-
PDF
- Split View
-
Views
-
Cite
Cite
Nichaphat Phancharoenkit, Anuparp Thienhiran, Pipit Burasakarn, Pusit Fuengfoo, Sermsak Hongjinda, Acute cholangitis caused by a huge hepatic simple cyst: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 2, February 2023, rjad056, https://doi.org/10.1093/jscr/rjad056
Close - Share Icon Share
Abstract
Simple hepatic cysts are usually asymptomatic and rarely cause complications. Among the rare complications of liver cysts, intracystic hemorrhage is one of the most frequent, and can result in a rapid increase in cyst size. Some simple hepatic cysts may be large and can present with pressure effects, such as abdominal discomfort or obstructive jaundice. A 68-year-old female with a simple huge hepatic cyst was scheduled elective laparoscopic fenestration in 6 weeks. Before the operation, she developed acute cholangitis, resulting from an acute increase in cyst size due to intracystic hemorrhage. Upon open fenestration, 6.1 L of chocolate-like fluid was drained. A huge simple hepatic cyst complicated by intracystic hemorrhage resulted in an acute increase in cyst size. Distortion of the extrahepatic bile duct by the cyst obstructed the bile flow. Acute cholangitis was eventually developed.
INTRODUCTION
Simple hepatic cysts are the most common benign lesions of the liver [1]. They are usually asymptomatic [2] and do not cause complications [3]. Among the rare complications of liver cysts, intracystic hemorrhage is one of the most frequent, and can result in a rapid increase in cyst size. Some simple cysts may be large and present with pressure effects, e.g. abdominal discomfort or obstructive jaundice [2].
We report rare complications of a huge hepatic cyst. Our patient presented with a symptomatic hepatic cyst was planned for laparoscopic fenestration. Before the operation, she developed acute cholangitis, resulting from an acute increase in cyst size due to intracystic hemorrhage.
CASE REPORT
This is a case of a 68-year-old female with history of provoked venous thromboembolism. A hepatic cyst was incidentally found during echocardiography. At initial presentation, the patient was asymptomatic. Her liver function tests (LFT) and tumor markers were normal. Enhanced computed tomography (CT) showed a benign appearing cystic lesion (14 × 20 × 21 cm) that occupied the right liver lobe, which resulted in mild intrahepatic duct (IHD) dilation in the left hepatic lobe with medial displacement of right kidney, and several gallstones.
Two years later, she came back to outpatient surgery department due to abdominal discomfort. Physical examination revealed a large palpable mass in the right upper quadrant. Laboratory examination showed total bilirubin 0.44 mg/dl and alkaline phosphatase (ALP) 192 U/ml. CT showed no significant change cyst size (15 × 20 × 21 cm). She was diagnosed with symptomatic simple hepatic cyst and was scheduled laparoscopic fenestration in 6 weeks.
On the morning of the day of surgery, she developed fever and acute right upper quadrant pain. Physical examination revealed a body temperature of 38.1°C, heart rate of 110 beats per minute, blood pressure of 142/96 mmHg, good consciousness, icteric sclerae, distended abdomen and right upper quadrant tenderness without sign of peritonitis. The white blood cell was 12,600/ul with 87.9% of neutrophil. LFT showed total bilirubin 5.09 mg/dl, direct bilirubin 4.57 mg/dl and ALP 429 U/L.
She was clinically diagnosed with acute cholangitis. Possible differential causes were choledocholithiasis or complications of hepatic cysts. The patient was sent for a CT scan, which revealed an increase in hepatic cyst size (22 × 24 × 32 cm), causing increased IHD dilation in the left hepatic lobe and hepatic segment 5, without common bile duct dilation (Fig. 1).
