-
PDF
- Split View
-
Views
-
Cite
Cite
Pierre-Antoine Debordes, Ceyran Hamoudi, Noelle Weingertner, Antonio Di Marco, Superficial acral fibromyxoma: a case of missed diagnosis, Journal of Surgical Case Reports, Volume 2023, Issue 2, February 2023, rjad027, https://doi.org/10.1093/jscr/rjad027
Close - Share Icon Share
Abstract
Superficial acral fibromyxoma (SAFM) is a rare, benign, slow-growing fibroblastic tumour of the soft tissue that is part of the group of myxoid soft-tissue neoplasms. It is a rare entity and usually occurs in the acral regions. We report the case of a 64-year-old man who presented to the emergency room for a lesion expected to have occurred as a result of an ingrown toenail. Because this patient had a history of repeated recurrences despite multiple surgical wedge excisions, we performed a complete surgical excision, and the pathological analysis confirmed the suspected diagnosis of SAFM. There was no recurrence at the 6-month follow-up. This case highlights the fact that this tumour is still misunderstood and underrecognized by surgeons and this often leads to delayed diagnosis. Although it is a rare entity, clinicians should be aware of this tumour in cases of recurring ingrown toenails.
INTRODUCTION
Superficial acral fibromyxoma (SAFM) is a rare, benign tumour first described by John Fetsch et al. in 2001 [1]. It commonly affects acral regions with a distinct predilection for the periungual and subungual regions of the fingers and toes, but can affect other areas such as the palm, heel and ankle [2]. It is usually painless and develops as a slow-growing solitary nodule confined to the dermis and subcutaneous tissue. It affects a young to middle-aged population and occurs more frequently in men (male:female ratio of 2:1) [1]. Nail involvement can be seen, with features of hyperkeratosis or onycholysis.
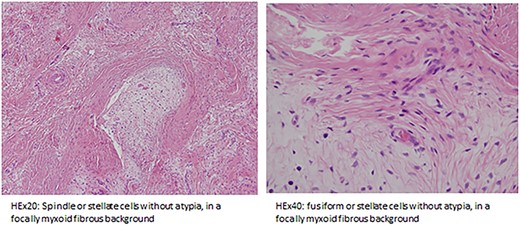
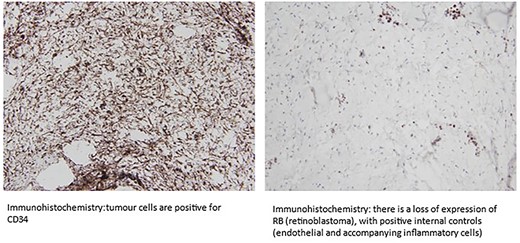
A classical histopathological feature of these tumours is the dermal and sometimes subcutaneous proliferation of spindle-shaped fibroblast-like cells or stellate cells in a myxocollagenous matrix with increased vasculature [3]. The tumour is usually well-circumscribed but nonencapsulated. Immunohistochemical analysis reveals tumour cell expression of CD34 and sometimes epithelial membrane antigen and smooth muscle actin. Loss of retinoblastoma (RB) expression is noted in the majority of tumours [1, 4, 5].
The clinical differential diagnosis of SAFM includes fibrous histiocytoma, dermatofibrosarcoma, cutaneous myxoma, acral fibrokeratoma, myxoinflammatory acral fibroblastic sarcoma, sclerosing perineurioma, myxoid neurofibroma, fibroma of the tendon sheath, giant cell tumour of the tendon sheath and glomus tumour [2, 5, 6].
Radiological imaging can reveal underlying bony erosions and scalloping due to the mass effect of the tumour. Sawaya et al. reported that bone erosion may be present in around one-third of SAFM cases [7].
In this case report, we describe the case of a patient with an SAFM in which a recurrent slow-growing mass of the left first toe was repeatedly diagnosed and treated as an ingrown toenail in the emergency department and by surgeons.
CASE REPORT
A 64-year-old sub-Saharan African male with diabetes with a long-standing history of a recurring slow-growing periungual mass of the left great toe after multiple surgical wedge excisions for an ingrown toenail presented to the emergency department with acute pain, bleeding and local swelling of the lesion. Physical examination revealed a painful periungual mass (Fig. 1). The toe’s range of motion was conserved and there was no sign of ischemia. An X-ray was performed and did not reveal any bone erosion or osteolytic lesions (Fig. 2). Neither computer tomography (CT) scanning nor magnetic resonance imaging (MRI) were performed. The emergency doctor initially treated the lesion with silver nitrate treatment, and the patient was referred for an orthopaedic consultation for treatment of a recurrent ingrown toenail.


