-
PDF
- Split View
-
Views
-
Cite
Cite
Shinji Kobayashi, Yuichiro Yabuki, Madoka Sugiyama, Takashi Hirakawa, Kenji Kurosawa, Submucosal dissection to close wide cleft palate with folded mucoperiosteum for bilateral cleft lip and palate with popliteal pterygium syndrome, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad575, https://doi.org/10.1093/jscr/rjad575
Close - Share Icon Share
Abstract
Characteristic features of popliteal pterygium syndrome (PPS) associated with the craniofacial region include cleft palate, syngnathia, and difficulty with reconstruction. We developed a new procedure of submucosal dissection with periosteotomy to close the folded mucosa in bilateral cleft lip and palate patients with PPS. This technique could be applicable for patients with wide cleft palate.
Introduction
In patients with cleft palate, closing a wide, short cleft palate is difficult. In particular, tissue defects in the hard and soft palate make closure extremely difficult. Areas that cannot be covered with palatal mucosa are likely to later become fistulas or scars, which can adversely affect maxillary growth and speech outcomes. Covering as much of the hard and soft palate as possible with mucosa is therefore advisable. Popliteal pterygium syndrome (PPS), as part of a spectrum of disorders associated with mutations in IRF6 [1, 2], is characterized by significant variability in the severity of cleft palate. In severe cases, the mucosa of the hard or short palate might be folded and be lacking. For bilateral cleft lip and palate (BCLP) patients having tissue defects with PPS, we devised a submucosal dissection with periosteotomy to stretch the folded mucoperiosteum by incising the neck of teeth on the hard palate. The present case report describes this new procedure of submucosal dissection to close the folded mucoperiosteum for BCLP with PPS.
Case report
A female infant diagnosed with bilateral cleft lip on prenatal ultrasound was born weighing 3032 g at 40 weeks of gestation. She was transferred to the neonatal intensive care unit and intubated for respiratory distress. Postnatal IRF6 mutation analysis demonstrated NM_006147:exon4:c.C250G:p.R84G, confirming the diagnosis of PPS. Physical examination showed bilateral web of the bottom of the knees and bilateral syndactyly, BCLP, fistulas of the lower lip, and bilateral congenital cords between the maxilla and mandible causing syngnathia with trismus (maximum mouth opening: 5 mm) (Fig. 1A, B). Trismus improved by 30 mm after cutting the cords (maximum mouth opening: 35 mm), allowing the patient to achieve oral intake (Fig. 1C, D). Moreover, the oral mucosa appeared to be folded on the hard palate, and the short soft palate was classified as Randall type III in which the distal tips of one or both uvulae do not even reach as far as the adenoids (Fig. 2A) [3].
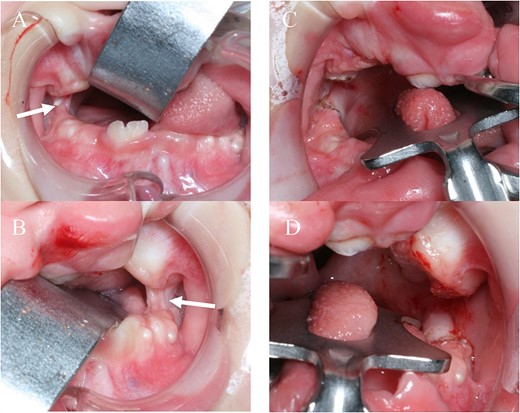
A, B: before release surgery, syngnathia is seen on both sides (white arrow); C, D: after surgery, syngnathia is released on both sides.
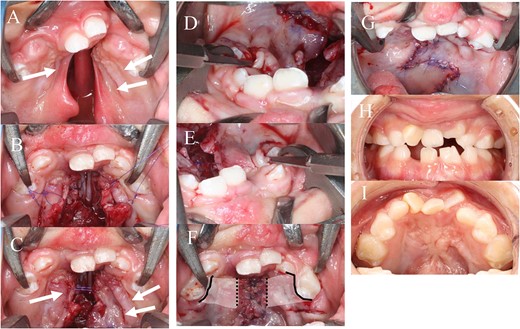
A: BCLP and short soft palate (white arrow: folded oral mucosa); B: after closure on the nasal side; C: the folded oral mucoperiosteum does not extend far enough to allow closure of the cleft palate and so is not closed directly; D, E: submucosal dissection with periosteotomy by a small blade from the cervical region of the teeth; F: the oral mucosa is closed after submucosal dissection; white area: range of submucosal dissection; black line: cervical incision; black dotted line: periosteotomy on the oral hard palate; G: after closure of the soft palate by DOZP; H, I: 6 years after surgery.
