-
PDF
- Split View
-
Views
-
Cite
Cite
Liwei Ying, Hua Luo, Xiaofang Ying, Zhong Zhu, Epidermoid cyst beneath the scar after total knee arthroplasty: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad208, https://doi.org/10.1093/jscr/rjad208
Close - Share Icon Share
Abstract
The epidermal cysts are benign cysts most commonly found in the head, neck and trunk. An epidermal cyst of the knee is an unusual complication developed after total knee arthroplasty. Here, we present a case of an 83-year-old man with a palpable mass in the left knee located beneath the scar, 3 years after total knee arthroplasty. The patient underwent complete surgical excision of the mass. Histological analysis revealed an epidermoid cyst.
INTRODUCTION
Epidermal cysts are the most common benign epithelial tumors in humans [1]. Epidermal cysts can result from various surgical procedures that lead to the implantation of epidermal cells into deeper tissues under the dermis, but there are few reports of postoperative occurrences of epidermal cysts in the knee. To the best of our knowledge, an epidermal cyst is a rare complication caused by total knee arthroplasty.
Here, we describe a case of epidermal cyst that occurred after total knee arthroplasty. The aim of this report is to introduce this rare complication of total knee arthroplasty and present preventive and treatment measures.
CASE REPORT
An 83-year-old man was admitted to our hospital with a skin lump on the incision located on the left knee without other concomitant symptoms (Fig. 1). He received left total knee arthroplasty 3 years ago. A mass, the size of a grain of rice, appeared on the incision 1 month after operation. Within 3 years, the mass gradually increased to the size of a pigeon egg. Physical examination revealed a skin-like, ~3 × 3 × 2 cm cystic solid mass with a clear boundary, a soft texture and painless touch, protruding on the skin surface. Laboratory data showed that inflammation index and tumor series index were normal. Ultrasonography (US) shows a 2.5 × 2.5 × 1.6 cm heterogeneous hypoechoic mass with regular borders (Fig. 2).
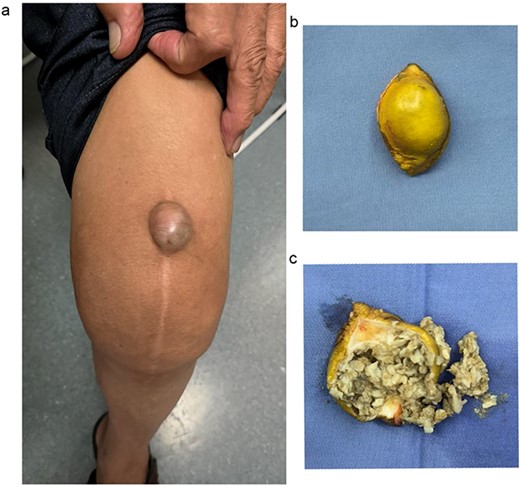
(a) A mass beneath the scar after total knee arthroplasty; (b) completely excised cyst with skin over it; (c) the appearance of cyst contents.
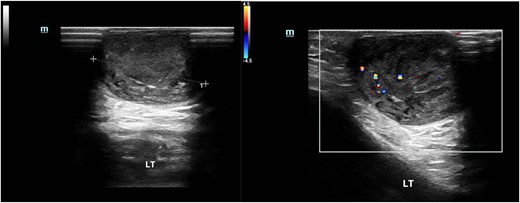
Ultrasound image of the epidermal cyst. US shows a 2.5 × 2.5 × 1.6 cm heterogeneous hypoechoic mass with regular borders.
After refining the related clinical exams, this skin mass was resected under general anesthesia. The final histopathological examination showed cystic wall lined with stratified squamous epithelium, a granular layer containing keratin and subcutaneous fibrous tissue hyperplasia without any nuclear atypia (Fig. 3). The patient provided informed consent for the publication of his clinical data and accompanying images. Postoperatively, the patient showed good recovery.
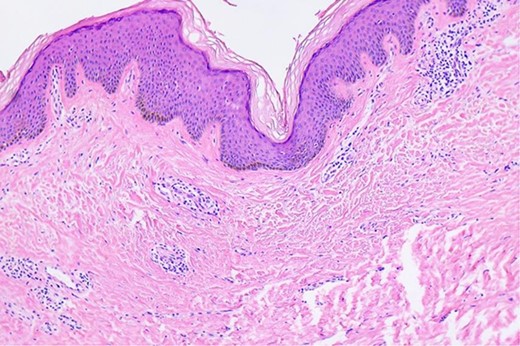
Microscopic findings of the epidermal inclusion cyst. A cystic lesion is lined by benign stratified squamous epithelium filled with abundant lamellated basket weave keratin (hematoxylin and eosin staining ×40).
DISCUSSION
To the best of our knowledge, the epidermal cyst is an unusual complication developed after total knee arthroplasty. Epidermal cysts, formed of cystic fluid, are mostly secondary to trauma, resulting from the proliferation of epidermal cells within a circumscribed space of the dermis [2]. Epidermal cysts are more common in men as in women with a ratio of 2:1, which may occur at any age and are usually diagnosed when the person notices a mass or dome-shaped lesion on his skin [3, 4]. Epidermoid cysts frequently appear on the trunk, neck, face and scrotum, behind the ears and in the palmoplantar region. Few literatures report the occurrences of epidermal cysts in the knee [4]. Although epidermoid cysts are usually benign and asymptomatic, they may secondarily become inflamed, infected or, rarely, develop into a malignancy [5].
Because of the potential for malignant transformation, surgical excision of the mass is recommended, especially when the cyst is large (≥2 cm) and palpable, or when it causes the patient discomfort [6]. All excisions should be sent for histologic analysis. Three main techniques are used to excise cysts: conventional complete excision, minimal excision and punch biopsy excision. In minimal incision methods for removing an epidermal cyst, the cyst contents and lining can be expelled through a small opening using lateral pressure or using negative-pressure suction [7]. Excision with punch biopsy technique may be used if the size of the lesion permits. Epidermoid cysts may be removed via simple excision or incision with removal of the cyst and cyst wall though the surgical defect. When the entire cyst wall is not removed, the lesion may recur [8]. TKA is the surgical replacement of a damaged knee joint with artificial joints. There is only a thin layer of soft tissue between the cyst wall and the artificial joint. Therefore, the patient in this study underwent complete surgical excision of the mass to reduce the risk of periprosthetic joint infection and cyst recurrence.
In this case, the articular capsule, subcutaneous and skin layers were sequentially closed with one absorbable line (PDP359 and VCP359), a 2-0 VCP317 suture and a 3-0 VCP316 suture, respectively. Compared with intermittent closure, running subcuticular closure after TKA results in a better appearance [9]. All kinds of surgical and invasive procedures can induce epidermal inclusion cysts. To prevent the occurrence of epidermal cysts, surgeons should use a fresh, sharp scalpel and should be careful not to push epithelium into the deeper tissues. Profuse saline irrigation of the operation wound to wash out epithelial debris before surgical wound closure. Skin incision suture requires accurate reapproximation of skin margins [10].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
AUTHORS' CONTRIBUTIONS
Concept/idea/research design: L.Y. and Z.Z. Writing and revision: L.Y. Data collection/data analysis: H.L. and X.Y.
DATA AVAILABILITY
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Medical Ethics Committee of Taizhou Hospital Affiliated to Wenzhou Medical University approved this study (K20221219). All the procedures were conducted according to the Declaration of Helsinki. The need for informed consent was waived by the Medical Ethics Committee of Taizhou Hospital Affiliated to Wenzhou Medical University as the study’s retrospective design.



