-
PDF
- Split View
-
Views
-
Cite
Cite
Mauricio Fabian Palacios, Alex Guachilema Ribadeneira, Sandra Morocho Imbacuan, Andrea Lisintuña Cisneros, Andrea Daniela Basantes, Colonic lipoma of the hepatic flexure causing invagination in an adult, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac440, https://doi.org/10.1093/jscr/rjac440
Close - Share Icon Share
Abstract
Intussusception is a rare condition in adults that can lead to intestinal obstruction due to malignant or benign lesions in the wall of the colon. Among the benign causes, lipomas are adipose tissue tumors that are most frequently located in the ascending colon. Invagination is characterized by nonspecific symptoms and normal laboratory test results. The exact point of invagination can be detected using advanced imaging studies such as abdominal computed tomography and colonoscopy. Invagination is treated surgically. Here, we presented the case of a female patient with colo-colonic invagination caused by a large lipoma diagnosed by computed tomography who underwent right hemicolectomy with primary ileocolonic anastomosis.
INTRODUCTION
Colonic intussusception is uncommon in adults, accounting for 1% of intestinal obstructions. Although it can have a benign etiology, most cases are caused by malignant lesions, which are found in up to 65% of cases. Colonic lipomas are an extremely rare cause of invagination [1]. The most frequent location is the ascending colon (45%), and tumors larger than 2 cm are associated with a high risk of invagination. The symptoms are nonspecific, and the lead point causing invagination is usually detected using advanced imaging studies.
CASE PRESENTATION
We present the case of a 56-year-old woman with a history of laparoscopic cholecystectomy and arterial hypertension under treatment; the patient had a polyp at the level of the hepatic flexure of the colon diagnosed 5 months before the presentation. She presented to our center with a 4-day history of colicky abdominal pain of low intensity that increased gradually. The pain was mesogastric and radiated to the left hemiabdomen and was accompanied with a sensation of an abdominal mass. On physical examination, vital signs were within the normal range with no abdominal distension. The patient showed tenderness in the mesogastrium and right hypochondrium; a mass was palpable in the mesogastrium with slight pain on palpation and no flatulence. Laboratory analysis showed a leukocyte count of 12 300 × 103/μl. Abdominal tomography showed colo-colonic invaginations involving the hepatic flexure and transverse colon (Fig. 1).
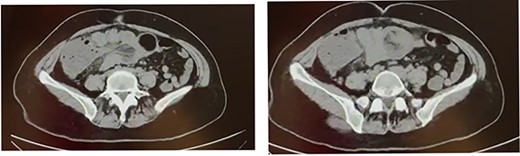
Computed tomography scan shows colo-colonic invagination with the ‘target sign’ or ‘doughnut sing’.
The patient was prepared for laparotomy considering the intussusception involving the ascending colon and hepatic flexure up to the middle of the transverse colon with wall edema and hypoperfusion areas that could not be reduced manually (Fig. 2A and B). The patient underwent right hemicolectomy with ileotransverse anastomosis and was subsequently transferred to the recovery room. The ERAS protocol was applied, with food tolerated after 24 hours, and the patient was discharged on Day 4. The intact sample was sent for pathology.
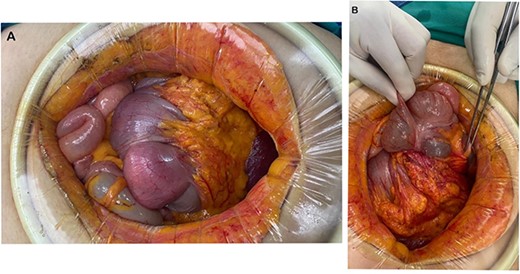
(A) The presence of an invaginating mass in the colon. (B) Colo-colonic intussusception involving the ascending colon, hepatic flexure and transverse colon.
The histopathology results reported a segment of the colon measuring 29 cm. A submucosal lipoma measuring 6 cm in the largest axis was present at the distal segment and occupied 90% of the lumen of the colon; it was characterized by yellow tissue of adipose nature that was continuous with pericolonic adipose tissue. The results of immunohistochemistry were negative for Mdm2 and Ki67 (Fig. 3).