Surgical technique
Cheiloplasty was performed at 6 months of age, followed by palatoplasty with submucosal dissection of the hard palate and double opposing Z-plasty (DOZP) of the soft palate at 2 years of age [4]. The nasal mucosa on the hard palate became stretchable by elevating the mucosa on the hard palate from the bone surface, resulting in direct closure (Fig. 2B). However, the oral mucosa with folded mucoperiosteum as a manifestation of popliteal pterygium could not be closed directly (Fig. 2C). This was because the mucoperiosteum of the hard palate lacked tissue and formed folds, as a characteristic of PPS. A small blade (Beaver™; Beaver-Visitec International inc, MA, USA) was inserted into the submucosa from the neck of the deciduous teeth on both sides to perform submucosal dissection with periosteotomy under the folded mucosa by blind manipulation (Fig. 2D, E). The length of the incision on the neck of the teeth was ~2 cm from the deciduous canine to the deciduous molar (Fig. 2F and Fig. 3). Submucosal dissection was performed with attention to the greater palatine neurovascular bundle. After the procedure, the folded cleft mucosa of the hard palate was released, extended, and then closed directly with periosteum. DOZP was performed to close the soft palate (Fig. 2G). As of 6 years after surgery, the palate remained closed and orthodontic treatment was initiated, and facial appearance was improved (Fig. 2H, I and Fig. 4).
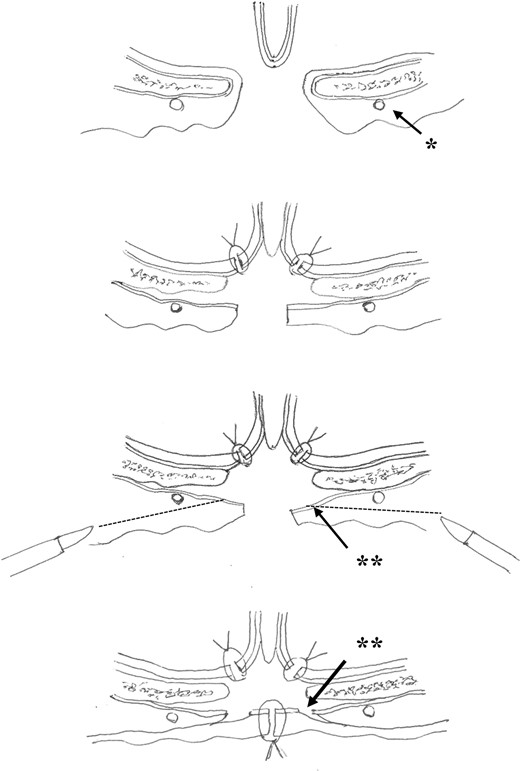
Illustration of the procedure on cross-section of the hard palate (arrowhead*: palatine artery; arrowhead**: periosteotomy; dotted line: submucosal dissection).
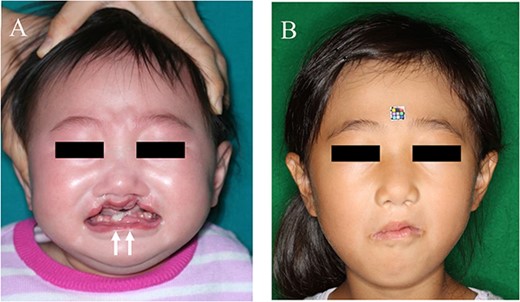
Facial appearance. A: preoperatively, the patient shows incomplete BCLP with fistulas of the lower lip (white arrows); B: 6 years after surgery.
Discussion
PPS is part of a spectrum of disorders associated with mutations in IRF6. The syndrome was first described in 1869, and the term was coined in 1968. PPS is characterized by autosomal-dominant inheritance, significant variability in severity, and related phenotypic features [1, 2]. Characteristic features associated with the craniofacial region, such as cleft palate and syngnathia, include difficulty with reconstruction, limited jaw excursion, and difficulties with breathing and feeding [1]. We described the case of a PPS patient who had syngnathia as well as BCLP with folded oral mucoperiosteum. This patient, who originally showed tissue loss with folded mucosa on the hard palate, and Randall type III soft palate, represented quite a severe case warranting surgical treatment. For these cases, we developed submucosal dissection with periosteotomy, allowing us to stretch the mucoperiosteum and close the cleft on the hard palate. Advantages of this procedure include the avoidance of sheet or areal scars that would occur after lateral incision on the hard palate, as the mucoperiosteum is closed directly. Although lateral incisions and release with DOZP would have been possible to obtain closure of the oral mucosa, lateral incisions would be likely to result in sheet or areal scars and might have caused maxillary retraction. The cervical incision might leave less scarring than lateral incisions and minimized maxillary retraction.
Meanwhile, the possibility of damaging the palatine artery during dissection represents a disadvantage of this method. Since the artery runs close to the periosteum, dissection should be performed in the superficial layer of the mucosa, as close as possible to the mucosal epithelium to avoid arterial damage. Furthermore, incision of the periosteum and stretching of the hard palate resulted in periosteal defect. Despite these disadvantages, the present approach appeared superior to other techniques for the hard palate, considering maxillary retraction. Submucosal dissection with periosteotomy would be useful to extend and close the mucosa for wide cleft cases as well as PPS. In all cases, careful follow-up is needed until the patient reaches adulthood, to monitor speech outcomes and maxillary growth.
Conclusion
We developed submucosal dissection with periosteotomy to close the folded mucosa in BCLP patients with PPS. This technique could be applicable for patients with wide cleft palate.
Conflict of interest statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Data availability
Data available on request from the authors.