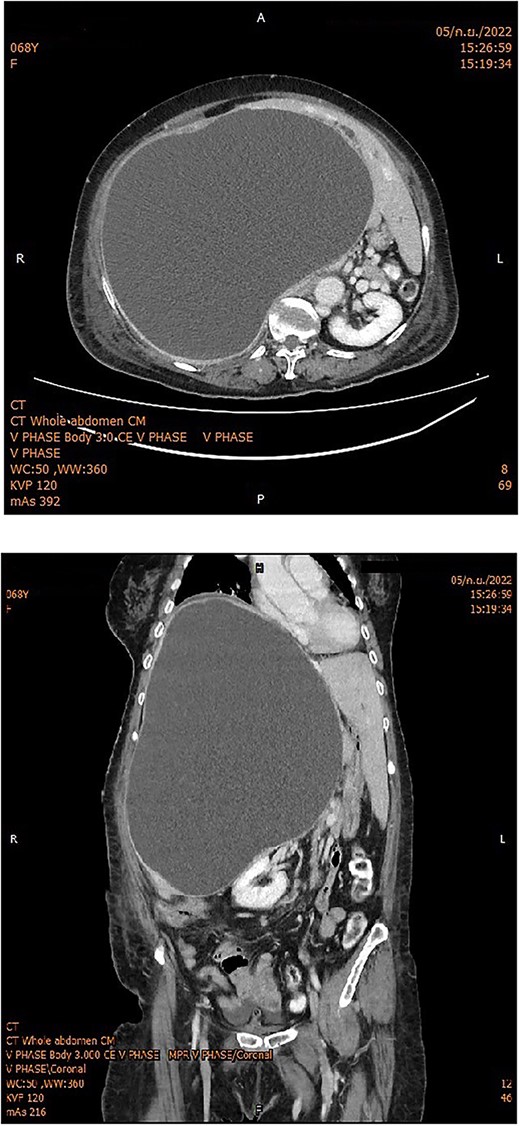
Whole abdomen enhanced CT showed a huge hepatic cyst occupying the right lobe of the liver with intrahepatic bile duct dilatation in the left lobe; the right kidney was displaced into the midline.
We concluded that the patient had acute cholangitis due to external hilar bile duct compression caused by acute changes in hepatic cyst size. The most likely cause of the acute increase in cyst size was intracystic hemorrhage. Intravenous antibiotics were administered, and general support was provided. Therefore, the surgery was postponed the next day until the patient was stabilized.
The patient was conscious and had stable hemodynamics. Laparoscopic fenestration was performed. A 10-mm camera port was placed below the umbilicus. Percutaneous cyst aspiration was then performed. After 1,000 ml of chocolate-colored fluid was retrieved, the hepatic cyst did not decrease in size. The surgery was converted to open fenestration (Fig. 3) and 6,100 ml of cyst fluid was aspirated. The cyst wall was unroofed using an ultrasonic sealing device. The operative time was 3 h and 45 min.
The acute cholangitis was improved after surgery. Serum bilirubin levels became normal on postoperative Day 8 (total bilirubin 0.99 mg/dl, direct bilirubin 0.53 mg/dl), but ALP did not normalize until discharge. The patient also experienced cardiogenic pulmonary edema and hospital-acquired pneumonia. She was discharged with full recovery and independence on postoperative day 21.
The subsequent endoscopic retrograde cholangiopancreatography showed no filling defect or luminal narrowing (Fig. 2). Pathological examination of the cyst wall revealed a benign cyst lined by cuboidal cells with acute chronic inflammation (Figs 4 and 5).
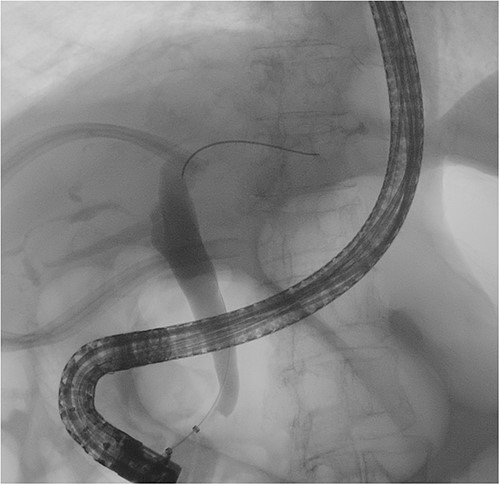
Cholangiography showed a smooth common bile duct wall without intraluminal filling defects.