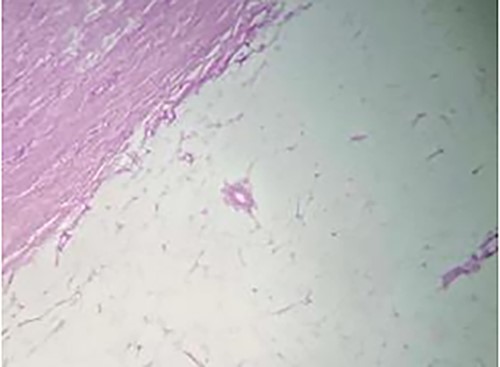
Histopathology results showing an expansive growth pattern, with invasion of the muscularis propria and serosa and extension towards the pericolonic adipose tissue. Immunohistochemical results were negative for MDM2 and Ki67.
DISCUSSION
Invagination is rare in adults, accounting for 1–5% of all intestinal obstructions [1, 2]. It is more frequent in children. In this condition, a proximal segment of the colon invades an adjacent distal segment. Although the underlying mechanism in adults is not entirely clear, secondary intestinal invagination is believed to be triggered by a pathological lesion of the intestinal wall that alters the normal peristaltic activity, which thus becomes a lead point of invagination of one intestinal segment into another one [3].
Primary invagination occurs in the absence of a point of invagination and is more common in children; the small intestine is most frequently affected. In contrast, secondary invagination arises from a lesion that acts as the point of invagination.
There are different types of invagination as follows:
Enteroenteric, which affects only the small intestine.
Colo-colonic, which affects only the large intestine.
Ileocolic, which involves the terminal ileum and ascending colon.
Ileocecal, in which the ileocecal valve is the lead point.
Colo-colonic intussusception is the most common type in adults, accounting for 17% of all intestinal invaginations in adults [1–4].
There are several possible causes as follows: benign and malignant lesions, polyps, adenomas, lipomas, adhesions, inflammatory diseases, diverticulum, endometriosis and previous anastomosis. Approximately 60–65% of cases are caused by a malignancy.
Colonic lipomas are benign adipose tumors that occur infrequently and are characterized by slow growth. They were first described by Bauer in 1757. Colonic lipoma is the third most frequent benign tumor of the intestine after hyperplastic and adenomatous polyps, and it has an incidence rate of 0.2–4.4%. It is more common in women aged 40–70 years, and it presents as a solitary mass or as multiple masses in up to 25% of cases. The most frequent location is the right colon in 61% of cases, followed by other locations including the transverse colon with flexures (15.5%), descending colon (20.1%), sigmoid colon and rectum (3.4%) [1, 5]. It has a variable size, and masses of up to 30 cm have been reported. Approximately 90% of lipomas are submucosal, which is consistent with the pathology results of the present case. They are generally asymptomatic and are detected incidentally during imaging tests, colonoscopy or surgery. Lipomas larger than 2 cm are usually associated with symptoms and should be removed surgically because of the risk of invagination [1, 5].
The main symptom is abdominal pain in 83% of cases, in addition to bleeding and changes in bowel habits particularly constipation [1, 5, 6]. According to Menegon Tasselli et al., abdominal tenderness is the most frequent clinical sign in 37% of cases, followed by abdominal distension in 16%. Laboratory test results are normal in 61% of cases. Preoperative diagnosis is difficult, and diagnostic imaging studies include radiography, abdominal ultrasound, tomography and colonoscopy [6]. The most commonly used method is abdominal computed tomography, which has a sensitivity of 87% and specificity of 100%; it detects intestinal invagination as a lesion with the typical appearance known as the ‘Dance sign’ or a soft tissue ‘sausage-shaped’ mass. Invagination is confirmed by colonoscopy, which can also detect the lead point [3, 6].
The treatment of intussusception in adults is almost always surgical. The technique used depends on various factors such as the size of the lipoma, the location, the severity of inflammation and the presence or absence of complications [1]. For submucosal lipomas smaller than 2 cm, extraction by endoscopy with electrocautery is a valid option. Determining whether the intussusception is caused by a benign or malignant lesion is essential because this information affects the extent of resection [7].
There is no consensus regarding whether the intussusception should be reduced before resection, and several authors do not recommend barium reduction in the adult population [7, 8].
In conclusion, colonic intussusception is rare in adults. Submucosal colonic lipomas, which are among the benign causes, are confirmed by histopathology. The diagnosis of this condition is challenging for the surgeon because it presents with nonspecific symptoms. Intussusception is detected by abdominal computed tomography and colonoscopy, and the treatment in the majority of cases is surgical.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



