial or not-for-profit sectors.
CONSENT
The authors obtained all appropriate patient consent forms. In this form, the patient provided consent for the images and other clinical information to be reported in the journal.
DATA AVAILABILITY
All data are available upon request.
AUTHORS’ CONTRIBUTIONS
The authors testify that all persons designated as authors qualify for authorship. Additionally, all authors have reviewed and approved the final version of the manuscript for submission.