During the orthopaedic consultation, because the patient had a history of repeated recurrences despite multiple surgical wedge excisions and because no anatomopathological analysis had previously taken place, the patient was taken to the operating theatre and a complete surgical excision with free margins was performed without complications. The lesion was soft and ulcerated and was sent for anatomopathological analysis (Fig. 3). The lesion measured 21 × 15 mm within the sample measuring 31 × 20 × 21 mm.

Analysis of the lesion revealed a superficial, dermal tumour consisting of a lobulated proliferation of spindle cells without atypia, mitosis or necrosis, embedded in a fibrous and focally myxoid stroma. Immunohistochemistry showed that the spindle cells were CD34 positive and demonstrated a loss of RB1 expression. The clinical and anatomopathological findings were consistent with a diagnosis of SAFM (Figs 4–6).
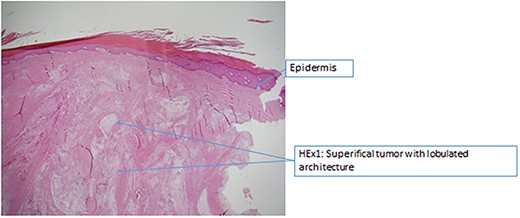
Histopathology – superficial tumour with lobulated architecture.
The wound was left open for secondary healing and the patient received careful wound care. At the 6-month follow-up, the patient did not complain of any aesthetic or functional issues or pain and there was no evidence of local recurrence (Figs 7 and 8).


DISCUSSION
SAFM is a rare soft-tissue tumour found mainly in acral regions, and it usually involves the periungual or ungual region. In a recent literature review, Crepaldie et al. reported 314 cases between 2001 and 2019 [8]. They found that SAFM affected the toes in 46% of cases and fingers in 39.1%. Incidence in men was higher; around 60% of cases occurred in men [8].
SAFM may present as a nodule in the periungual folds with or without affecting the nail apparatus. In some cases, as in ours, the clinical presentation might be a periungual ulcerated lesion. A history of trauma of the affected site has been reported in literature; our patient, however, did not report any previous trauma.
Bone involvement (bone erosion or osteolytic lesions) can be present in one-third of cases [7]. In our case, standard X-ray did not reveal any bone involvement. We did not perform a CT scan or MRI before surgical resection since it would have led to a delayed diagnosis and extra cost. Nevertheless, in unclear cases, MRIs can prove useful. Moreover, a CT scan can detect soft-tissue calcifications and bone erosions [9]. High-resolution ultrasonography (US) with Doppler is readily accessible and cost-effective and can detect small benign tumours and tumour-like conditions of the nail apparatus. However, the quality of the US examination remains operator dependent [9].
The differential diagnosis of SAFM is vast, and therefore immunohistochemical analysis is essential to distinguish SAFM from other lesions. Moreover, an important pathological differential diagnosis is dermatofibrosarcoma, which also expresses CD34 but retains RB1 expression and is characterized by a specific genetic alteration. Another important differential diagnosis is myxoid neurofibroma, since tumour cells in SAFM often have a neural-like appearance. However, neurofibroma consistently stains positive for the S100 protein and does not show the increased vasculature observed in SAFM [5].
The natural course of SAFM is benign. Nevertheless, transformation to a low-grade malignant tumour is possible; however, no malignant transformation has been reported until 2001 [4, 8]. Local recurrence rates of 22–24% have been reported [1, 10], therefore surgical excision with adequate margins must be performed. Local recurrences are non-destructive and can be cured by re-excision. Moreover, such resection should be performed by experienced surgeons in operating theatres and histopathological analysis should be performed. In cases of a typical history and painless mass, we do not recommend such excision in emergency facilities. Furthermore, short-term follow-up of 6 months to 1 year is necessary because of SAFM’s slow-growing nature and possible recurrence [6].
In conclusion, SAFM remains misunderstood and underrecognized because of its rarity. Missed diagnosed and partial resection in emergency settings may delay diagnosis and lead to recurrence. SAFM should always be suspected when patients present with soft-tissue tumours of the fingers and toes, especially when there is a painless slow-growing mass or a history of recurrence after surgical excision.
Moreover, our case highlights the importance of a multidisciplinary approach in such cases.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICAL APPROVAL
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of this journal on request.