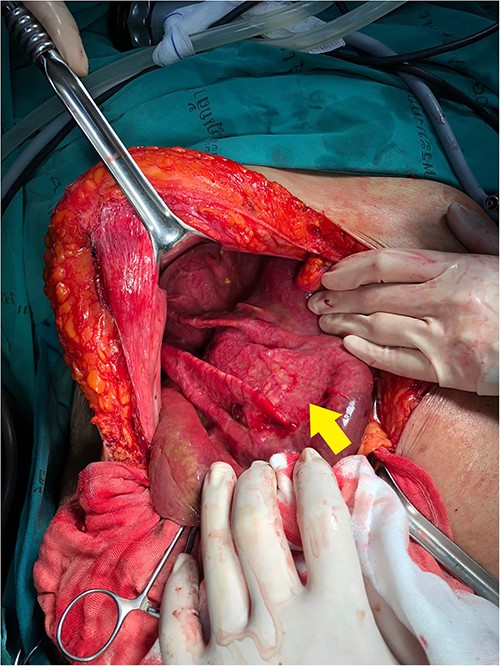
Intraoperative findings showed a collapsed hepatic cyst (arrow) in right liver lobe after cyst fluid was removed.
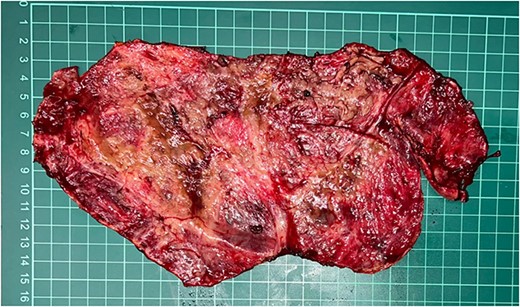
Gross pathology shows the inner surface of cystic wall that was excised.
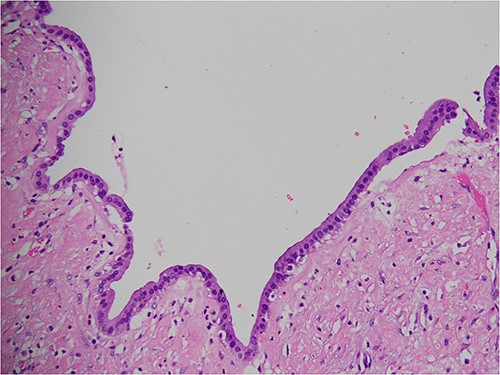
Pathological examination of the resected cyst wall showed a benign cyst lined by cuboidal cells.
DISCUSSION
Simple hepatic cysts rarely cause complications. They do not connect to bile duct, and they contain clear serous fluid [3]. Treatment is not required unless complications develop. The treatment options include surgery or minimally invasive procedures. No randomized controlled trials comparing these options have been published. Guidelines recommend treatment based on the best available technique [4]. For very large hepatic cysts, like the one in our patient, the proper treatment is fenestration. Fenestration involves removing the cystic wall to create communication between the cyst and peritoneal cavity. Complications in this patient were intracystic hemorrhage, obstructive jaundice and acute cholangitis.
Intracystic hemorrhage cannot be detected by CT. Guidelines suggest that ultrasound or magnetic resonance imaging may help identify bleeding in cysts [4]. In our case, CT showed only an increase in size. Due to the slow-growing nature of simple cysts, acute increased cyst size may imply bleeding within the cyst. Intracystic hemorrhage can be observed intraoperatively, with cyst fluid showing chocolate-like color. Due to the enlarged cyst, increased IHD dilatation in the left hepatic lobe and liver segment 5 was observed, but there was no common hepatic duct dilation. Thus, the obstruction was around the hilar level. The huge cyst distorted the extrahepatic bile duct, causing external bile duct compression. The obstruction of bile flow progressed from partial to complete. Laboratory results demonstrated isolated abnormal ALP levels, without hyperbilirubinemia, and subsequent tests showed elevated both ALP and bilirubin levels.
Obstructive jaundice due to simple hepatic cysts is rare. Previous reports have described liver cyst located in central area near hepatic hilar [5–9]. No reported cases suffered from acute cholangitis. A possible explanation is the slow-growing nature of simple hepatic cysts, which do not cause an acute increase in intraductal pressure. Increased intraluminal pressure of the bile duct impairs tight junction of the biliary epithelium, leading to cholangiovenous and cholangiolymphatic reflux [10, 11].
Few cases of acute cholangitis associated with simple hepatic cysts have been reported. Keunho et al. [12] reported a small liver cyst near the left hepatic hilum causing IHD dilation in the left liver lobe and acute cholangitis. Only ALP was elevated in this case. Serum bilirubin was normal because only the left hepatic duct was affected. The other two reports described acute cholangitis with secondary simple hepatic cyst infections [13, 14].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data are available in the article.



